Abstract
More and more patients are starting to demand solutions that do not involve the “gray” color of titanium in their treatment planning. White color, biocompatibility and low plaque affinity make zirconia dental implants the implant of choice for desirable esthetic outcomes. From the biological point of view, zirconia implants also enhance soft tissue integration. Zirconia implants can be presented in one- and two-piece design. Despite their popularity, more clinical studies need to be carried out to confirm the clinical outcome and the success rate of zirconia dental implants.
Introduction
Dental implant therapy is considered a well-documented and validated clinical procedure for restoring missing teeth. Currently, various implant systems and different materials are available on the market with the aim of restoring esthetics, function and improving the patient’s quality of life (Jung et al. 2012; Balmer et al. 2018). Due to patients’ esthetic requirements, proper selection of biomaterials (titanium alloys, titanium-zirconia alloys or zirconia) for implant placement is crucial for an optimal and satisfying result (Buser et al. 2019). Commercially pure titanium is the “gold standard” and first choice of treatment modality due to its favorable mechanical and chemical properties, successful osseointegration and well documented clinical success (Brånemark et al. 1977; Buser et al. 2012). However, one of the concerning disadvantages of titanium is its metallic gray color which can represent a challenge, especially in the esthetic anterior zone. This is more relevant in cases with a thin gingival biotype (Lorenz et al. 2019). Even though the prevalence of hypersensitivity or allergic reactions to titanium is low, 0.6% (Bianco et al. 1996; Sicilia et al. 2008; Cadosch et al. 2010; Jacobi-Gresser et al. 2013), soft tissues around dental implants may undergo corrosion in the oral cavity, which can lead to such a reaction. Nowadays, an increasing number of patients are starting to ask for metal-free solutions, esthetics being a major concern. Therefore, it is important to evaluate alternative materials that can achieve biocompatibility and a natural tooth-like color (Balmer et al. 2018). The first generation of ceramic implants was made of aluminum oxide, but, due to its unsatisfactory biomechanical properties, these implants were withdrawn from the market in the 1990 (Vanhakendover 1987; Cionca et al. 2017). Zirconium dioxide ceramic (zirconia) was introduced as an alternative to aluminum oxide, particularly tetragonal zirconia polycrystal 3% mol yttrium oxide stabilized zirconia as the material of choice for dental implants (Kelly & Denry 2008; Cionca et al. 2017).
In this blog, we will discuss the use of zirconia dental implants as an alternative material in oral implantology. In addition, we will explore their advantages and disadvantages when compared to titanium dental implants.
Why should we use zirconia dental implants?
Zirconia with its white tooth-like color, proven biocompatibility and low plaque affinity makes it a promising alternative to titanium implants (Fig. 1) (Salihoglu et al. 2011, Cionca et al. 2017; Rodriguez et al. 2018). In terms of properties such as good soft tissue integration, low plaque affinity and small amounts of inflammatory infiltrate, it is assumed that these implants may lower the risk of peri-implantitis (Cionca et al. 2017).

However, the recently published ITI Treatment Guide Volume 13: Prevention and Management of Peri-Implant Diseases, showed that peri-implant disease can also occur on zirconia dental implants (Heitz-Mayfield et al. 2023). These findings highlight the need for careful monitoring and maintenance of all types of dental implants to prevent potential complications and ensure long term success. Regardless, high flexural strength (900-1200 MPa), high fracture toughness, resistance to corrosion and wear, low thermal conductivity are just some of the favorable mechanical and physical properties of this material (Piconi & Maccauro 1999; Sanon et al. 2015). In challenging esthetic conditions, zirconia has shown itself to be the material of choice, with less influence on color changes than titanium in thin gingival biotypes (Jung et al. 2007).
