Introduction
The replacement of missing teeth in the anterior area with dental implants is one of the most challenging topics in implant dentistry. Guided bone regeneration (GBR) is a procedure often performed, especially in the case of ridge deficiencies. It allows for implant placement in a prosthetically driven position and favorable esthetic results. This approach is a common and established procedure carried out before or simultaneously with implant placement. In a recently published clinical study, a new type of GBR technique called the “L-shape technique” was presented. Its purpose is to increase the cervical volume at the time of implant placement. This enables clinicians to achieve highly esthetic outcomes with implant therapy in the anterior zone. Therefore, the aim of this blog article is to introduce this new methodology and to describe the clinical experience and scientific evidence behind the technique.
The rationale behind the L-shape technique
It is well known that the PASS principle is important to achieve predictable and successful outcomes for GBR. The PASS principle – Primary closure to ensure undisturbed and uninterrupted wound healing, Angiogenesis to provide necessary blood supply and undifferentiated mesenchymal cells, Space maintenance/creation to facilitate adequate space for bone ingrowth, and Stability of wound and implant to induce blood clot formation and uneventful healing events (Wang et al. 2006).
Nowadays, one of the most commonly used GBR procedures is the conjunctive use of bone graft substitutes with a resorbable membrane. Even though this combination is well documented, displacement of bone particles may frequently occur after flap closure. According to in-vitro data, using a so-called soft-type bone block and pins for the fixation of the membrane significantly reduces bone graft displacement and, at the same time, can better maintain the buccal contour after flap closure when compared to the use of conventionally used particle bone substitute without membrane fixation (Mir Mari et al. 2017). In other words, the above combination of materials leads to the enhancement of space maintenance, stability of the wound, and blood clotting according to the PASS principle. From an esthetic point of view, the volume at the future cervical aspect of the implant-borne restoration is the most critical. This encompasses both the horizontal and vertical extent of the ridge at the implant shoulder. The so-called L-shape technique was developed based on these prerequisites (Zuercher et al. 2021). It involves using a collagenated soft-type bone block trimmed into an “L” shape. The “L” is placed buccally and crestally, allowing for over-augmentation at the level of the implant shoulder. It is covered with a resorbable membrane fixed with resorbable pins apically. Using a specific geometry of bone substitute material enables maximum volume at the buccal, compensating for subsequent horizontal bone resorption.
What is the surgical protocol of the L-shape technique?
Flap design and implant placement
