Abstract
In modern implant dentistry, osseointegration and bone regeneration are no longer the main focus. Patients are not only asking for functional restorations but also for natural-looking and esthetically satisfactory implant rehabilitations. Mucosal recessions are a common biological complication around dental implants in the esthetic zone. There are various possible causes; however, just one factor like implant malpositioning will suffice. Soft tissue recession is always preceded by bone dehiscence; hence, soft tissue correction is performed not only for esthetic reasons but also to avoid or correct rough implant-surface exposure with possible onset of peri-implantitis. Soft tissue augmentation can be a decisive factor for a long-term stable result. Treatment options include coronally advanced flaps (CAF), tunnel technique (TT), or submergence of the implant with/without prosthetic changes. In addition, different soft tissue graft donor sites are available with distinctive advantages.
Introduction
Implant-based rehabilitation is a clinical challenge, especially in the esthetic zone. Patient expectations have changed, and esthetics play an essential role in defining the success of rehabilitation. Surgical soft tissue management can be carried out at different stages during implant reconstruction and surgical techniques can be divided into two main categories: increase of keratinized tissue width and increase of soft tissue thickness/volume.
- The goal of keratinized tissue augmentation techniques is to obtain a band of keratinized tissue attached to the periosteum that increases the depth of the vestibular fornix and improves patient home care and plaque control (Souza et al. 2016; Jepsen et al. 2018; Perussolo et al. 2018; Zigdon et al. 2008).
- The goal of soft tissue thickness augmentation techniques is to create or restore the peri-implant supracrestal soft tissues by increasing their thickness and height from the bone crest to the mucosal margin using different kinds of connective tissue grafts (CTG); these tissues are crucial to obtain a natural emergence profile of the prosthetic restoration and to ensure a satisfying esthetic result. These techniques are commonly performed in the anterior area (Tarnow et al. 2021; Anderson et al. 2014).
The main time points to consider for soft tissue management are predominantly before implant placement, simultaneously with implant placement, and during second-stage surgery. Soft tissue augmentation, however, can be carried out even later to correct complications that can arise after delivery of the prosthetic restoration.
Causes of soft-tissue deficiencies
Patient-related factors
As is known in every field of dental surgery, systemic or behavioral factors such as inadequate oral hygiene, smoking, non-compliance, and uncontrolled diabetes are not only predisposing factors for soft tissue recession but also negative prognostic parameters for corrective surgery (Decker et al. 2017; Cortellini & Tonetti 2004; Cairo 2017).
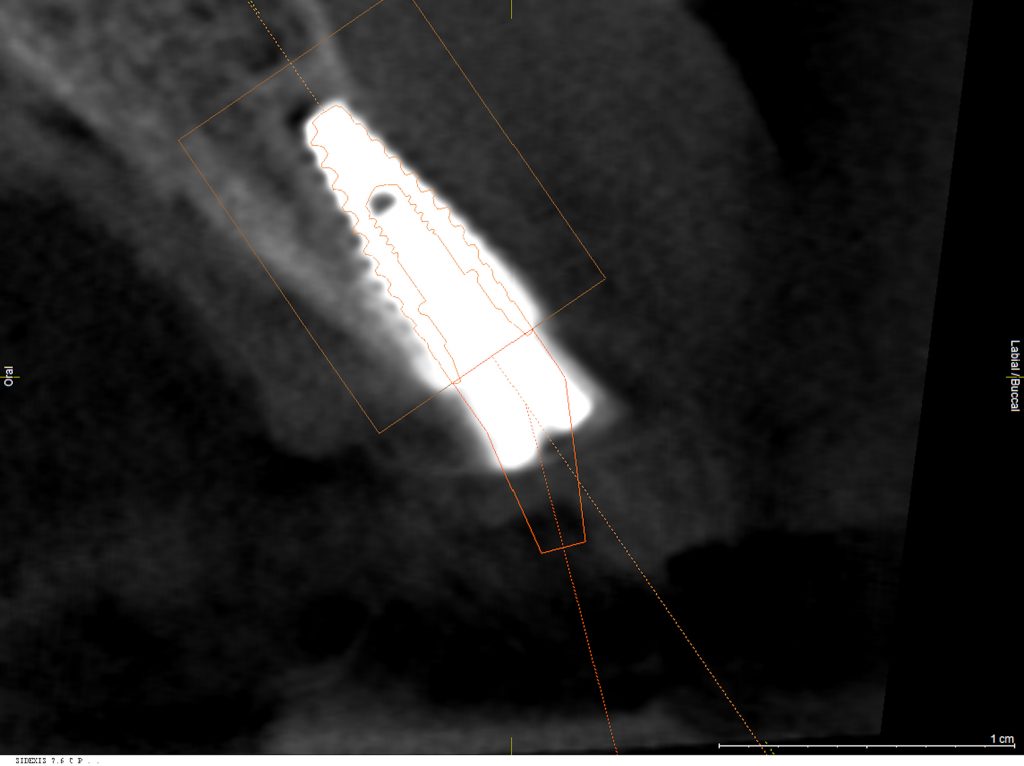
Implant position
Accurate implant placement seems to be the dominant causative factor for the development of mucosal recession (Zucchelli et al. 2019). Buccal implant position has been reported with a nearly 35 times higher probability for mucosal recession development (Sanz-Martin et al. 2020). If the implant shoulder is located outside the ridge contour, and it is impossible to compensate for this too distant buccal position by reshaping the prosthetic emergence profile or with angulated components, it has to be seen as irrational to treat (Zucchelli et al. 2019). Most reports primarily focus on bucco-oral positioning; however, vertical placement is just as important. In the case of a bone level implant, the implant shoulder should be placed 3 – 4 mm below the anticipated mucosal margin (Dawson et al. 2008). Case analysis with an analog or digital mock-up is recommended. The mesio-distal implant position has a minor impact on facial tissues, and papilla presence or formation may be impaired (Grunder et al. 2005).
