Introduction
Achieving long-term esthetic success by replacing missing teeth with dental implants is often challenging for clinicians. Predictable results can only be achieved when an adequate diagnosis and application of the most current scientific evidence are considered. Several variables significantly impact the treatment outcome of fixed implant-supported rehabilitation in the anterior maxilla area, and they entail a comprehensive understanding of the 1) patient, 2) surgical site, 3) tissue biology, 4) surgical protocol, 5) implant design, 6) restorative approach, and 7) maintenance.
This blog article aims to provide colleagues with technical and clinical considerations based on our experience and current scientific evidence to perform an appropriate treatment plan when replacing missing teeth in the esthetic zone with implant-supported restorations.
From tooth extraction to implant loading
Different surgical and prosthodontic protocols applied in oral implantology are directly associated with the long-term outcome of implant-supported restorations (Morton et al., 2018). Therefore, dental implant treatment planning should be assessed before tooth extraction (if the tooth is still present), mainly in the anterior esthetic zone
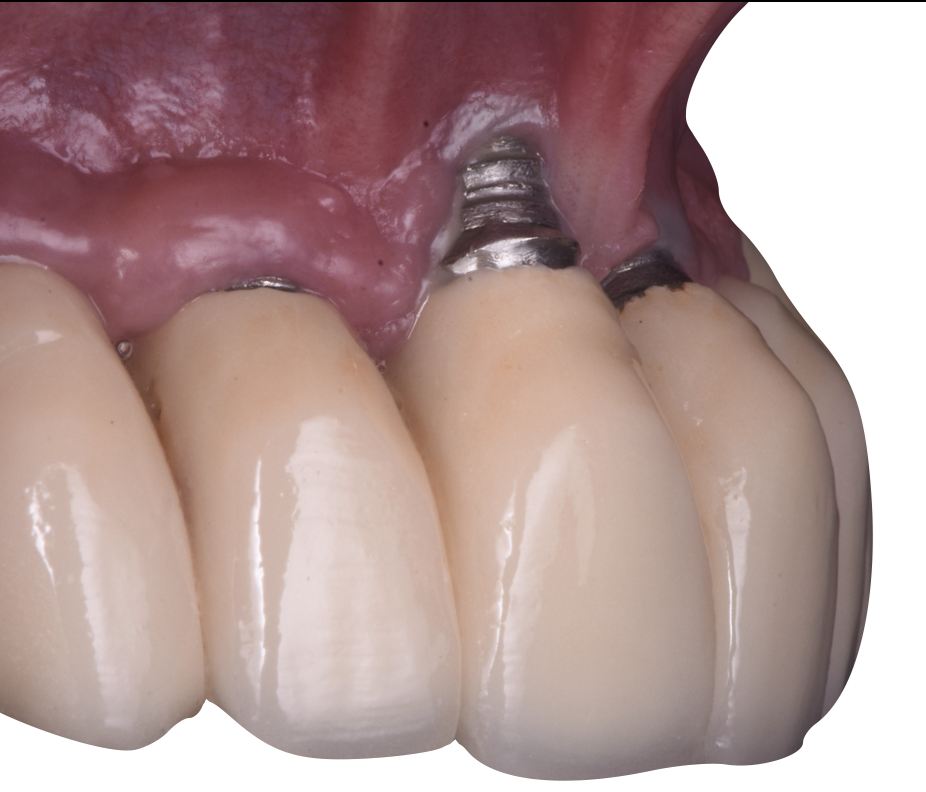
The implant placement and selection of restorative/loading protocol should be based on the aim to achieve predictable long-term hard and soft tissue stability, optimal esthetics, reduced risk for complications, and meeting patient-specific and site-related criteria (Figs 1 – 2).
