Introduction
Complete edentulism continues to affect a significant portion of the population, especially among elderly individuals, despite significant advancements in preventive dentistry (Felton et al. 2016). For a set of complete dentures, the mandibular denture often exhibits poor retention and stability due to destabilizing anatomical features such as the mobility of keratinized tissues, tongue movement, reduced surface area or diminished muscular control, leading to discomfort and anxiety (Müller et al. 1995; Awad & Feine 1998). Consequently, according to the McGill Consensus of 2002, two-implant retained mandibular overdentures (IODs) have become the standard treatment option for rehabilitating edentulous mandibles (Feine et al. 2002, ITI Treatment Guide Volume 4). However, bone resorption following tooth loss often leads to insufficient bone volume, making the placement of standard implants (>3.5 mm) challenging or even unfeasible. To address this issue, narrow-diameter implants (NDIs) are used as an alternative to bone augmentation procedures. The available literature describes various types of NDIs, but it is generally accepted that an NDI is defined as an implant with a diameter of ≤3.5 mm. More specifically, following the 2018 ITI Consensus Conference, three categories of NDIs were proposed (i.e., (1): Ø Implants with a diameter of <2.5 mm (“Mini-implants”); (2): Ø Implants with a diameter of 2.5 mm to <3.3 mm; (3) Ø Implants with a diameter of 3.3 mm to 3.5 mm.( Schiegnitz E & Al-Nawas B. 2018, Jung et al. 2018). Mini dental implants (MDIs), classified as Category 1 NDIs, were initially used as transitional or provisional implants to stabilize interim prostheses during the osseointegration phase of conventional dental implants and for orthodontic anchorage, with a plan for subsequent removal (Krennmair et al. 2013). Later, histological studies confirmed the osseointegration of these implants, leading to their expanded use in definitive restorations, including fixed (single narrow edentulous spaces) and removable (partial and complete denture stabilization) prostheses (Flanagan D. 2021). This article aims to offer insights and practical guidelines for effectively utilizing MDIs in the rehabilitation of mandibular edentulism with IODs.
The role of mini dental implants (MDIs) in mandibular overdentures
Key features and designs of MDIs
MDIs are typically designed as one-piece implants with an integrated transmucosal abutment, which also incorporates an attachment to enhance the retention of dentures (Klein et al. 2014). Their unibody design compensates for the reduced dimensions by enhancing load resistance and provides several advantages, including eliminating the microgap at the implant-abutment connection (Trang et al., 2022). Additionally, it enables single-stage surgery, which can be performed in a flap or flapless approach. Most commercially available one-piece MDIs for overdentures are available in conventional lengths, tapered, self-cutting and composed of biocompatible titanium alloys to enhance their mechanical properties (Elias et al. 2008). In contrast to orthodontic and provisional implants, which typically have machined, smooth surfaces to facilitate their removal after temporary use, MDIs used for overdentures employ various surface modifications to enhance osseointegration. These modifications include sandblasting with aluminum oxide followed by cleaning and passivation with an oxidizing acid or a sandblasted, large-grit, acid-etched (SLA®) surface, similar to that of standard implants. (Proteasa et al. 2015; Yilmaz et al. 2020)
Recommendations for MDIs in mandibular overdentures
Since MDIs were introduced as a prosthetic solution for retaining mandibular overdentures, manufacturers have recommended placing a minimum of four MDIs in the inter-foraminal area for edentulous mandibles (Mundt et al. 2015). This rationale was proposed to compensate for the MDIs’ reduced diameter and smaller bone-to-implant contact area. In addition to this, in vitro studies have shown that increasing the number of MDIs correlates with improved overdenture stability, retention and maintenance of retentive force for a longer time (Alshenaiber et al. 2022; Alshenaiber et al. 2023). However, some researchers have explored the use of just two MDIs, following the standard of care for conventional implants. This minimal approach for MDI-supported overdentures remains debatable (Tomasi et al.2013; Catalan et al. 2016). Immediate loading of the implants is also possible with an insertion torque of 35 Ncm or higher and is more widely used with flapless implant placement (Šćepanović et al. 2015).
Regarding the recommended length of MDIs, a prospective cohort study observing 21 patients with MDI overdentures over one year reported that short (7-mm) and medium- length (10-mm) MDIs, as defined in the study, had a higher failure rate (38% versus 1%) compared to long MDIs (14-mm) (Tomasi et al. 2013). Notably, all failures were attributed to biological implant loss rather than mechanical failure. Therefore, length may influence longevity; however, further research is required to draw conclusions.
