Artificial intelligence (AI) has transformed every industry worldwide, including dentistry. While ever more dental professionals attempt to adopt AI in studies and daily routines, most AI researchers come from engineering fields, leading to potential knowledge gaps in these techniques. This article aims to bridge that gap by presenting AI’s fundamental principles and their applications to clinicians. With minimum essential engineering knowledge, the article will help dentists recognize the basic mechanisms, benefits, and limitations associated with modern AI. Thereupon, clinicians can harness the power of this technological tool to enhance their daily practices and research effectively while avoiding potential pitfalls.
AI applications in dentistry
After understanding the nature of AI as a mathematical approach to analyzing vast amounts of data and the underlying relationships, it is easier to recognize real-life applications for AI. AI has made its mark in numerous dentistry applications, supporting clinical practice and research endeavors. The significant categories of application include:
Automation of repetitive tasks
Automating administrative tasks is a prominent and immediate application of AI in dentistry. AI-powered software can seamlessly manage scheduling, send patient reminders, handle billing, and answer common patient inquiries. This reduces the load on administrative staff, boosts overall efficiency, and allows dental professionals to devote more attention to direct patient care.
Clinical decision support systems/expert systems
AI can support clinicians during their decision-making process. These advanced systems can help analyze patient records and clinical data, aligning them with established guidelines to provide sound recommendations for diagnoses or treatments. For instance, a program can be designed to categorize a patient’s periodontal disease status based on the evaluation of diagnostic factors and clinical examinations (Farhadian et al., 2020). This enhances diagnostic efficiency and alleviates uncertainties, especially for young or less experienced dentists.
Imaging analysis
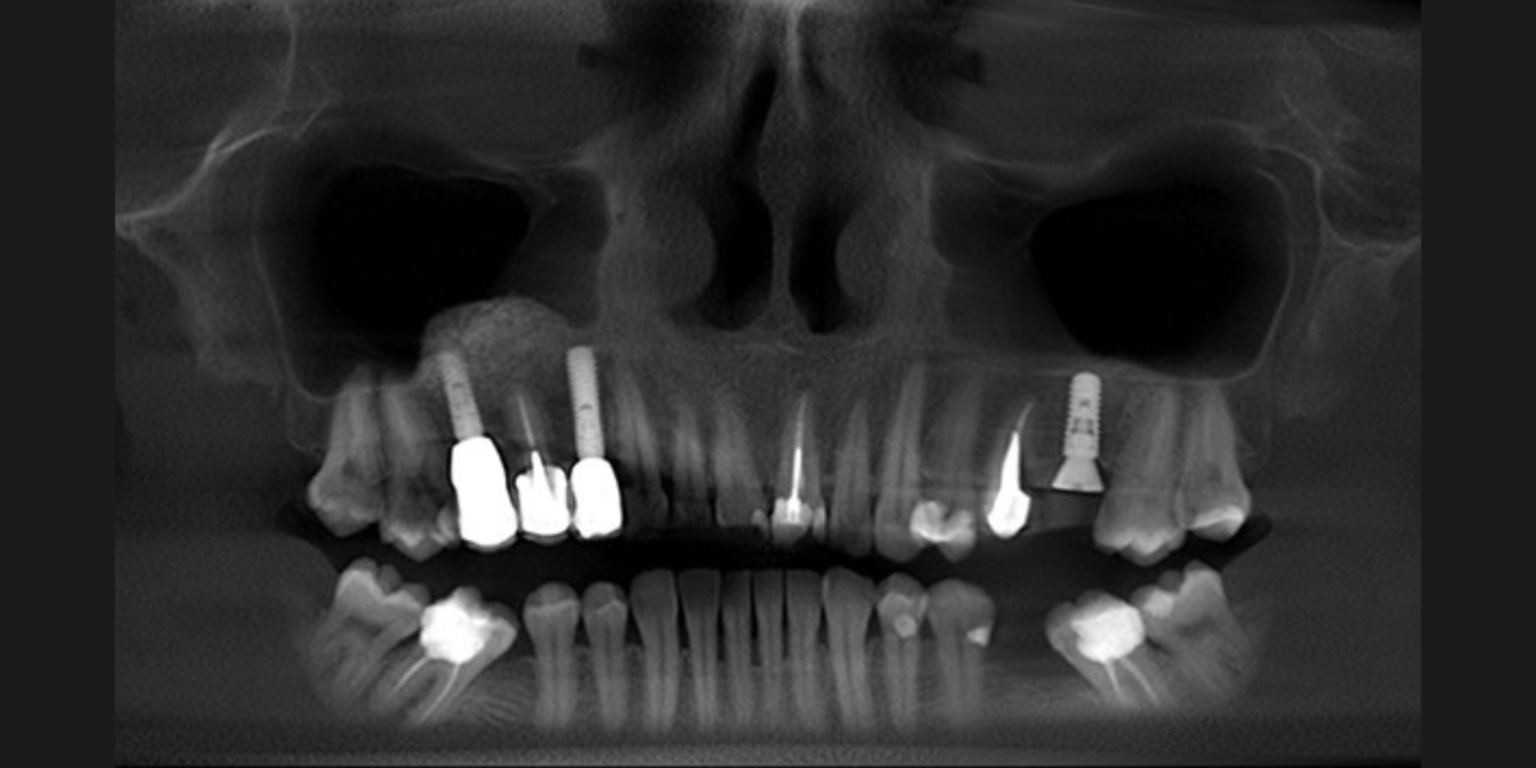
Dental imaging has emerged as a significant area of interest where AI is exhibiting considerable potential. AI algorithms, particularly deep learning, have been employed in analyzing radiographs and other clinical images to assist in detecting and diagnosing various oral diseases (Muresan et al., 2020). It is worth noting that the applications of AI in imaging can be integrated with other purposes discussed in this section. For example, AI has been adopted in research to identify conditions like caries, periodontal disease, and pathological patterns. AI also shows potential in analyzing 3D images, enhancing the planning process for procedures like implants or orthognathic surgeries (Xiao et al., 2021).