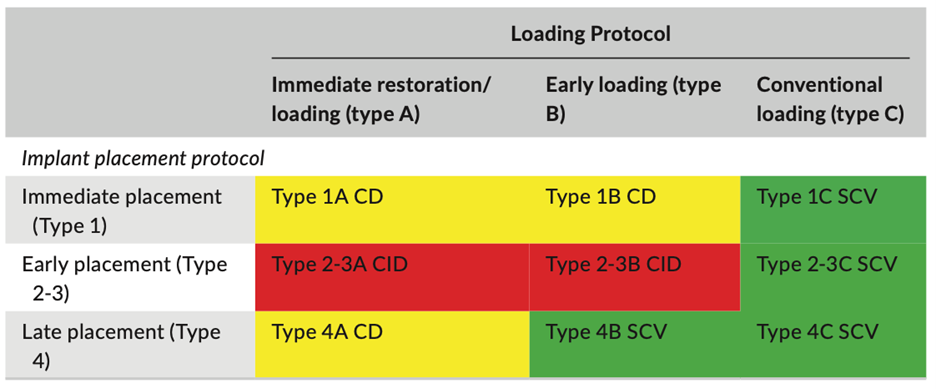
The 6th ITI Consensus Conference reviewed the available evidence for the clinical outcome of fixed implant prostheses treated with different combinations of implant placement and loading protocols (Gallucci et al., 2018).
The possibilities for dental implant placement include the following:
- Immediate implant placement post-extraction
- Early implant placement with soft tissue healing (4 – 8 weeks) or partial bone healing (12 – 16 weeks)
- Implant placement in healed sites
The possibilities for dental implant loading include the following:
A) Immediate loading/provisionalization: Earlier than one week after implant placement
B) Early loading: 1 – 2 months after implant placement
C) Conventional loading: >2 months after implant placement
In the past, implant placement and loading protocols were analyzed separately. However, both are directly related to each other. For instance, high initial insertion torque (“primary stability”) is a requirement for immediate loading. Obtaining high values of initial insertion torque will be more likely on a healed site (“implant placement in healed sites”) than in a post-extraction socket (“immediate implant placement”) since greater mechanical friction occurs.
For this reason, it seems obvious that it is necessary to combine these implant placement and loading categories (1A, 1B, 1C, 2A, 2B, etc.) to arrive at clinical recommendations (Fig. 3).
Some examples and clinical tips based on the current scientific literature are:
Immediate implant placement and loading (Type 1A) (Cosyn et al., 2016, Blanco et al., 2019)
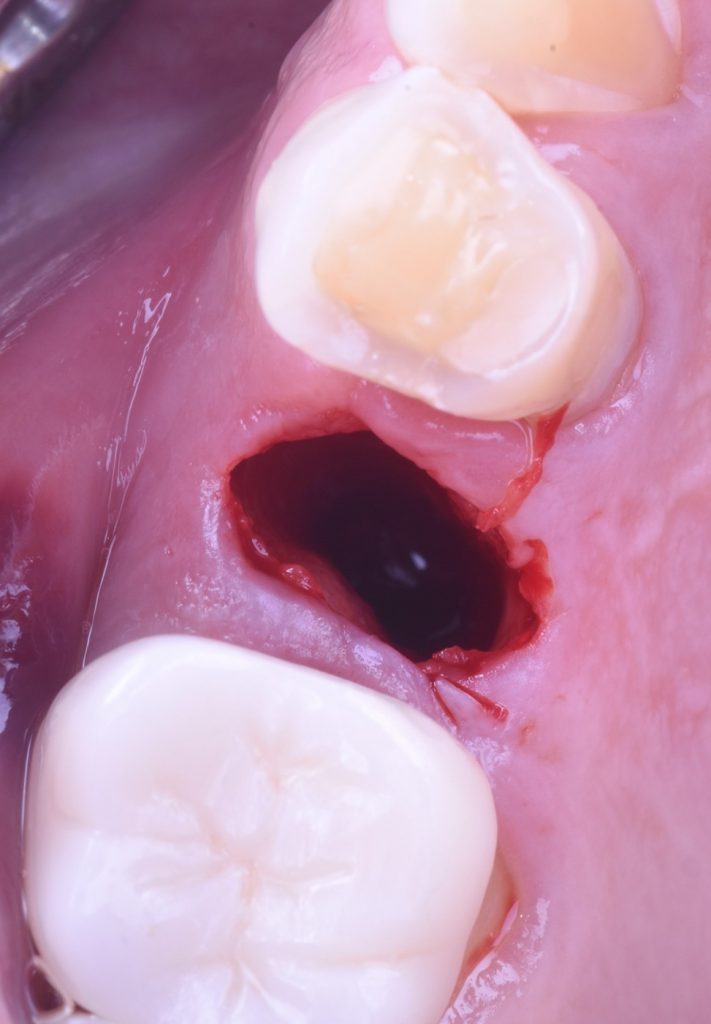
Immediate implant placement with immediate restoration/loading (type 1A) should be considered in particular when:
- There are patient-centered requirements (e.g., esthetic requirements, reduced morbidity).