Patient-reported outcomes with MDI-retained overdentures
Regarding the impact of ΜDIs on patient-reported outcomes, previous studies have demonstrated that overdentures retained by MDIs enhance patient satisfaction (Lemos et al. 2017), oral health-related quality of life (OHRQoL) (Reissmann et al. 2018), and functional parameters compared to conventional complete dentures (Kabbua et al. 2020). These findings can be attributed to improved mastication and chewing efficiency. In a recent study, a mandibular overdenture utilizing four titanium-zirconium MDIs was found to significantly improve both masticatory performance (MP) and maximum bite force (MBF) in edentulous patients compared to their pre-treatment levels with conventional prostheses (Leles et al. 2024).
MDIs over conventional implants for overdentures
Survival rate and long-term outcomes of MDIs
The survival rate of MDI-retaining mandibular overdentures is reported to be 95.63% after an average observation period of 28.24 months (Jawad & Clarke 2019), comparable to that of conventional implants (De Souza et al. 2015; Temizel et al. 2017). Substantial evidence indicates that failure rates are generally higher in the maxilla than in the mandible (Tomasi et al. 2013; Proteasa et al. 2014). However, one study reported no significant difference in failure rates between the maxilla and mandible up to 4 years of follow-up, with the majority of patients receiving 6 implants in the upper jaw and 4 in the lower jaw (Mundt et al. 2015). Concerning peri-implant outcomes, a previous study (Enkling et al. 2020) reported an overall mean marginal bone change of −1.18 mm (±0.79) after 5 years in mandibular overdentures retained by four one-piece MDIs, remaining within clinically acceptable limits. The authors concluded that this treatment approach is predictable, ensuring stable peri-implant bone and soft tissue conditions.
Advantages of MDIs for mandibular overdentures
MDIs enable the rehabilitation of edentulous patients in cases where a highly resorbed residual ridge limits the placement of standard diameter dental implants. While grafting procedures can enhance bone width, they are often associated with a higher risk of side effects, longer treatment time and increased patient discomfort (Clavero et al. 2003). In addition, from an economic perspective, MDIs offer an advantage with their lower material costs compared to conventional implants, making them a potentially more affordable option (Bidra &Almas 2013). Other benefits of MDIs include the possibility of flapless placement, which reduces intraoperative trauma, and the potential for immediate loading, resulting in a shorter recovery period. These minimally invasive procedures are better tolerated by patients (Reissmann et al. 2018) and contribute to higher treatment acceptance, especially among elderly, edentulous patients who may be less inclined to undergo more complex interventions.
Surgical and technical challenges of MDIs
However, we should be aware of some surgical and technical complications that may occur during treatment. MDIs may be exposed to a higher fracture risk than standard implants due to their narrow diameter and tapered body design (Tabrizi et al. 2017, Holmgren et al. 1998). Moreover, anatomical factors such as high-density bone sites may also increase the risk of fracture during insertion due to over-torquing, which demands the identification of potentially dangerous areas predisposing to implant breakage (Dörsam et al. 2020; Leles et al. 2023). Failure of osseointegration was described as a more common incidence than implant fracture in the systematic review by Jawad & Clarke, being mainly attributed to overpreparation of the osteotomy site or poorer bone quality (Jawad & Clarke 2019). In these cases, the prosthesis continued to function on three MDIs.
As previously mentioned, MDIs are typically one-piece implants with a fixed abutment, which can tolerate a divergence of implants up to 40 degrees (Yilmaz et al. 2020). Nevertheless, they have a limited ability to correct improper angulation compared to standard-diameter implants, which incorporate multi-unit and angled abutments for positional adjustments. Due to this limitation, achieving parallel placement is essential for ensuring optimal prosthetic fit and minimizing mechanical complications. Misaligned MDIs can disrupt overdenture seating, increase stress on the peri-implant bone, and contribute to biomechanical complications such as excessive lateral forces (Shatkin et al. 2007). Furthermore, parallelism is particularly critical for the immediate loading of MDIs, as it promotes uniform load distribution and reduces micromovements that could jeopardize osseointegration (Šćepanović et al. 2015).