However, we should be aware of some of the disadvantages these implants present. Low temperature degradation or aging presents a process where the metastable tetragonal phase transforms into monoclinic at temperatures above 200 degrees in the presence of water, which can result in a reduction in mechanical properties such as toughness, strength, or density of the material (Hashim et al. 2016). Studies have shown that commercially available two-piece zirconia implants have technical complications of 1.6%, including single crown chipping and fracture of the ceramic crown (0.8%) as well as fiberglass abutment fracture (0.8%) (Becker et al. 2017; Roehling et al. 2018).Moreover, diameter-reduced zirconia implants have shown a survival rate of 82.4%, which is not acceptable when compared with the survival rate of reduced-diameter titanium implants (Gahlert et al. 2013). Although both titanium and zirconia dental implants show similar hard and soft tissue integration, titanium implants show faster osseointegration (Roehling et al. 2019). It was estimated that the 1- and 2-year survival rate of zirconia implants was 98.3% and 97.2%, respectively, while 1-year marginal bone loss was 0.7 mm (Roehling et al. 2018). It was reported that the failure rate of commercially available zirconia implants was 2.4% (early failures 1.6%, late failures 0.6%, implant fracture 0.2%). Notably implant mobility was not presented with clinical signs of infection, which was described previously as “aseptic loosening” (Cionca et al. 2015; Roehling et al. 2018).
Despite the disadvantages, one of the most common indications for using these implants is the patient’s wish for a metal-free solution.
One- vs. two-piece zirconia dental implants
Currently, there are two types of zirconia dental implants available on the market: one and two-piece (Cantarella et al. 2021). The first to be introduced and designed was the one-piece zirconia implant which contains an abutment-like superstructure connected to the body of the implant, making it a solid piece (Cionca et al. 2015; Cantarella et al. 2021). One of the most challenging limitations of the one-piece design is that the implant needs to be placed in a perfect prosthetically-driven position, and computer guided implant surgery should be performed to achieve a satisfying result. If the implant is not placed in an adequate position, the only solution to correct the position is preparation of the suprastructure. However, preparation can negatively influence the fracture strength of the implant which can lead to undesirable outcomes (Cionca et al. 2017; Kamel et al. 2017; Cantarella et al. 2021). When using this design, clinicians should be aware that the final restoration can only be cemented, which can lead to biological complications that are well documented in the literature. In the esthetic zone – to avoid visibility of the crown margin – the implant is placed deeper, and the risk of the excessive cement increases (Figs 2 – 3) (Wilson 2009; Cionca et al. 2017).
To overcome these limitations, two-piece zirconia dental implants were presented. Currently, various abutment solutions such as zirconia abutments, PEEK abutments or titanium abutments are available. Even though titanium abutments have shown good results on titanium implants, their use on zirconia implants still needs to be investigated. The mechanical properties of zirconia and titanium are different. Zirconia can resist great pressure forces while titanium shows bending and flexural resistance instead of fracture (Piconi & Maccauro 1999; Joos et al. 2020; Cantarella et al. 2021).
When comparing the one-piece and two-piece designs, higher crestal bone loss and lower survival rate were demonstrated for the one-piece implant, while one study showed comparable results regarding crestal bone loss and survival rate for both (Fig. 4) (ArRejaie et al. 2019).
Case presentation
This case was treated at the School of Dental Medicine, University of Belgrade. A 26-year-old male patient presented to the Oral Surgery Clinic with a missing right central incisor in the maxilla due to a traffic accident six months earlier (Fig. 5).