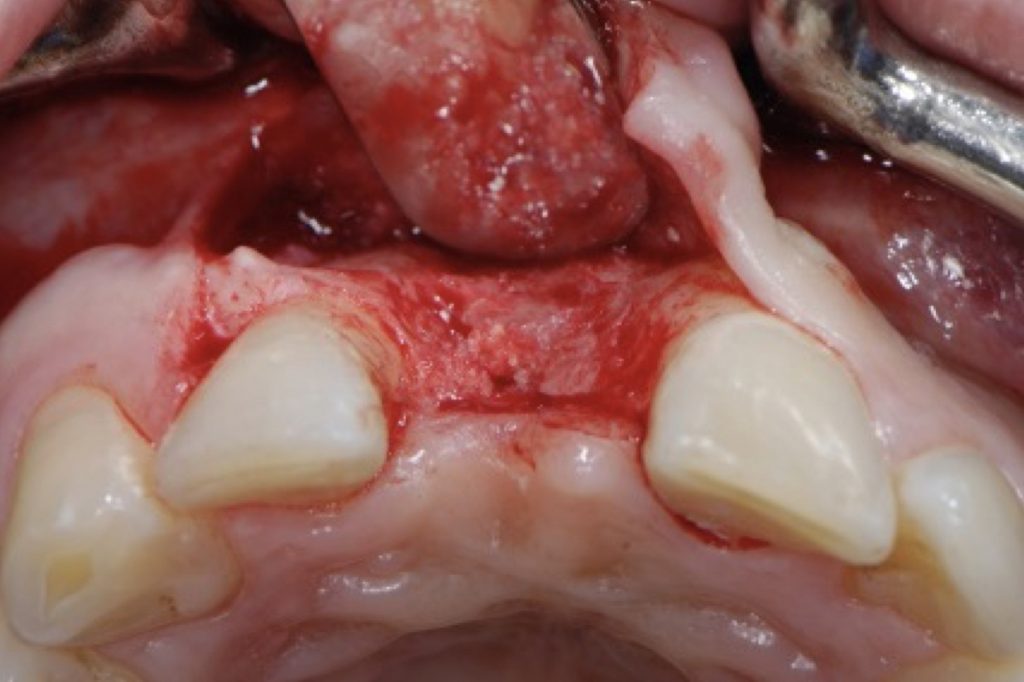
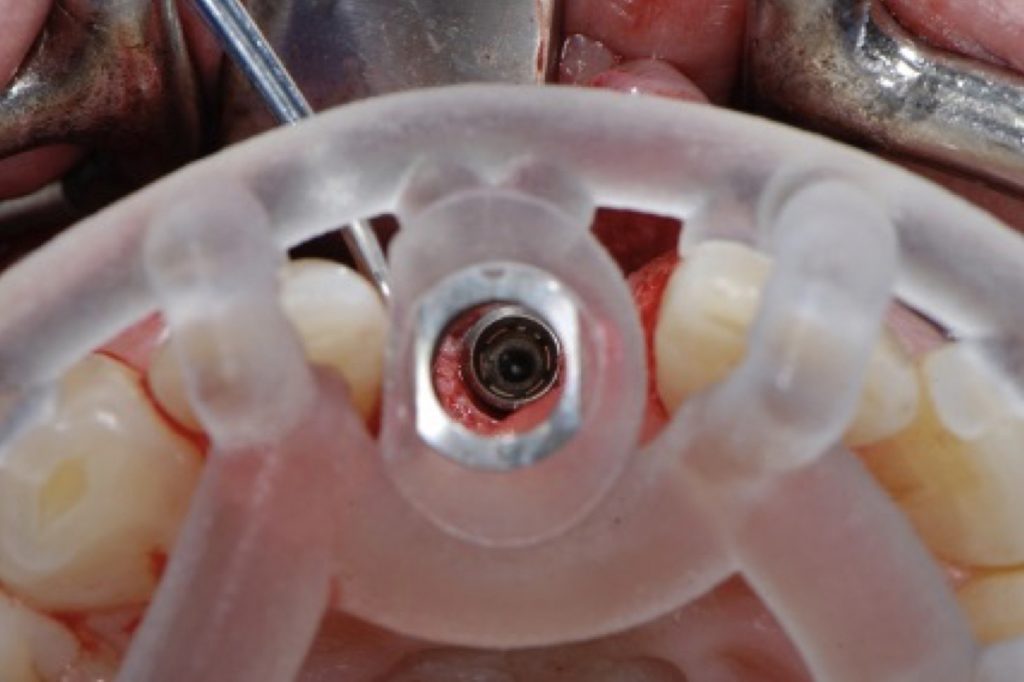
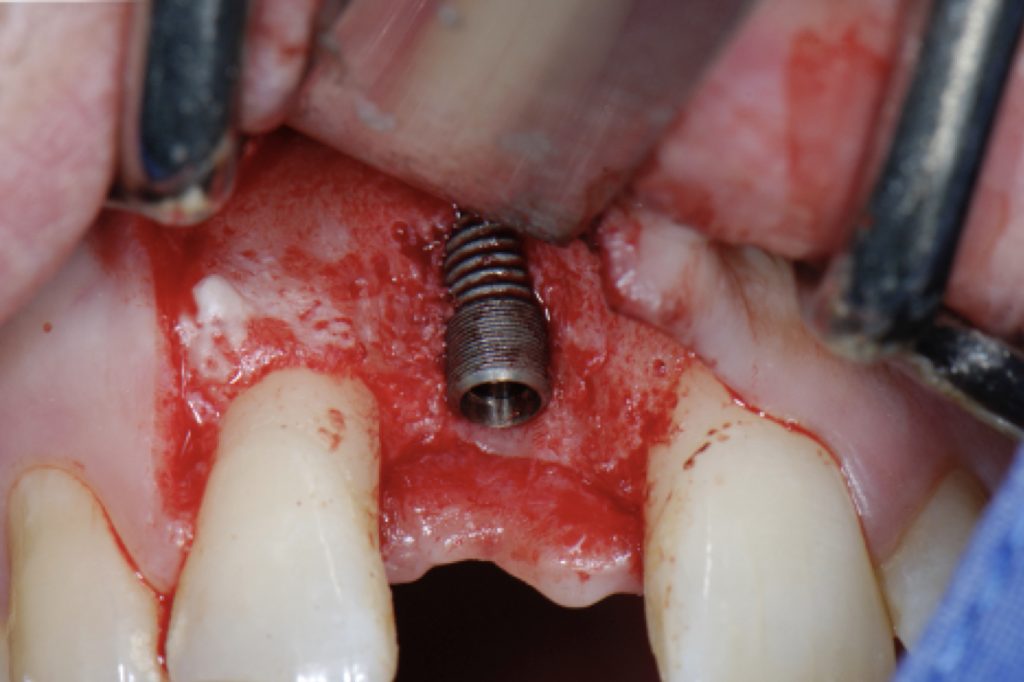
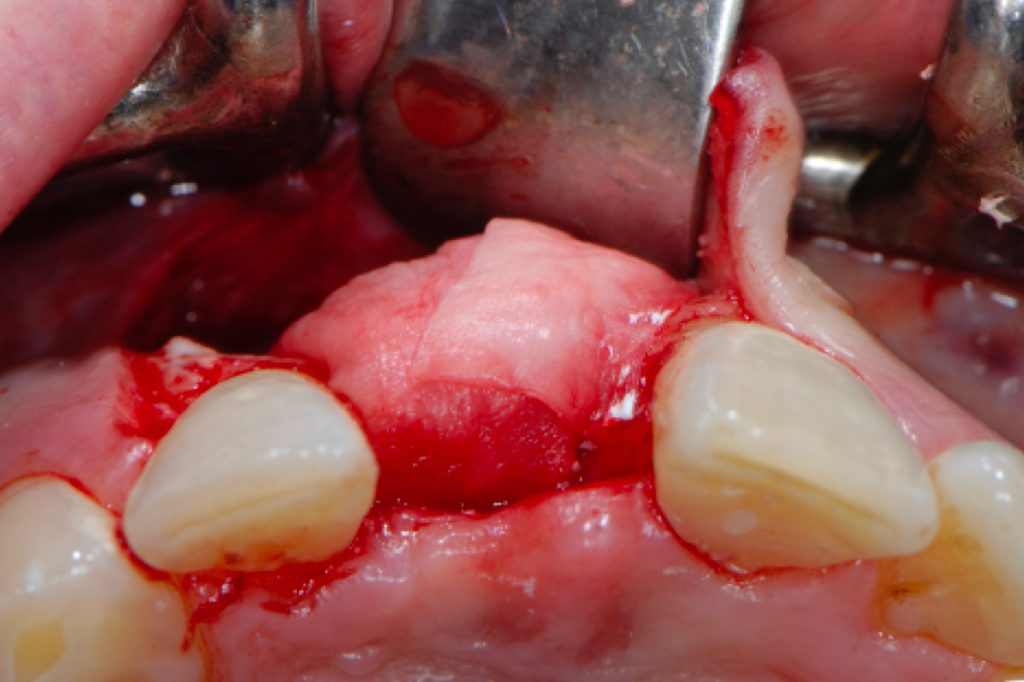
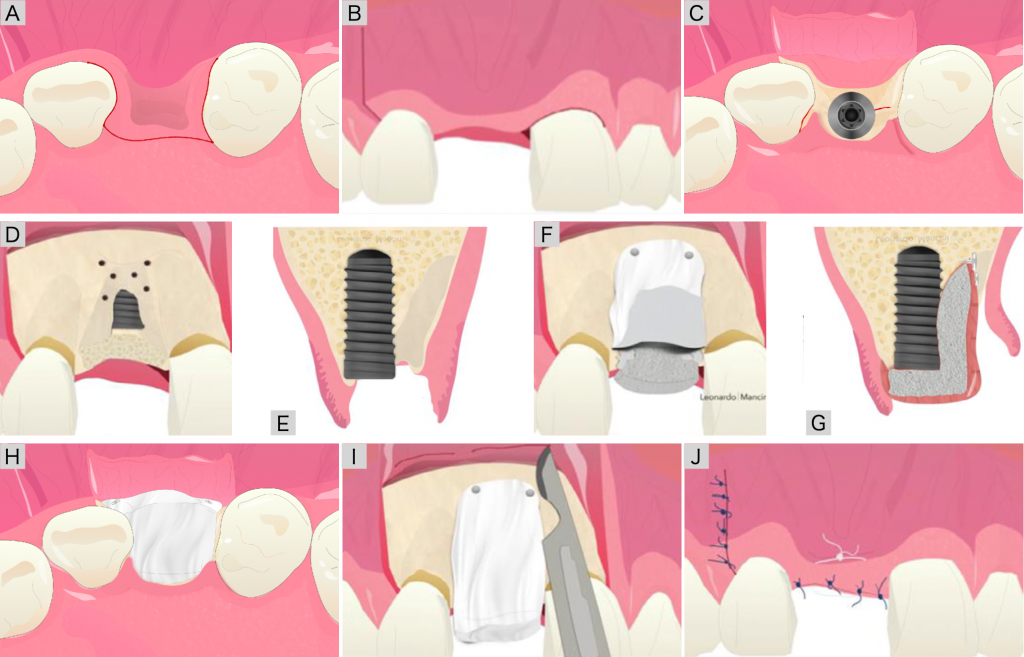
After administering local anesthesia, a palatally oriented crestal incision connecting the two adjacent teeth is performed (Fig. 8A). A sulcular incision follows this at both adjacent teeth. One vertical releasing incision called a ‘hockey stick’ is placed at the most distally possible aspect of the adjacent tooth intersecting the sulcus at a right angle (Fig. 8B). A full-thickness flap is elevated allowing for the assessment of the alveolar ridge contour. The implant bed is prepared, and the implant is placed in a prosthetically ideal position mostly requiring GBR (Figs 8C, E).


GBR procedure with L-shape
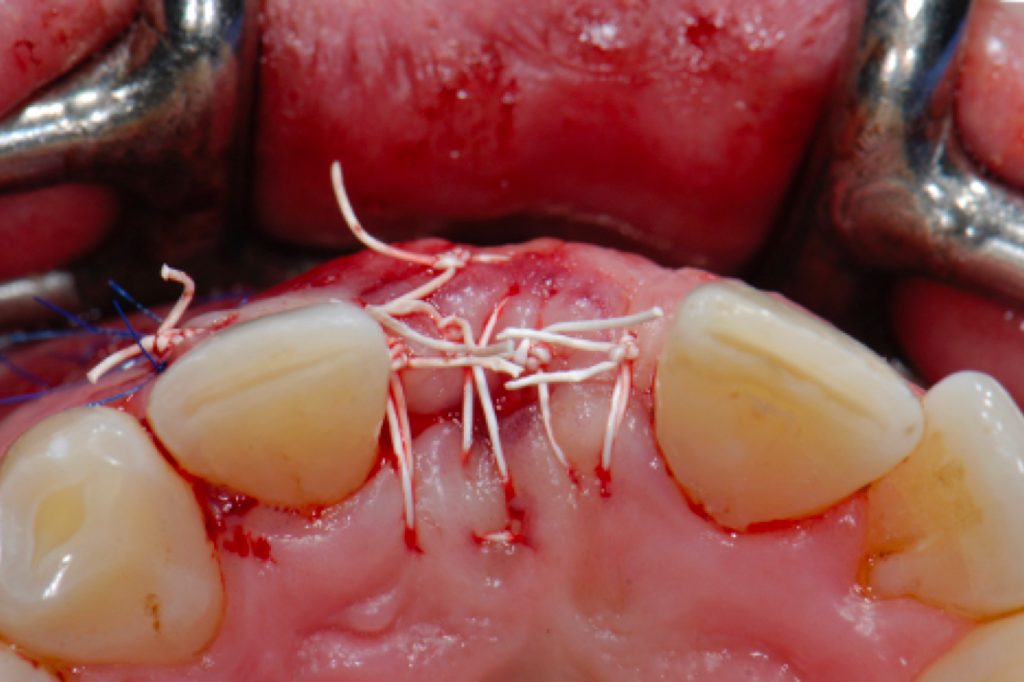
After implant placement, decortication at the area planned for GBR is performed using a pilot drill or a fine round bur. Two perforations should be prepared at the apical area to allow placement of the resorbable fixation pins to anchor the membrane (Fig. 8D). A resorbable collagen membrane is trimmed according to the defect size and placed in the ideal position. The membrane is fixed to the apical area (Fig. 8F). Thereafter, the L-shape block is trimmed. The soft-type bone block is soaked with sodium chloride or blood and shaped into an “L” using a scalpel or scissors. The L-shaped soft-type bone block is placed buccally and crestally at the level of the implant shoulder (Fig. 