Introduction
A lack of vertical dimension of alveolar bone at the posterior maxilla is a common challenge in implant dentistry. Usual causes can be the result of a loss of alveolar bone from periodontal destruction, or a pneumatized maxillary sinus, or both. Advancement in material science and nanotechnology allow stronger implant with shorter length to be made. The use of short implant with a length of 8mm or less is commonly utilized in cases of limited vertical space, with promising survival rate comparable to the more standard-length implant (Lemos, Ferro-Alves, Okamoto, Mendonca, & Pellizzer, 2016). In other cases, however, it is impossible to place implant without sinus floor elevation (SFE). Lateral window sinus lift is the classical approach to improve residual bone height, first described over 40 years ago (Boyne & James, 1980). Later development and refinement of surgical instruments and techniques allows us to elevate the sinus floor, to a lesser extent, with predictable result by a transalveolar approach (Pjetursson & Lang, 2014). Both approaches result in implant survival rates comparable to implant placed in normal bone (Jensen & Terheyden, 2009). Clinical decision of the respective surgical approaches is mainly based on anatomical parameters include subantral bone height, sinus width, sinus floor anatomy, the presence of sinus septum, etc (Stacchi et al., 2020).
Lateral window SFE is a reliable and clinically well-documented technique, which is indicative when residual crestal bone height is less than 5mm. It is used as a staged augmentation procedure to increase crestal bone height before implant placement. Sometimes, when residual bone volume allows adequate primary stability of a dental implant, simultaneous SFE with implant placement could be considered. Nevertheless, SFE could be surgically demanding, especially for young clinicians. One crucial step to success is to create a proper access to the part of the sinus where grafting is needed.
The “optimal” window
A lateral window opening with appropriate size at a proper location facilitates a smooth sinus floor elevation. A couple of aspects dictate how an “optimum” window include:
Window size and location
Size of a lateral window should be large enough to allow proper visualization of the surgical site, access of surgical instrument for safe lifting of the Schneidarian membrane and deliver of the bone graft with ease. On the other hand, it should not be too large to jeopardize the retention of grafting material and reduce the amount of vital bone wall for its osteogenic power. Depends on experience, some dental surgeons could perform the same surgery efficiently and effectively with a smaller sized window. Generally, it is recommended to create a lateral window measure at least 5mm vertically and 8 to 10mm horizontally if single implant is to be placed. It was suggested the ideal position of the window to be as mesial and as low as possible in relation to the maxillary sinus (Zaniol & Zaniol, 2017).
Bone wall thickness & convexity
Sinus bone wall can be paper-thin. So much so it could appear bluish when a flap is raised, allowing clinicians to know exactly where the sinus is located. It is the time when we must be cautious because any sharp cut could go beyond the point and lacerate the sinus membrane. It is however a surgical advantage if the window bone rim is within a certain thickness, i.e. within 1mm. Thicker bone wall may increase the time of cutting and reduce the visibility when approaching the sinus membrane. If the window is small, positioning of sinus curettes may be difficult. Besides, some sinus wall appears flatter in the outlook and some with more convexity, as it continues from the zygomatic buttress. It could be hard to lift a window at a convex slope, which require more skillful approach to avoid damaging the membrane.
Neighbouring teeth
Roots of the neighbouring teeth may present their way with different curvature and length. Sometimes they may be proximal to the anterior wall of the sinus, and close to the superficial cortex of the alveolar bone proper. Damage to adjacent teeth during the surgery may result in root resorption or pulpal necrosis, especially when the neurovascular supply to the dental pulp is interrupted. Keeping a good 2mm distance away from them is essential to avoid unwanted post operative complications.
Sinus septum
Sinus septum, which presence in roughly 30% of patients, is a known risk factor of sinus membrane perforation(Testori, Weinstein, Taschieri, & Wallace, 2019). Different surgical approaches were discussed in the literature to cope with this problem. For a fully developed septum separating the maxillary sinus into an anterior and a posterior zone, two windows could be prepared on either side of the septum. Sinus floor elevation could then be performed separately for the two compartments. On the other hand, for a relatively small septum, a larger window encompassing the septum could be performed. By removing the sinus bone wall, the lining membrane could then be elevated from both sides of the septum.