An essential factor to consider when planning an overdenture retained by MDIs is ensuring sufficient prosthetic space for proper attachment function and denture stability. The required vertical space for MDI attachments is comparable to other freestanding abutments, such as Locator systems. The prosthesis includes a secondary attachment component, consisting of a metal housing that contains the retentive element (Proteasa et al. 2015). In addition to the housing height, space must also be allocated for the acrylic base, denture teeth, and, if decided, a reinforcing metal framework, with a total vertical requirement of at least 8 mm (Sekinishi et al. 2015, Alaseef et al. 2022).
The most frequently reported technical complications are fractures of the overdenture (Enkling et al. 2020), typically near the matrices, which are frequently observed in studies where existing complete dentures are converted into overdentures (Kern et al. 2018). In such cases, reinforcing the denture with a small metal framework has been suggested as an effective solution (Enkling et al. 2020, Schenk et al. 2024).
Clinical case 1
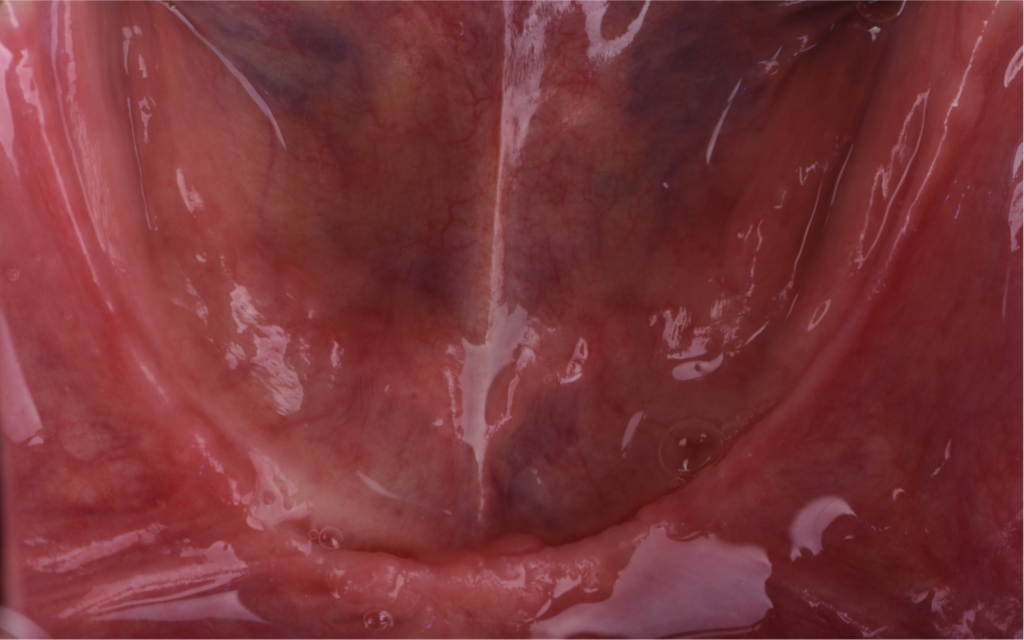
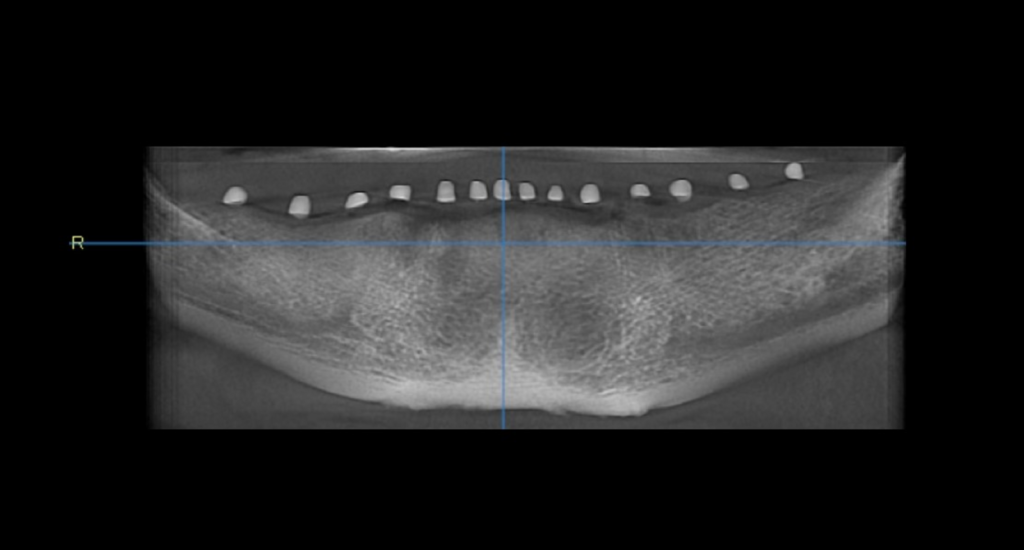