Predictive analytics for treatment outcomes/prognoses
AI can leverage predictive analytics to assist with treatment planning. For example, given a patient’s orthodontic records, AI can help analyze a spectrum of clinical data. This includes lateral cephalometric analyses, determinations of vertebra maturation degree, skeletal classification, and more (Mohammad-Rahimi et al., 2021). Several approaches have also been proposed to predict the need for tooth extractions and orthognathic surgeries (Suhail et al. 2020; Kim et al. 2021).
Surgery/prosthesis planning
AI is making inroads into pre-surgical planning procedures, particularly with 3D imaging software. For example, AI can indicate significant structures, such as the inferior alveolar nerve in the mandible, or optimize the design of an implant or surgical stent (Jaskari et al., 2020; Kurt Bayrakdar et al. 2021). AI can also help analyze and design dental prostheses (Hwang et al. 2018) such as crowns, bridges, and removable dentures. While AI can enhance or even eliminate specific steps involving repetitive image processing, such as defining the borders and locations of targeted objects, more intricate analyses and optimizations generally still need dentist oversight for validation.
Research and education
The nature of AI as a mathematical approach makes it align seamlessly with the academic dimension of dentistry, especially in statistical analyses. AI is valuable for parsing large datasets to correlate the relationships between the various factors shaping oral health and disease. Furthermore, on the basis of extensive data, AI holds the potential to spotlight and decode previously elusive insights into dentistry that remain undiscovered.
All the AI applications in dentistry outlined hold the potential to enhance patient outcomes, streamline clinical workflows, and increase the precision and efficiency of numerous tasks. Nevertheless, as with any technology, AI presents challenges that warrant careful deliberation that will be discussed in the following section.
Limitation
There are plenty of articles emphasizing the benefits and strengths of AI but it is also crucial to recognize its limitations in order to avoid potentially misleading content and undesirable consequences. This section will list several significant considerations when evaluating AI research or its applications in practice
The importance of quality data
The quality of the input data determines the quality of the outcome of an algorithm (Jain et al. 2020). A well-known phrase in data science and machine learning is “garbage in, garbage out.” If the input data is flawed, biased, noisy, or of poor quality (“garbage in”), the whole algorithm is trained on these suboptimal data. Therefore, the output data will mirror these imperfections and result in being flawed, biased, noisy, or of poor quality (“garbage out”).