Soft tissue factors
The peri-implant phenotype was recently introduced (Avila-Ortiz et al. 2020). A thin peri-implant phenotype is characterized by horizontal mucosal thickness <2 mm (MT), vertical soft tissue height <3 mm, and attached/keratinized mucosa width <2 mm (KM). While there is limited evidence for successful coverage of shallow mucosal recession, there is no data on the treatment of deep (>2 mm) and wide recessions (Sculean et al. 2017). Reduced diameter prosthetic components will provide more space for interdental tissues and, thereby, better blood supply and tissue healing (Zucchelli et al. 2013).
Hard tissue aspects
A thin peri-implant phenotype is characterized by thin, soft tissue dimensions and buccal/oral bone thickness <2 mm (Avila-Ortiz 2020). A 2-mm-thick buccal bone plate is advised to minimize bone resorption and maintain stable soft tissue levels (Merheb et al. 2014). It is noteworthy that the mucosal level seems to be more dependent on soft tissue thickness than bone thickness, at least in the short-term (Kato et al. 2018).
Discussion
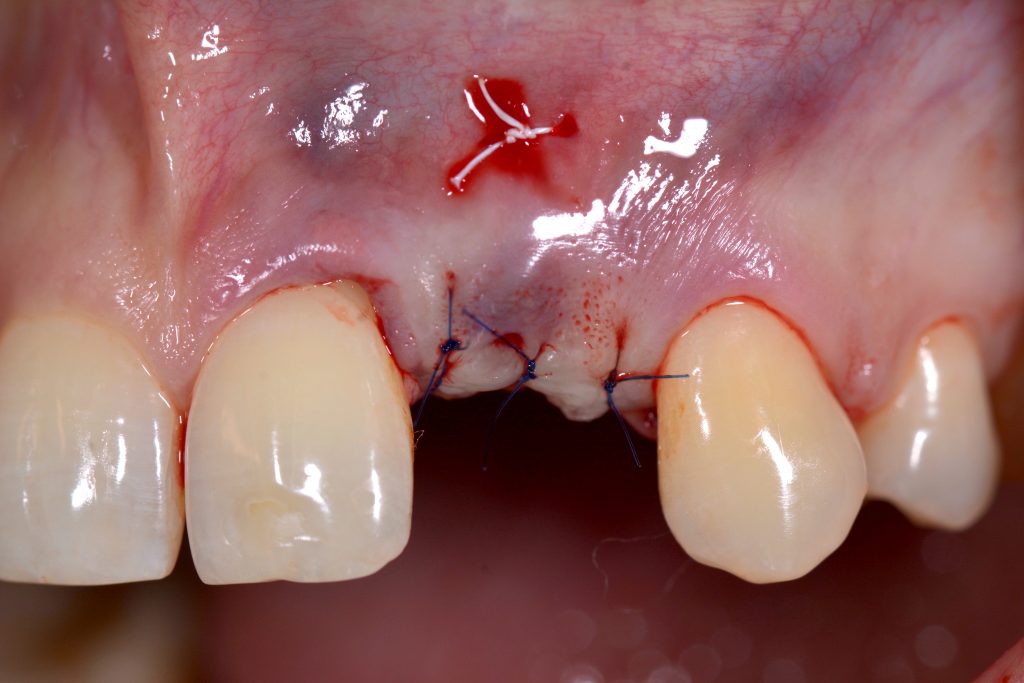
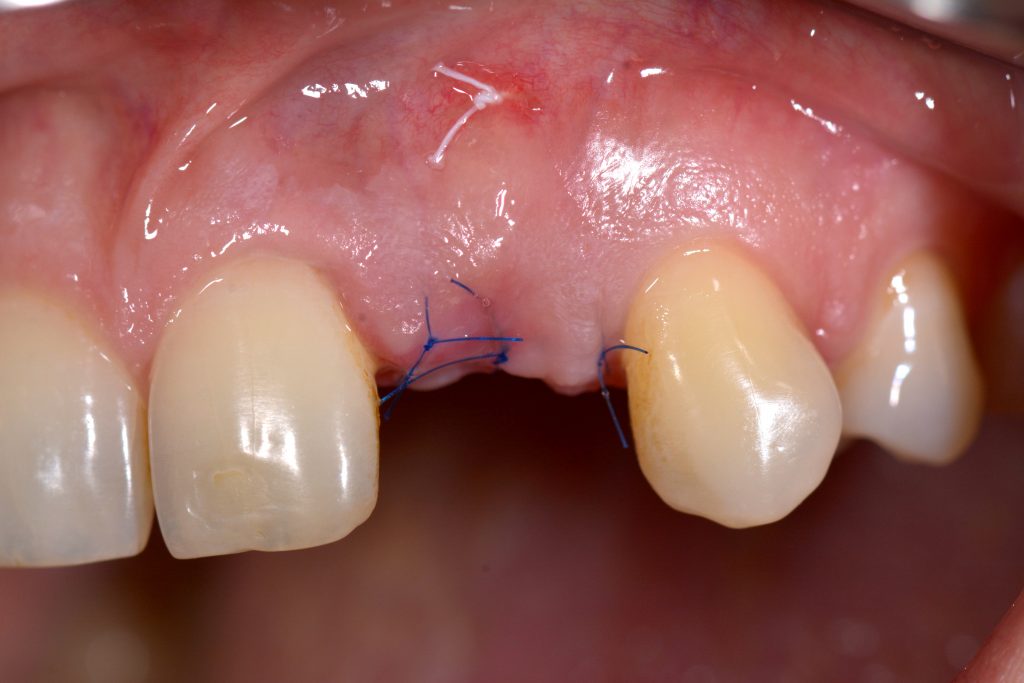
Although the incidence of esthetic complications seems to have decreased in recent years, there is a growing demand for clinicians performing implant placement to no longer focus simply on osseointegration or bone augmentation but also on soft tissue management (Pjetursson et al. 2014; Chackartchi et al. 2019). The patient may experience peri-implant soft tissue deficiency (PSTDef) as a grayish shimmer or a dark shadow buccal to the implant. Correction of PSTDef can be done before, together with, and after prosthetic delivery; however, due to easier access, soft tissue augmentation is recommended either before or while uncovering the implant (Thoma et al. 2014). A recent systematic review evaluated the impact of peri-implant phenotype modification techniques (Tavelli et al. 2021). The gain in MT revealed comparable results for CTG (+ 1.13 mm) and acellular dermal matrices (ADM; + 1.08 mm), followed by collagen matrices (CM; + 0.76 mm). As in plastic periodontal surgery, there is an ongoing debate whether CAF (with/without vertical releasing incisions) or “incision-free techniques” like TT is the superior option to cover peri-implant soft tissue dehiscence (PSTDeh). To the authors’ best knowledge, no clinical trial and, consequently, no systematic review has assessed the outcome of these approaches comparatively. Leading experts in plastic