The following two cases were treated at the Implant Center, School of Dental Medicine, University of Belgrade. A healthy 70-year-old male patient was referred for the rehabilitation of his edentulous mandible, complaining about poor retention of his mandibular denture and discomfort during masticatory functions. Clinical and radiographic assessment revealed significant alveolar ridge resorption, restricting the feasibility of conventional implant placement. After discussing the available treatment options in detail, the patient decided to proceed with the placement of four mini dental implants (MDIs) to support a mandibular overdenture. (Figs 1-2)
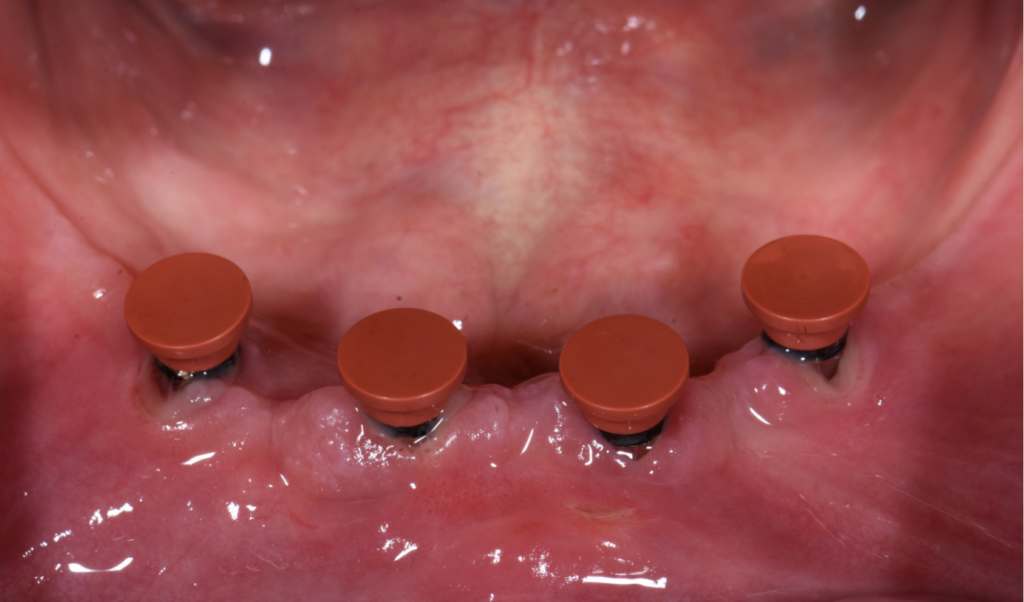
A flapless surgery for the installation of the MDIs was performed. Initially, the pre-determined implantation site was drilled with the ∅1.6mm Needle Drill (Institut Straumann AG, Switzerland), followed by the 2.2 mm BLT Pilot Drill (Institut Straumann AG, Switzerland). All implants were placed parallel with the help of paralleling posts (Institut Straumann AG, Switzerland). Insertion of the implant was initiated with the vial cap and the implants were placed into their final position manually with the help of Optiloc® Adapter (Institut Straumann AG, Switzerland). All implants achieved a minimum insertion torque of 35 Ncm, enabling the prosthetic protocol for functional immediate implant loading to be implemented. (Figures 3-10)