- Several pre-operative and intrasurgical conditions are met (Figs 4 – 5):
- Intact socket walls after tooth extraction with adequate bucco-palatal dimensions to grant a facial gap >2 mm after implant placement
- Facial bone thickness of at least 1 mm
- Thick gingival phenotype
- No acute infection at the site
- The availability of bone to facilitate primary stability without selecting an improper implant diameter or prosthetically incorrect implant position
- Insertion torque 25 – 40 Ncm and/or ISQ value >70
- An occlusal scheme that allows for protection of the provisional restoration during function
- Patient compliance
Early implant placement (Type 2) (Buser et al., 2013)
This may be considered in most clinical situations when immediate implant placement is not indicated, mainly in sites with thin facial walls and defects that often require simultaneous bone augmentation procedures. Notably, the subcategory Type 2-3C is scientifically and clinically validated, showing excellent survival and success rates in long-term follow-up.
Implant placement in healed sites (Type 4)
This is the least desirable of the placement time options due to the risk of alveolar ridge resorption and extended treatment time. However, some patients with local or systemic conditions (e.g., smoking, diabetes mellitus, severe autoimmune diseases) that may alter the healing process of the extraction socket may benefit from this protocol.
When late placement is indicated for patient- or site-related reasons, an alveolar ridge preservation(ARP) procedure may be recommended to facilitate a less invasive and predictable future esthetic restoration (Couso-Queiruga et al., 2022). This is of particular interest in clinical situations such as:
- Extraction sites where a significant ridge reduction is expected that may jeopardize the implant placement in a bio-restorative position, such as:
- Thin (<1 mm) or severely damaged buccal bone plates
- Posterior sites with limited ridge height that may lead to implant placement with concomitant maxillary sinus floor elevation or inadequate implant size selection to avoid nerve structures or bone dehiscences
- Young patients where the implant placement will be significantly delayed in time
Implant designs
Implant design is a broadly discussed factor for the successful replacement of missing teeth in the esthetic area.
Even though the use of tissue-level implants in the esthetic zone has been reported in the literature (Siebert et al., 2018), bone-level implants offer several advantages over the former in the esthetic area. Among these advantages are the following:
- A more extensive tolerance range for abutment height and shape selection according to the supracrestal tissue height (STH) and implant depth (Fig. 6)
- Significant versatility for abutment replacement if soft tissue recession or other problems occur
- Space maintenance for simultaneous guided bone regeneration procedures (GBR) of the surrounding bone ridge coronal to the implant platform employing slim and long healing abutments or screw-retained abutments (SRAs) during the healing period – instead of cover screws or wide machine collars from TL implants
- Improved emergence profile in narrow restorative spaces and reduced physiological remodeling around the abutment due to platform switching and deeper implant placement with slim abutment emergence until the bone level height is reached
Other designs such as “tapered implants” have demonstrated several advantages when used in the anterior segments of the mouth to avoid bone fenestration at the apex due to pronounced ridge concavities and to improve primary stability.
Also, implants with a unique thread design – large anchoring surface – such as BLX Implants® (Straumann, Basel, Switzerland) may be beneficial to increase the primary stability in favor of immediate loading and immediate implant placement to improve esthetic results and long-term success rates (Gamborena et al., 2021).
Implant diameter
The most appropriate implant diameter depends on the restored edentulous span and residual bone ridge width.