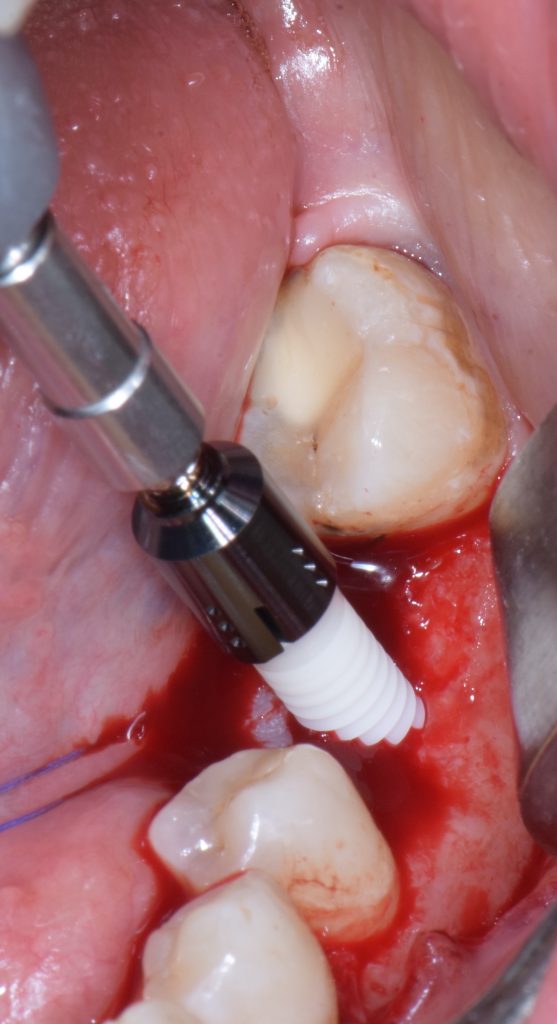
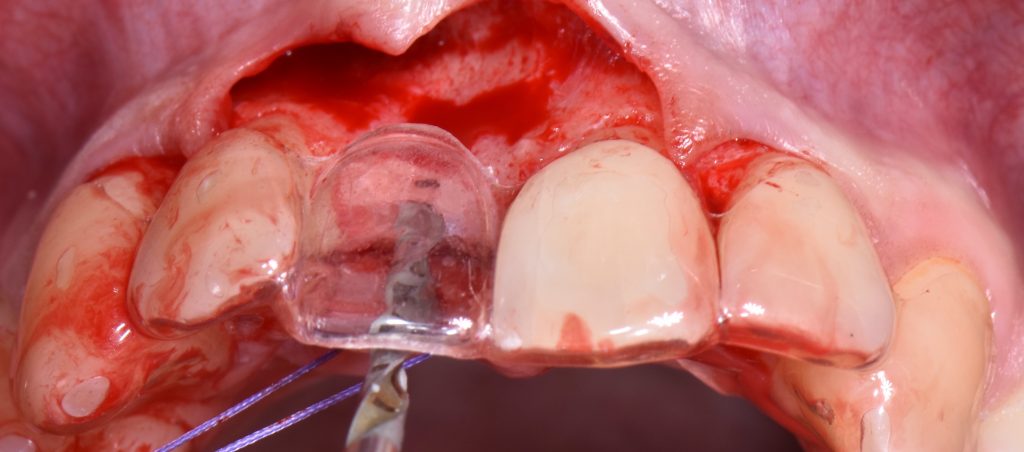
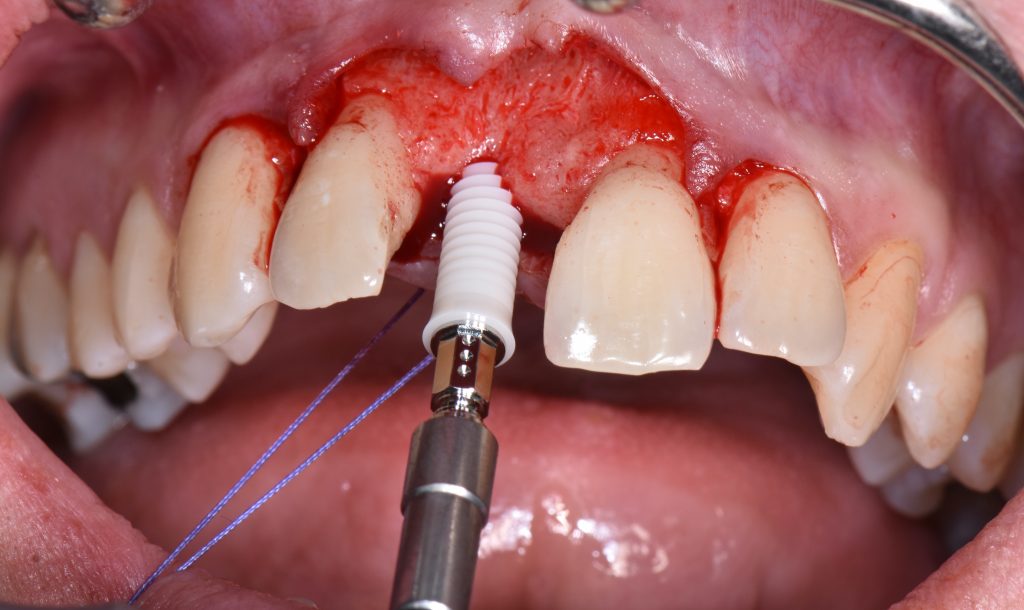
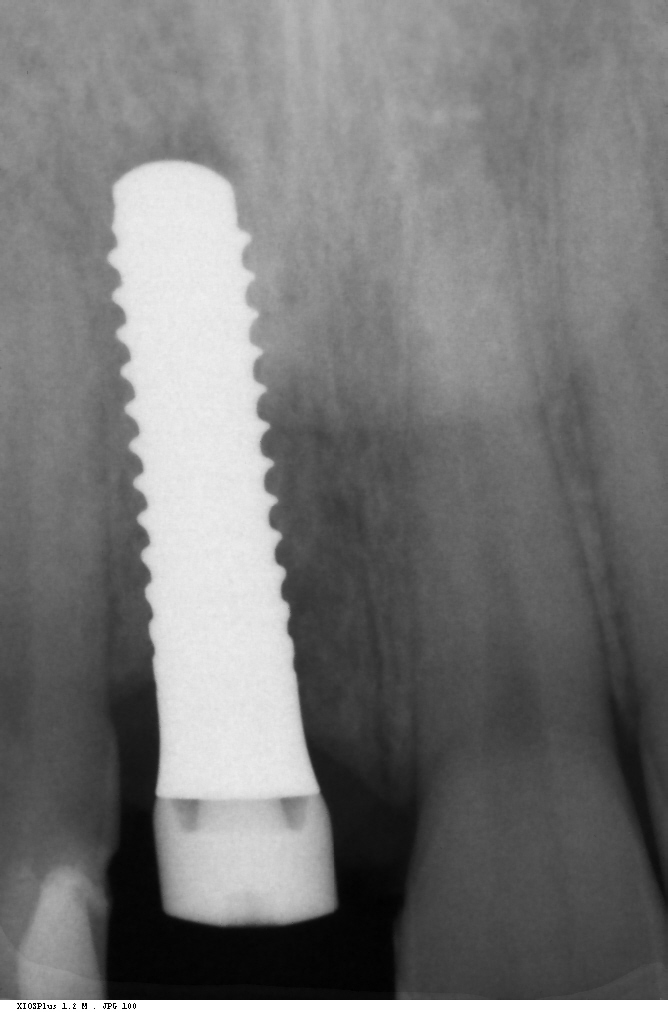
The patient had no significant medical history, and the examination revealed good oral hygiene and periodontal health. A CBCT scan was performed and showed adequate bone volume for implant placement. After obtaining informed consent, a surgical procedure for the placement of a Straumann two-piece Pure Ceramic implant was carried out. The surgical procedure was performed under local anesthesia using 4% Articaine, 1:100.000 epinephrine. The implant was placed in the correct 3D implant position using a surgical guide (open V design) according to the Straumann protocol (Buser et al. 2004) (Figs 6 – 7).