Arterial anastomosis
An accidental cut into an artery near the maxillary sinus may not result in life-threatening event, but it certainly impairs surgical site visibility and increases difficulty in management of the surgery. Blood supply of the maxillary sinus comprises of three origins: the infraorbital artery, the posterior lateral nasal artery and the posterior superior alveolar artery (PSAA), with their intercommunicating anastomoses (Rosano, Taschieri, Gaudy, & Del Fabbro, 2009). Intraosseous and extraosseous anastomoses run along the lateral wall of the sinus, which the intraosseous vessels usually situates at a more crestal position than the extraosseous counterpart (Solar et al., 1999). An intraosseous anastomosis is present in almost 100% of the patients but only visible on cone-beam CT imaging in 50% of the cases. An anastomosis of the PSAA running across the lateral wall of the maxillary sinus is a potential thread. It was reported to be present in 20% of the normally positioned antrostomy area, which possesses potential risk of intraoperative haemorrhage (Elian, Wallace, Cho, Jalbout, & Froum, 2005).
The concept of guided sinus surgery
All the above-mentioned factors are considered. The outcome is a desired area that a lateral window would be created. In the era when cone-beam CT was not commonly available, much was relied on the anatomical knowledge and surgical experience of the operator. Extraoral and intraoral X-ray provided information about the size of the sinus in relation to the neighbouring vital structures. Visual inspection and percussion feedback on the bony surface during the surgery often gave us hints as