- Preservation of the peri-implant buccal bone wall has been correlated with long-term peri-implant health (Spray et al., 2000, Monje et al., 2019)
- Narrow diameter implants (NDIs) contribute to preserving the buccal bone width, reducing the risk for future aesthetic problems such as peri-implant soft tissue dehiscence (Fig. 7) (Evans and Chen, 2008, Sanz-Martín et al., 2020, Romandini et al., 2021)
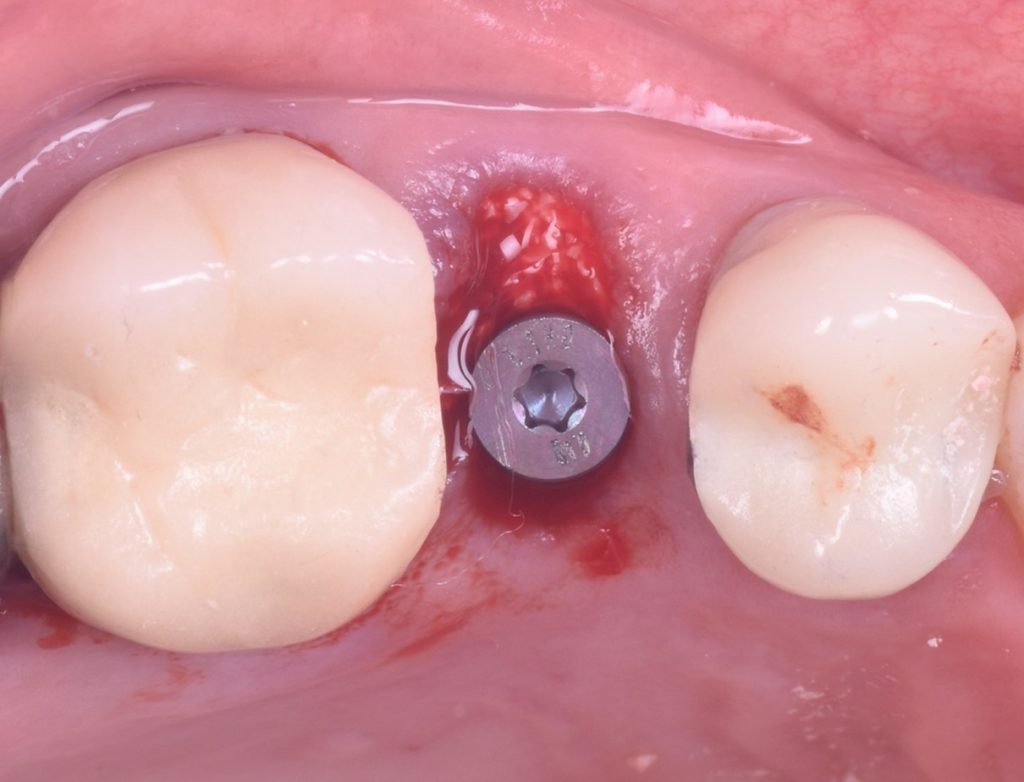
- During immediate implant placement, NDIs maintain the integrity of the labial bone and a facial gap >2 mm that can be filled with a slow resorption material so a future tissue collapse can be compensated (Figs 8 – 9) (Vignoletti and Sanz, 2014, Sanz et al., 2017)
- When reduced horizontal space to neighboring teeth is present, NDIs facilitate an adequate emergence profile and shape of the final prosthesis, resulting in better maintenance of the interproximal bone peaks without compromising the papillae
- More space between implants: where adjacent implants are placed too closely, bone remodeling can result in loss of bone height between adjacent implants, which will also affect soft tissue height between these implants (Tarnow et al., 2000)
Narrow diameter implants (NDIs) were shown to be effective when replacing a single tooth in non-load-bearing regions. Reinforced titanium implants such as TiZr (Roxolid®) are recommended to improve fracture resistance (Benic et al., 2013, Ioannidis et al., 2015).
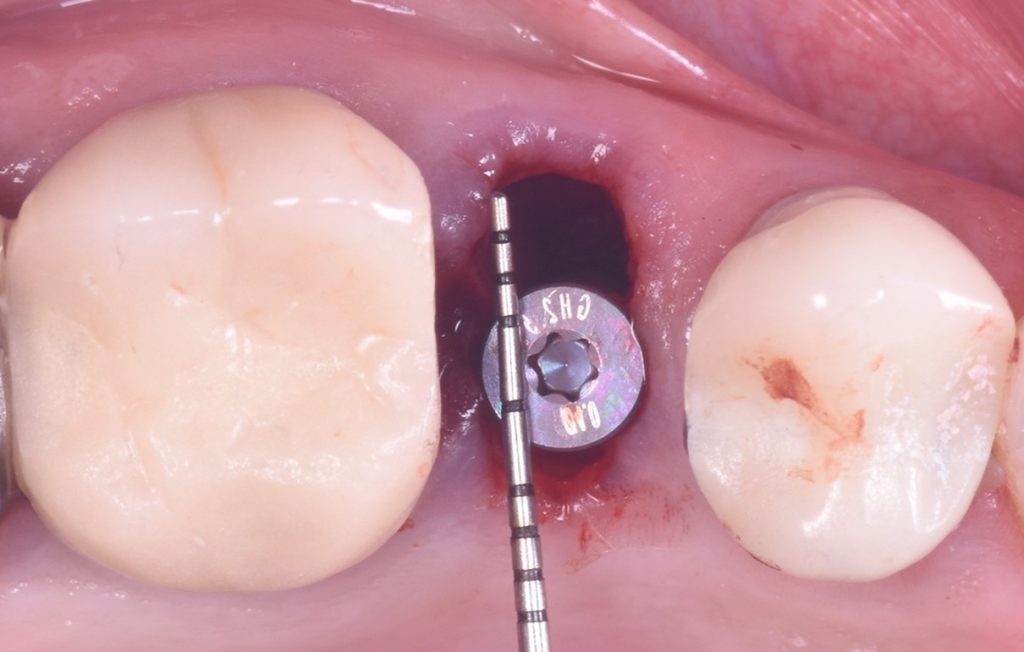
Three-dimensional implant position
Obtaining a successful outcome when treating an edentulous space with dental implants in the esthetic area will largely depend on the three-dimensional implant position. Implants that are correctly positioned have a lower risk of esthetic problems.