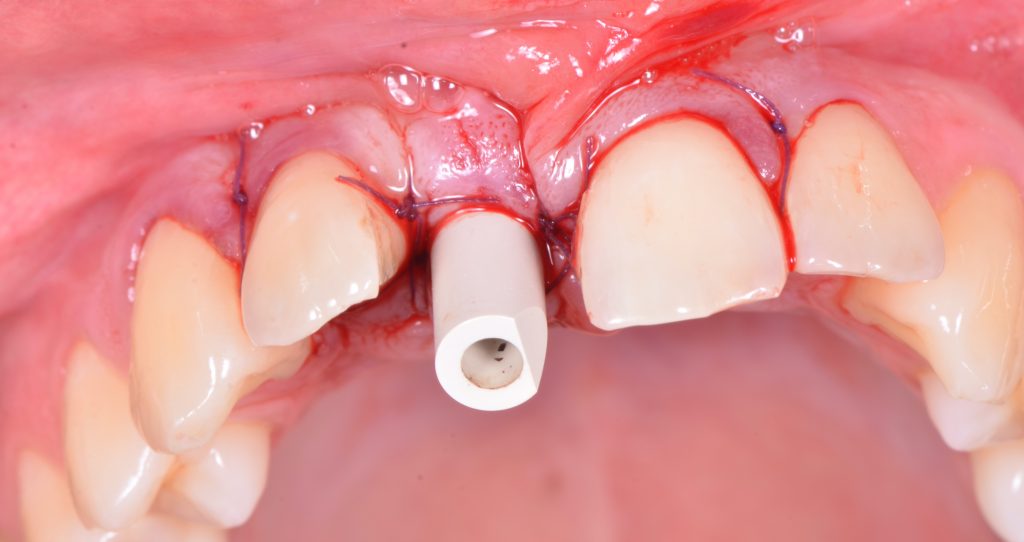
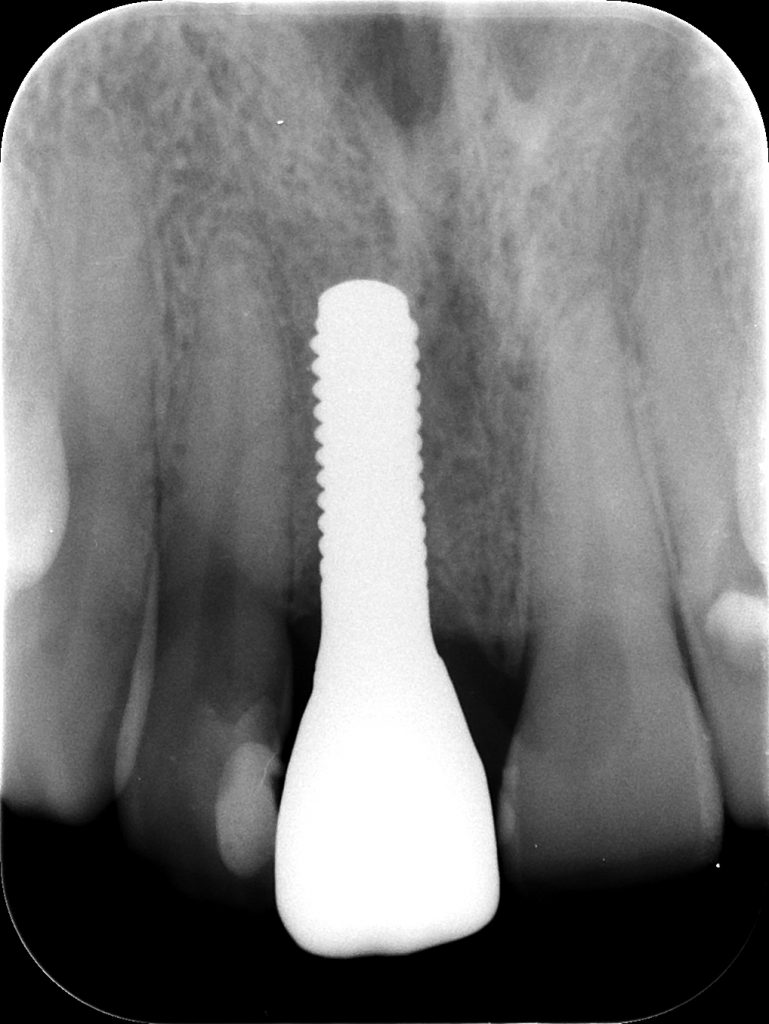
The torque wrench indicated high insertion torque of 35 Ncm and an immediate loading protocol was planned (Gallucci et al. 2018). A healing abutment (Institute Straumann) was placed, and primary wound closure was achieved with 5-0 single resorbable sutures (AssuCryl Lactin, Assut Sutures of Switzerland, Pully-Lausanne, Switzerland). A control periapical radiograph was performed (Fig. 8).
After implant placement, a scan body was placed and a digital impression was taken with an intraoral scanner (3Shape E1, 3Shape, Copenhagen, Denmark). The final virtual design of the provisional restoration was performed with 3D design software (Exocad Matera 2.3, Exocad, Darmstadt, Germany). Drilling of the PMMA block was completed in a 5-axis milling machine (Zenotec Select, Wieland, Pforzheim, Germany). The temporary crown was delivered 24 hours after surgery (Figs 9 – 10).