well. Moreover, measurement could be performed from neighbouring teeth and the alveolar crest, to determine where our desired window should be. The ideal location for the lateral window was approximated. Once a window was created, adjustment could be made by incremental enlargement in order to reach the preferred size and shape.
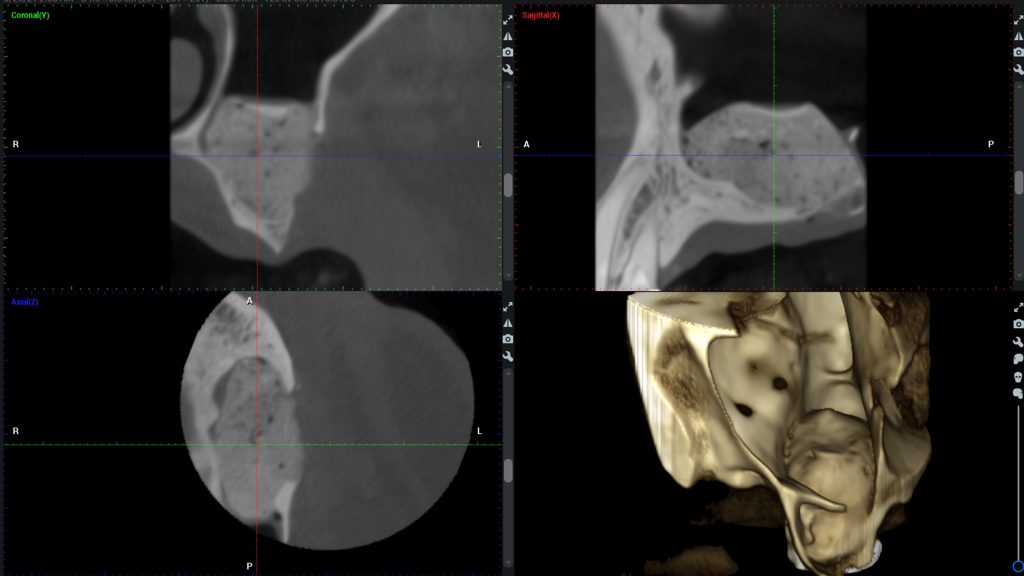
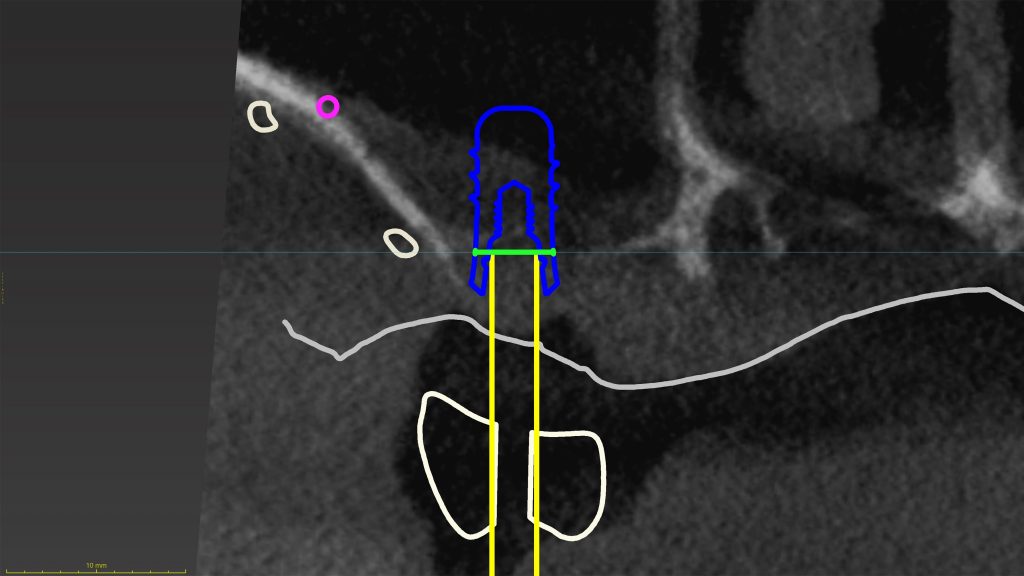
With technological advancement, the use of cone-beam CT imaging allows us to perform an even more realistic surgical planning than one can ever imagine. We are able to see, in different planes and in three dimensions, how the different anatomical structures related to one and other. Intraosseous blood vessels running along the sinus wall could be identified. In cases of an irregularly shaped sinus, we can design a window which follow the slope of the sinus floor to tailor made our cut. The location and dimension of sinus septum could also be evaluated (Neugebauer et al., 2010). We become knowing so well, with confidence being accurate, that we want to draw our most desired lateral window in the planning software.
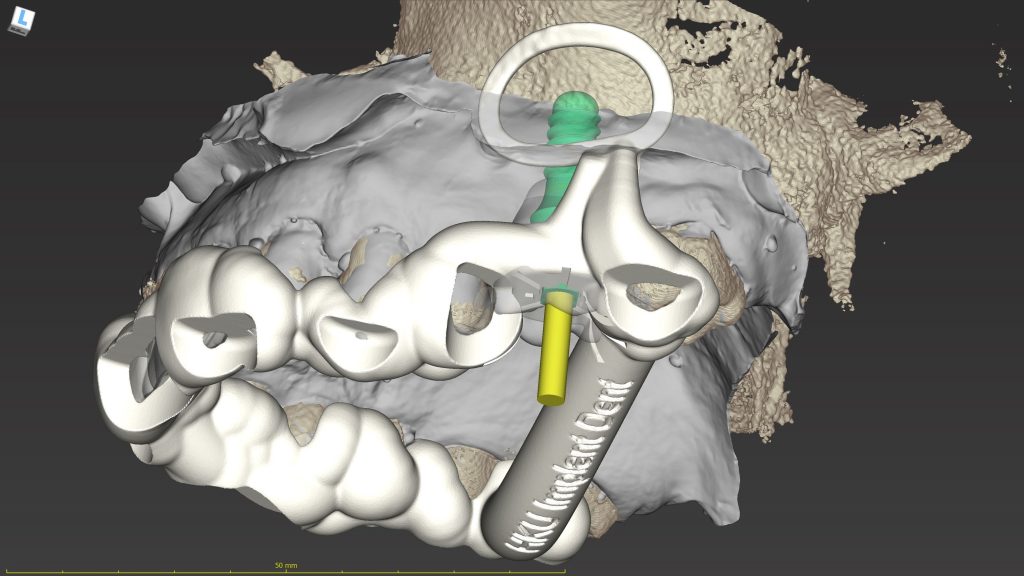
Currently, CAD/CAM technology also allows computer-aided implant surgery (CAIS) being carried out with good precision (Smitkarn, Subbalekha, Mattheos, & Pimkhaokham, 2019; Tahmaseb, Wu, Wismeijer, Coucke, & Evans, 2018). Surgical guide is being fabricated to facilitate implant osteotomy and placement. The same principle can be applied in the creation of a surgical guide for lateral window for sinus floor augmentation (Strbac et al., 2020; Zaniol, Zaniol, Tedesco, & Ravazzolo, 2018).