This simple but important concept can be easily overlooked in many studies, as multiple factors can compromise data quality. Common influencing factors include but are not limited to, ambiguous diagnostic definitions, labels provided by inexperienced clinicians, and unrepresentative or biased datasets skewed toward particular patient populations or distribution.
For example, a common commercial use of AI in dental radiography is to detect dental caries, periapical lesions, and marginal bone loss on panoramic radiographs. However, panoramic radiography has already proven unsuitable for diagnosis because of its low spatial resolution, distortion, and superimposition (Vandenberghe et al. 2010). Even seasoned clinicians need help providing precise diagnostic labels in such scenarios. Thus, the AI models trained on these potentially flawed labels may also inherit these inaccuracies, even if their diagnostic abilities match human experts. With this in mind, however, more reliable outcomes can be achieved using higher-quality data sources, such as intraoral radiographs or cone-beam CT, as a reference for model training.
Reliability of AI-processed information
Generative AI is gaining considerable attention in AI nowadays, including text-related, image-related, or a combination of both. Applications for the general public, such as Chat-GPT, Midjourney, and other AI image enhancers, have seen rapid adoption. Besides general purposes, machine-learning engineers have been trying to address challenges in medical imaging with these innovative techniques.
In this regard, a popular focus is on improving image quality and resolution. Various algorithmic attempts have been employed to approximate adjustments to eliminate noise or artifacts. However, the underlying mathematics of these approaches should be scrutinized. While post-processed images usually offer enhanced visual clarity, their adoption for diagnostic purposes can be contentious.
Post-processing algorithmic approaches, such as metal artifact reduction (MAR) and image upscaling, have been employed to enhance visual image quality by noise/artifact elimination and detail enhancement. After algorithmic refinement, the end images can appear natural and more defined for visualization while actually containing inaccuracies, distortion, and irretrievable information loss due to the estimation process (Coelho-Silva et al. 2021).
As such, post-processed images are usually not ideal for diagnostic purposes. There can be concerns with the authenticity of anatomical details in regions modified with estimation algorithms. For instance, several studies have suggested an adverse effect of MAR algorithms when detecting root fractures in cone-beam CT images in endodontically-treated teeth or around metal post areas (Bechara et al. 2013; Bezerra et al. 2015). One suggested mitigation is the careful evaluation of original and processed images during the examinations.
Interpretability of AI models
The interpretability or explainability in AI, especially deep learning models, is an ongoing challenge that data scientists are keen to address. In essence, interpretability refers to how well the inner mechanism of AI models can be comprehended by human users (Holzinger et al. 2019).
AI models’ inherent complexity and non-linearity enable them to tackle complicated tasks and make predictions. However, the decisions made by these models mainly depend on self-adjusted parameters during training, drawing patterns, and correlations identified in vast datasets. Therefore, these algorithms are often called “black boxes” and do not follow a human-like or intuitive logical way of thinking. This is particularly evident in deep neural networks, which involve a series of interconnected hidden nodes (neurons).
This lack of intuitive explainability can undermine the confidence and trust of its users. When users, including doctors, engineers, or policymakers, need help understanding how an AI system works, they may hesitate to take its recommendations. Sometimes, human experts can sidestep AIs’ decisional mistakes by relying on their judgments. Conversely, in critical situations where AI could offer invaluable insights, this trust deficit can hinder the benefits of incorporating AI assistance.
In terms of interpretability, simpler models are generally easier to explain, although their performance is less ideal than complex non-linear models. As such, there is often a trade-off between accuracy and interpretability in AI models (Luo et al. 2019). In some cases, it may be preferable to forgo a degree of accuracy for a more transparent and understandable model to users.
Ethics, regulation, and data privacy
Potential challenges with AI are not limited to technical aspects but can also extend to ethical, legal, and data privacy concerns (Naik et al. 2022; Zanca et al. 2022). While this article focuses on the technical aspects of AI, it is vital to acknowledge these other concerns when integrating AI into dental research or practice. These topics remain at the forefront of ongoing discussions in various professional associations
Conclusion
While AI offers transformative solutions, dental and medical professionals must be cautious when integrating it into their practice. Dentists should understand the underlying theories and continually update their knowledge to harness the full potential of AI while minimizing the risks and oversights that might compromise optimal patient care.