periodontal and peri-implant surgery advocate both techniques with related advantages. They have published treatment protocols or clinical cases using CAF (Zuchelli et al. 2019, Zuchelli et al. 2013) or TT (Sculean et al. 2017; Gamborena & Avila-Ortiz 2021; Zuhr et al. 2018). Hence, no purely scientific conclusions (external evidence) can be drawn, and technique selection might depend on the clinician’s preference/experience (internal evidence) or local factors. Local factors can be recession depth, the width of KM, and papilla width. CAF might allow better access to the implant surface or defect and greater flap mobility in single implants.
On the contrary, by avoiding extrasulcular incisions, applying TT will minimize scar formation and preserve papilla integrity and blood supply (Zuhr et al. 2018). A third option besides CAF and TT is to re-submerge the implant by removing the reconstruction. This will allow an additional gain in KM if the CTG is intentionally left exposed, helping to maintain the mucogingival junction later during the 2nd stage and allowing thickening of the papilla area. Future clinical studies should compare different treatment concepts (e.g., CAF versus TT) and the influence of varying defect configurations (e.g., exposure of prosthetic components vs. exposure of implant surface).
Autologous soft tissue grafts are still the gold standard in periodontal and peri-implant soft tissue management (Zuchelli et al. 2020). Within the last decade, de-epithelialized connective tissue grafts (deepCTG) and tuberosity grafts (tuberCTG) have become more popular. These grafts contain more lamina propria and fibrous connective tissue, supposedly making these grafts better suited for MT and KM augmentation (Sanz-Martin et al. 2019; Bertl et al. 2015). However, incomplete removal of the epithelial layer or graft exposure with deepCTG or tuberCTG might impair esthetics because of keloid-like healing, scar tissue formation, or differences in color compared to the recipient site (Maia et al. 2021; Zuchelli et al. 2014).
Conclusions & clinical recommendations
- Check crown-width to crown-length ratios in the anterior zone with mock-up (analog or digital);
- mainly treatment of shallow recessions seems predictable;
- CAF, TT, or implant re-submersion can be successful;
- application of any CTG can be successful in managing PSTD;
- if deepCTG/tuberCTG are used for their distinctive characteristics, flap overcompensation and careful removal of the epithelium are decisive factors.