Clinical application of sinus guide
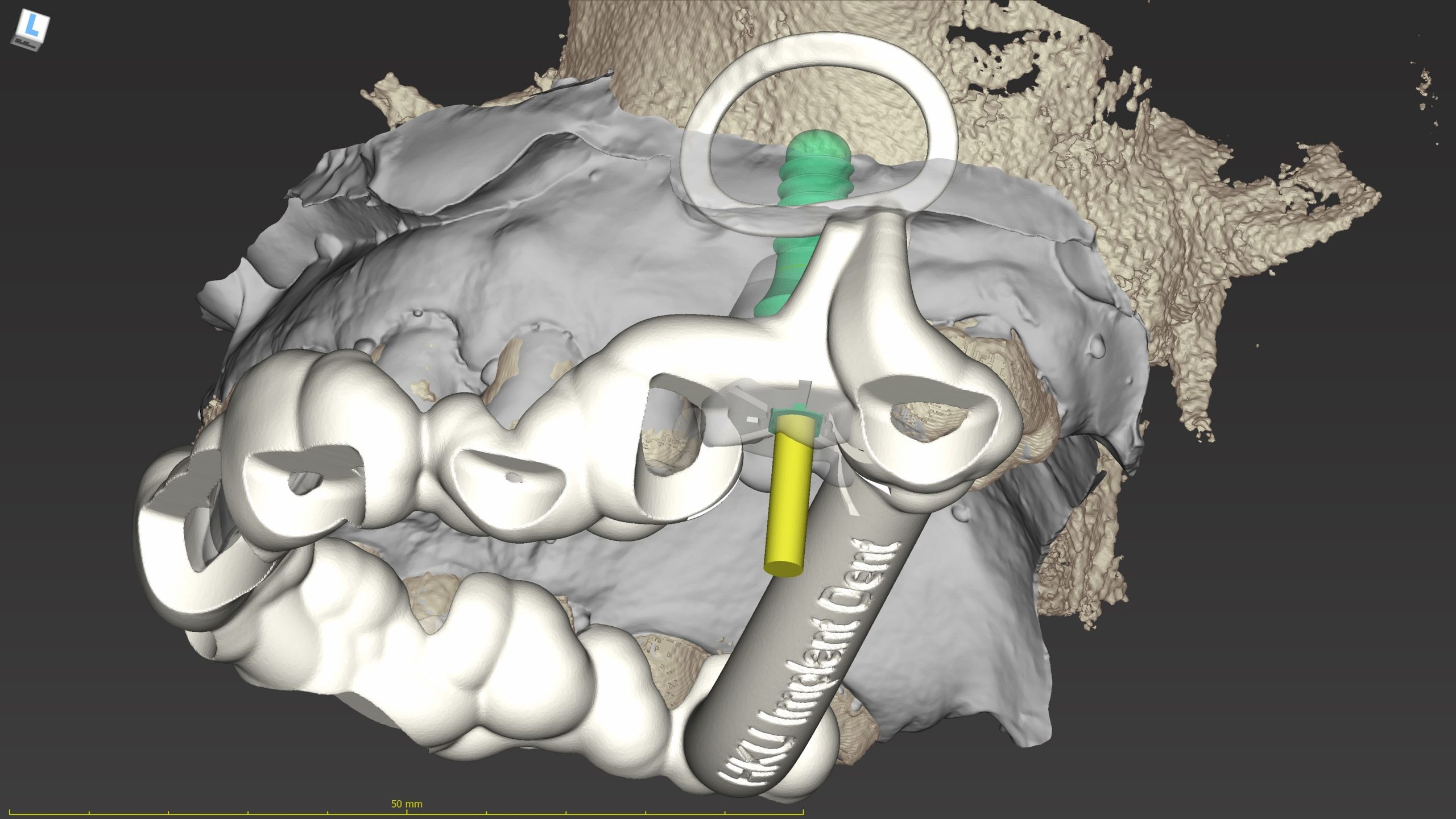
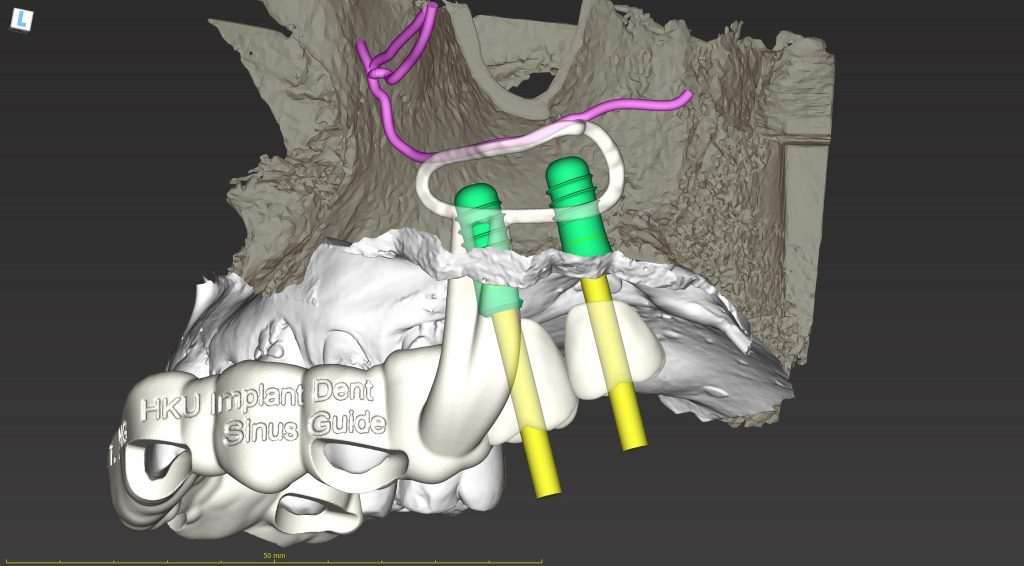
A few cases are used to illustrated how a sinus guide allows an efficient and safe antrostomy to be performed. In the first case, cone-beam CT image, virtual study model and diagnostix wax up model were imported into an implant planning software (coDiagnostiX version 10.2, Dental Wings). The window was designed to stay close to the anterior and inferior border of the maxillary sinus, with sufficient space for instrument to work at the target grafting area.