For the prosthetic procedure, transfer caps were placed on the implants and an impression was made using poly vinyl polysiloxane with a custom tray. Optiloc® model analogs were inserted into the Optiloc® impression copings, and master models were fabricated and mounted on the articulator and a metal reinforcement was planned to stabilize the overdenture. After the delivery of the denture, the patient was highly satisfied withits stability during function. (Figures 10-14)




Clinical case 2
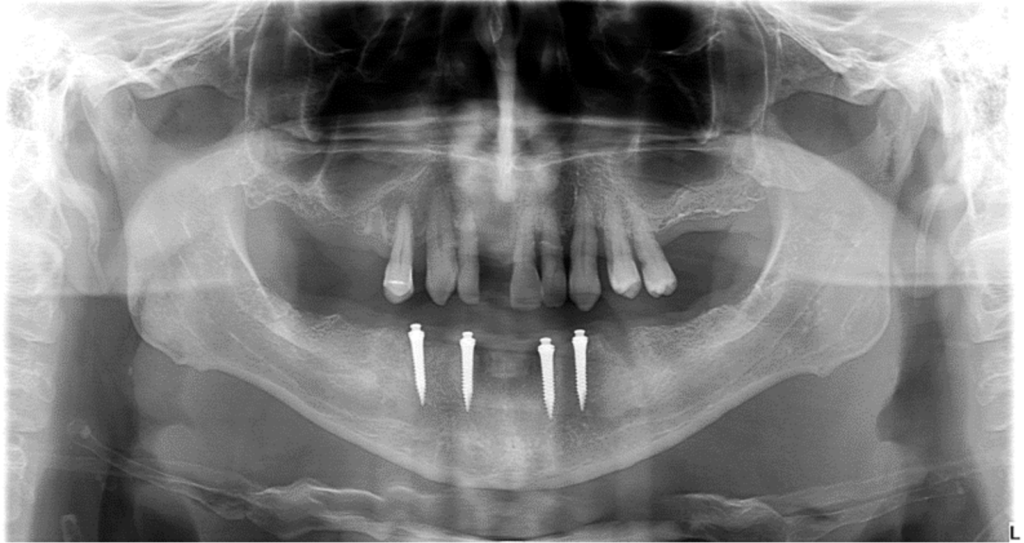
A healthy 62-year-old man was referred for the rehabilitation of his edentulous mandible, while the treatment plan for the maxilla involved the fabrication of a complete denture. At the time of assessment, the patient presented with no general medical contraindications and reported being a non-smoker. His primary concerns were to restore his masticatory function and the enhancement of esthetics. He had a preference for a time-efficient treatment plan that did not consider extensive surgical procedures. Given the reduced alveolar bone width and the patient’s preference for a minimally invasive approach, the placement of four MDIs was proposed (Figures 15-16).