Since the level of the interproximal papilla is partly related to the bone level height of the adjacent teeth, which in turn is affected by the implant-tooth and implant-implant distance, a space of 1 – 1.5 mm between the implant shoulder and the proximal root must be respected. This distance must be increased to 3 mm between adjacent implants. Respecting these distances might reduce the interproximal crestal bone loss, establish the necessary vertical distance between the contact point and bone crest, and contribute to the presence of papillae (Salama et al., 1998, Tarnow et al., 2000, Cardaropoli et al., 2003).
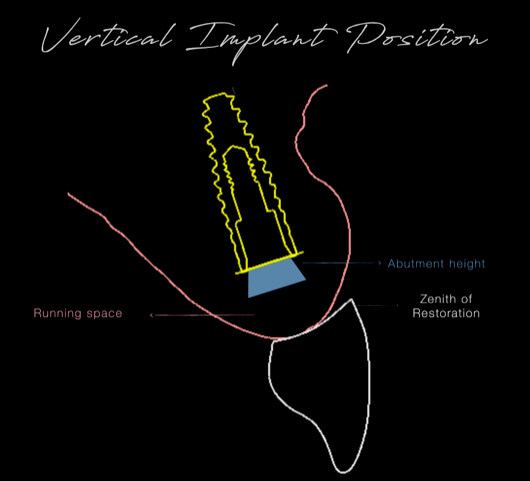
In determining the ideal corono-apical position of the implant, a digital tooth set-up determines the most apical boundaries of the intended restoration. Enough vertical space should be allocated for the transmucosal component connecting the crown with the implant. The following formula could be used:
“Most apical boundary of the intended restoration + running space + abutment mucosal height = vertical implant shoulder position “ (Fig. 10)
It has been demonstrated that the labio-palatal position of the implant in the esthetic zone plays a fundamental role in esthetic outcomes. Wide-diameter implants (Chen and Buser, 2009), buccal angulation of the implant, or implants too buccally positioned have a higher risk of soft tissue dehiscence (Sanz-Martín et al., 2020, Romandini et al., 2021). Also, implants placed too far palatally result in undesirable emergence profiles (Steigmann et al., 2014, Chu et al., 2019). Therefore, locating the implant axis 1 mm palatal to the incisal edge is recommended, so a screw-retained restoration is feasible. This will allow the clinician to maintain the retrievability of the implant-supported crown with direct screw access and, therefore, the possibility to modify the interim prosthesis to obtain an ideal emergence profile.
Digital implant planning will allow the clinician to choose a suitable surgical and prosthetic plan adequate to pursue bio-restorative implant restorations. Furthermore, digital surgical guides can substantially reduce human error compared to freehand implant placement (Fig. 11) (Bover-Ramos et al., 2018) and maximize the ideal 3D position following the treatment plan.
Summary
This blog article presents some technical and clinical considerations for performing an appropriate treatment when replacing missing teeth in the esthetic zone with implant-supported restorations. A proper 3D implant position is highlighted as one of the most critical aspects. The advent of new technologies allows advanced digital implant planning and guided implant surgery to address all the required variables according to the most up-to-date current scientific knowledge; in order to guarantee successful long-term outcomes in the esthetic area. Other variables (patient, anatomical, surgical, etc.) must also be considered but are not described in this blog.