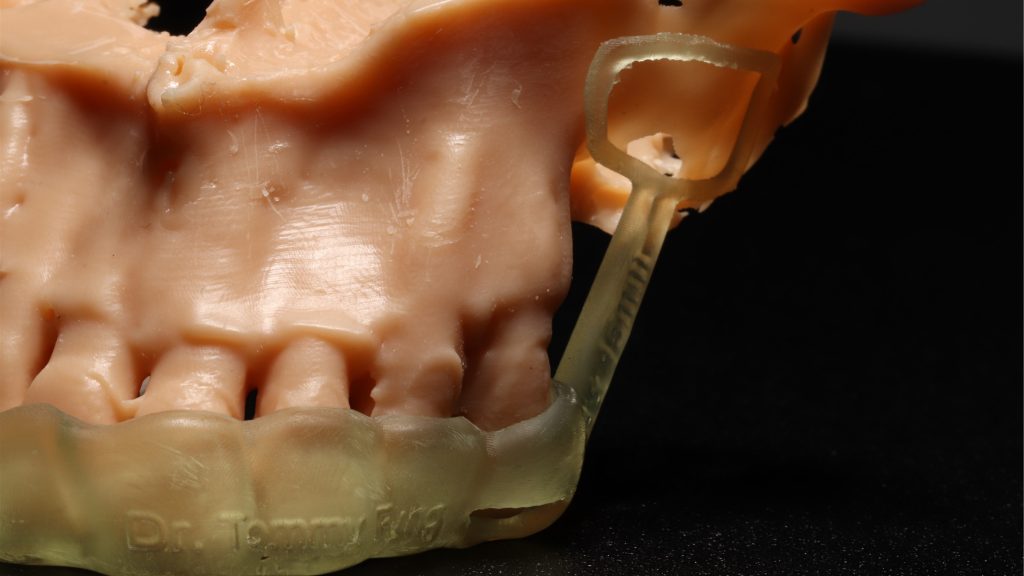
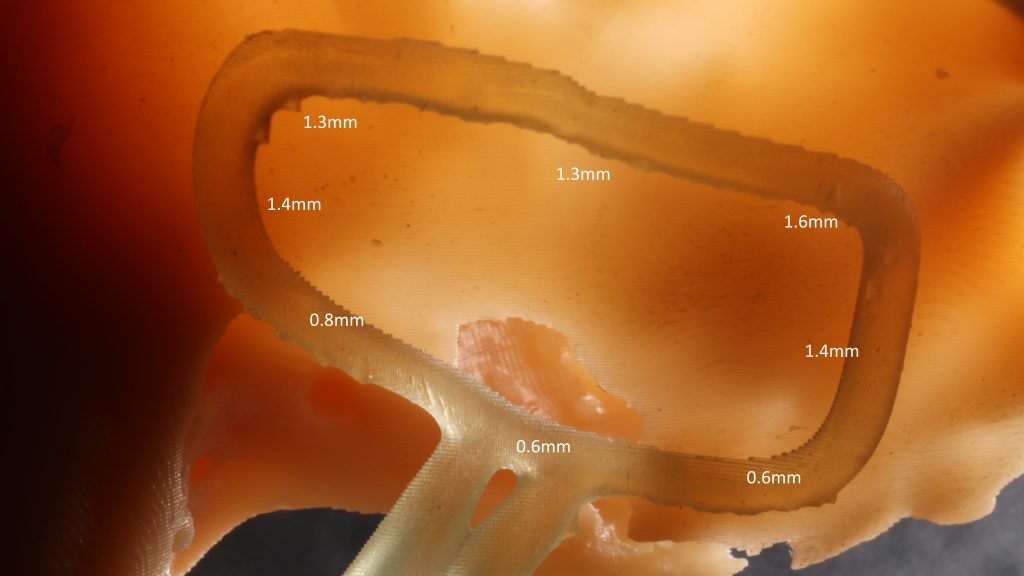
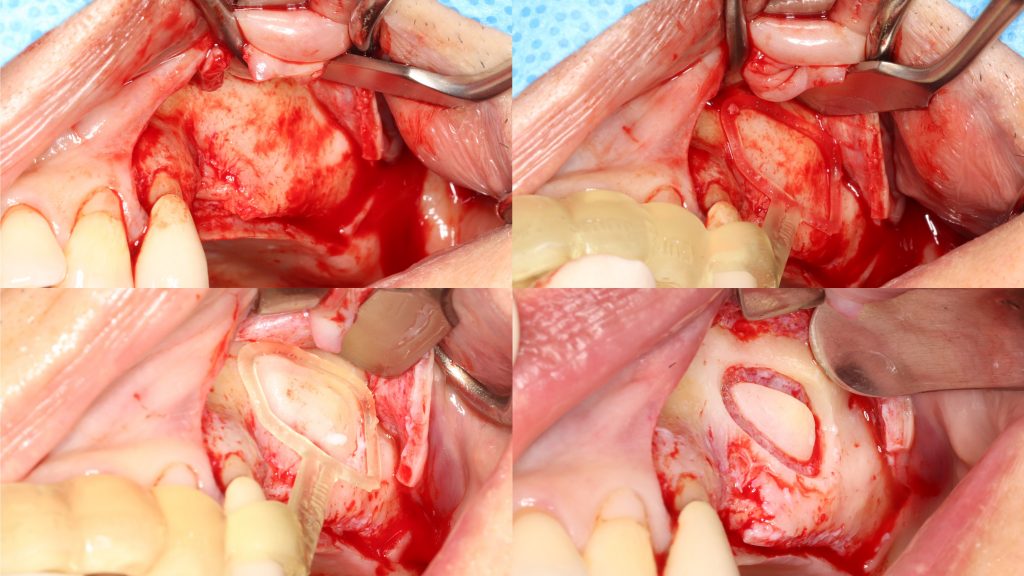
Within the planning software, the cut profile was drawn, considered that a round bur or piezo tip would be running within. So it was designed to be slightly larger than the actual window. By completing the cut profile into a full circle, it gave a complete guidance of the outline of the window. It also suggested the superior extent of the mucoperiosteal flap required to allow adequate exposure for the antrostomy. The dimension of the window guide was set to be an offset of 0.5mm away from bone, window rim width 1.5mm and thickness of 1.0mm. By these parameter, a thin guide was produced to reduce spatial hinderance and allow maximum visibility for the surgery. The actual guide would be flexible rather than rigid due to the slim design. It was not a concern because the guide was not intended to physically guide the instrument. It only served as a reference for the window to be made freehand. The rest of the guide was designed to cover the occlusal surface of all maxillary teeth to provide adequate stability. Inspection windows were created at a couple of occlusal spots to allow verification of proper seating of the surgical guide during use. The subsequent surgery was performed as described with the photos.
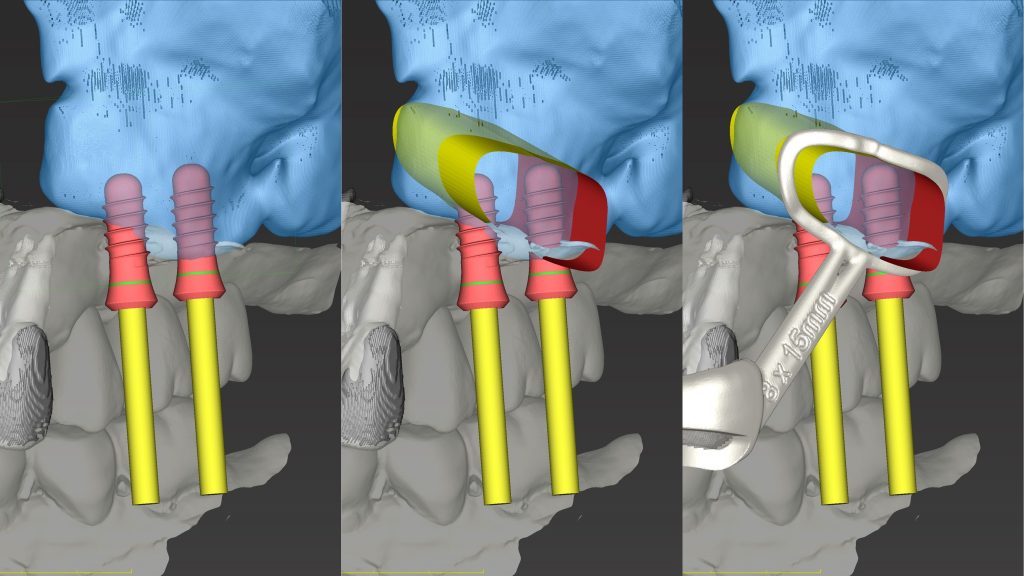
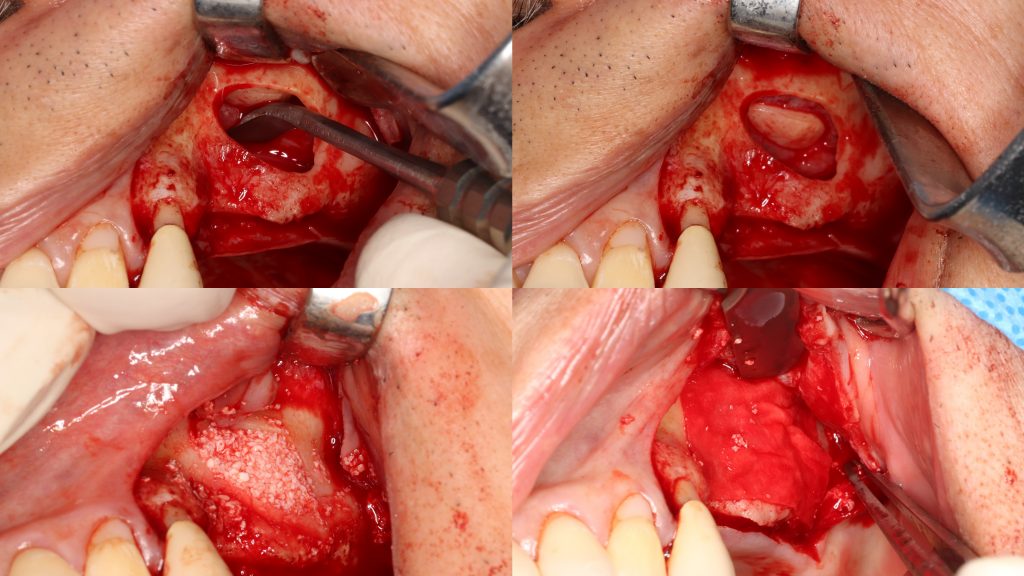