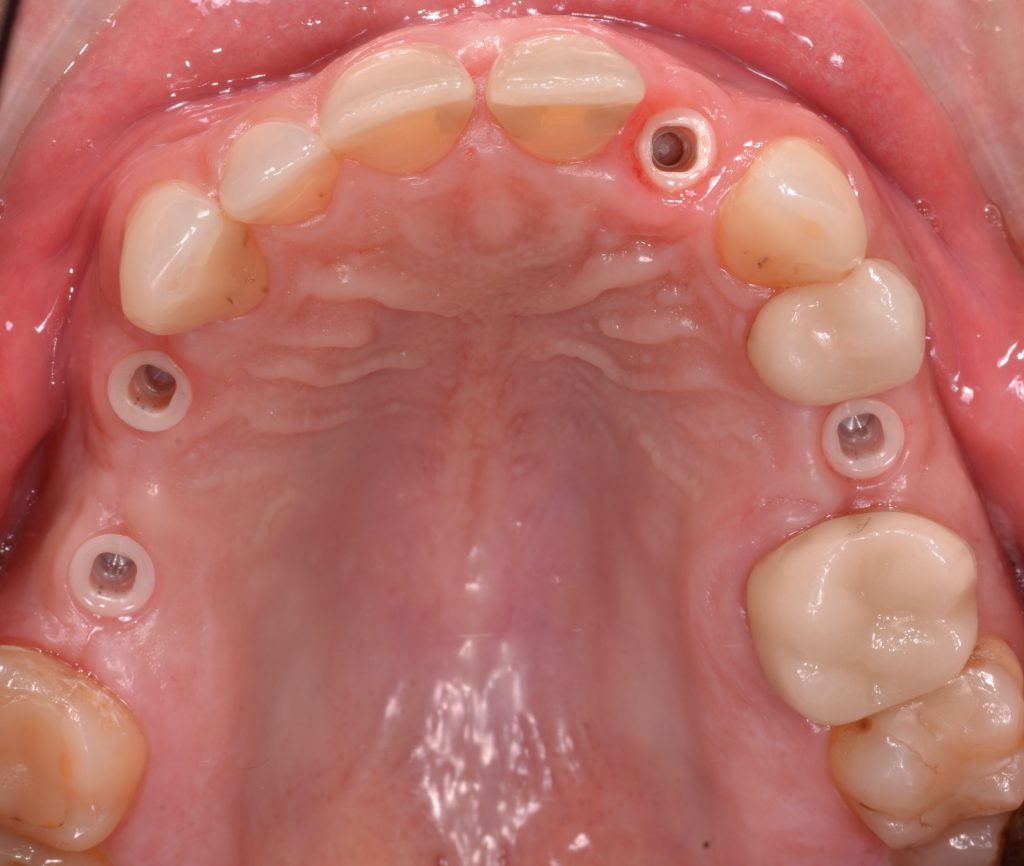
Four months after the surgery, a screw-retained layered zirconia crown was fabricated and delivered. The patient received instructions for oral hygiene and regular follow-up visits. The patient was followed up at 3 years, and the clinical and radiographic evaluations showed satisfactory results with no complications (Figs 11 – 12).
The implant showed successful osseointegration, and the soft tissues around the implant were healthy and stable. The esthetic result was satisfactory, and the patient reported good function and satisfaction (Figs 13 – 14).
This case report highlights the successful rehabilitation of a traumatic missing central incisor in the upper jaw with a Straumann Pure Ceramic implant.
Conclusion
The use of zirconia dental implants in modern implantology is a promising solution for patients seeking a biocompatible and esthetic alternative to traditional titanium Implants. However, further research is needed to evaluate the long-term clinical outcomes of zirconia dental implants.
Acknowledgment
I would like to thank my mentors Dr. German Gallucci, Dr. Aleksa Markovic and Dr. Miodrag Scepanovic for their collaboration and involvement in the zirconia dental implants project and also for their contribution to my academic and clinical development.
Read more in the Forum Implantologicum feature topic “Zirconia in Implant Dentistry“
Learn more about zirconia in implant dentistry in the ITI Academy