8G). If concave defects remain, they are augmented using the remaining material or conventional bone substitute particles. The previously attached collagen membrane is folded over the grafted materials and carefully adapted under the palatal flap (Fig. 8H). Periosteal releasing incisions are performed to advance the flap 2–3 mm over the palatal incision to achieve tension-free wound closure (Fig. 8I). The papilla region of the vertical incision should first be closed using interrupted sutures. A vertical mattress suture can help to place the papilla in its correct position. One horizontal mattress suture is applied to counteract post-operative swelling, with a needle inserted at the level of the mucogingival junction. The crestal incision is sutured with single interrupted sutures. Finally, the vertical incision is closed with single interrupted sutures (Fig. 8J).
Second-stage surgery
Around 4 months after implant placement, second-stage surgery is usually performed. The crestal soft tissue area is de-epithelialized, followed by a u-shaped incision. The cover screw is changed to a healing abutment folding this small flap towards the buccal side, allowing for slight augmentation of the buccal contour. In the case of the seldom occurrence of bone on top of the implant, this can be safely and easily removed using curettes, ultrasonic scalers, or specially designed trephine burs manufactured by the respective implant manufacturer.
Outcomes
The retrospective clinical study referred to concluded that the L-shape technique seems to be a reliable procedure resulting in stable clinical and esthetic outcomes accompanied by high levels of patient satisfaction.
The evaluation of the clinical parameters at recall appointments revealed the following: mean probing depth (PD) 2.72 ± 0.76 mm, plaque index (PI) 5.0% ± 0.09%, and bleeding on probing (BOP) 15% ± 0.26%. The mean width of mid-facial keratinized mucosa measured 2.93 ± 1.38 mm. These findings indicate a sufficient amount of keratinized mucosa and healthy peri-implant tissues.
The pink esthetic score (PES) and the white esthetic score (WES) revealed mean values of 10.7 ± 3.3, 8.8 ± 1.4, respectively. An example of a clinical case treated with the L-shaped technique in region 11 is shown in Figure 4.
Patients’ overall esthetic satisfaction was assessed using a numerical rating scale (NRS) at the follow-up visit. The mean NRS amounted to 9.4 ± 0.8, indicating that all patients were almost entirely satisfied with their treatment outcome.

Summary
This blog article presents the rationale behind the so-called L-shape technique with a step-by-step clinical protocol and current evidence. Within the limitation of the available studies (Zuercher et al. 2022, Lee et al. 2021, Jung et al. 2021), this novel GBR technique achieved not only favorable esthetic outcomes, but also high patient satisfaction. So far, there is no gold standard for the GBR procedure in the anterior zone leading to superior esthetic outcomes. However, the technique presented may be recommended in suitable clinical situations.