The next example demonstrated a case of similar design. Since residual bone height (4mm) was sufficient for achieving good primary stability of an implant, SFE and implant placement could be performed simultaneously, with a surgical guide incorporating both features, as described by Sun and co-authors (Sun et al., 2020). The surgical plan began with a proper prosthetic set up of the missing tooth, with good alignment within the arch and occlusal loading directly opposite to the mandibular teeth. The implant was virtually placed according to the set up to allow axial loading, screw hole opening at the centre of the occlusal table, and periodontally-friendly emergent profile design. After determination of the correct 3D positioning of the implant, the sinus window was designed to allow easy access to the location which sinus floor elevation and grafting was most needed, with consideration of the anatomical characteristics as mentioned previously. The surgery was performed accordingly.
Another example of a sinus guide, which aimed to denote the position of an anastomotic artery on the sinus wall to provide some form of alert for the clinician, by intentionally overlapping the upper rim of the window guide with the position of the vessel. It was identified on the cone-beam CT that a PSAA anastomosis ran across the sinus wall. After consideration, the sinus window was designed to be inferior to the blood vessel to avoid getting the cut too close to it. With naked eye, an intraosseous vessel is sometimes observed as a dark line running on the bony wall when a full thickness flap is elevated, but a pre-surgical study of the cone-beam CT imaging allows us to visualise it thoroughly. With similar thought, a sinus guide can also be designed to locate the position of a sinus septum, as discussed in the literature (Teixeira, Sakurada, Philippi, & Goncalves, 2021; Wang, Ye, Sun, & Wu, 2021).
Conclusion
When state-of-the-art imaging technique allows us to see beyond the surface anatomy, and that CAD/CAM technology helps transfer our plan into the actual surgical field, the beauty of a surgery is to perform it as designed. With the popularization of more accurate and economical 3D printers, this becomes more convenient than ever. The availability of digital hardware and software opens new possibilities. Their potential use is only limited by our imagination. Precise lateral window opening helps us to avoid some, but not all risks of sinus floor elevation surgery. Pre-surgical planning becomes more demanding, but the reduction in surgery time and improvement in safety benefit our patients, which makes the afford all worth spending.
For more detailed references, check out the following material on the ITI Treatment Guide and ITI Academy:
- ITI Treatment Guide Volume 5: Sinus Floor Elevation Procedures
- ITI Treatment Guide Volume 11: Digital Workflows in Implant Dentistry
- Surgical Planning and Procedures, Principles of Sinus Floor Elevation by Simon Storgard Jensen
- Surgical Planning and Procedures, Lateral Sinus Floor Elevation by Simon Storgard Jensen