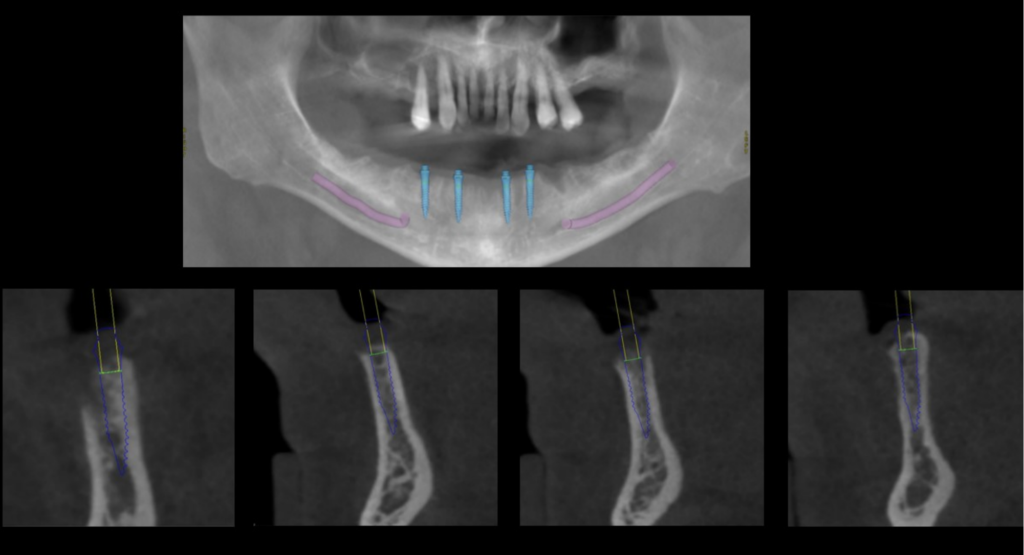
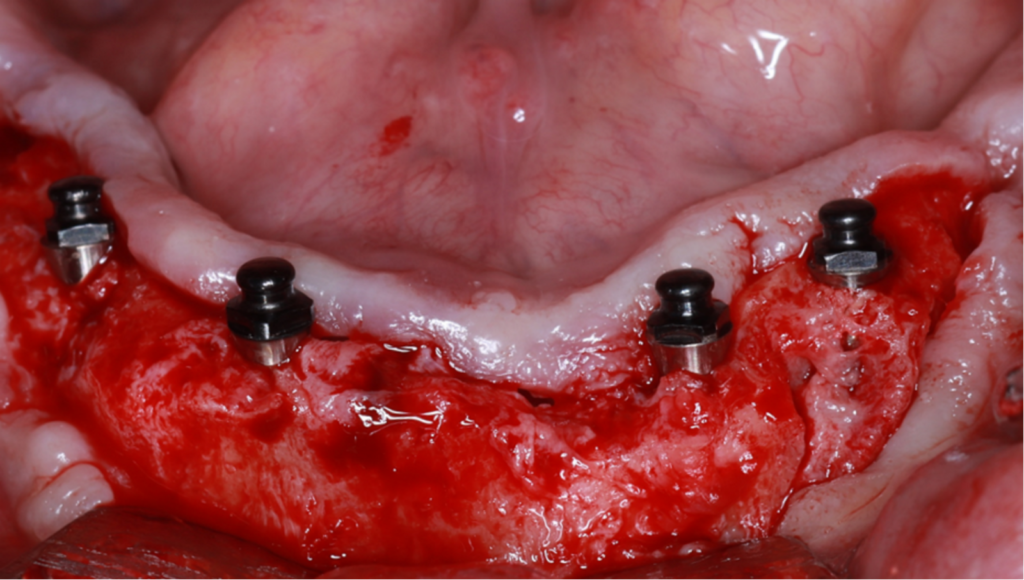
Due to alveolar bone discrepancies associated with post-extraction sockets, a crestal incision was performed and a full-thickness flap was raised. Subsequently, four one-piece 2.4-mm MDIs (Straumann® Mini Implant System, Institut Straumann AG, Switzerland) with a length of 12 mm were placed freehand in the inter-foraminal region, ensuring a minimum distance of 5 mm between the implants. A delayed loading protocol was followed due to lower torque values (<35 Ncm). (Figures 17-18).
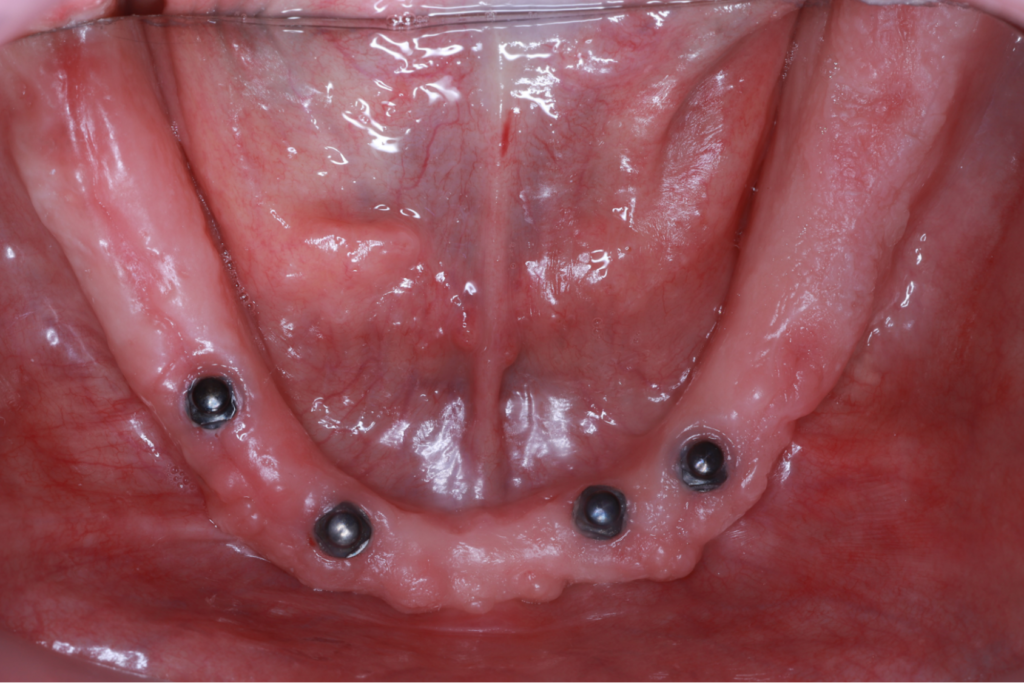
Following a 6-week healing period, the restorative process was initiated, and the IODs with the Optiloc® (Institut Straumann AG, Switzerland) retentive system were delivered to the patient (Figures 19-20).

Conclusions
Mini dental implants (MDI) retaining mandibular overdentures exhibit high survival rates, while offering several advantages such as a minimally invasive procedure, reduced treatment time at a more affordable cost. These advantages improve overall patient satisfaction in both esthetics and function. This suggests that MDIs are a reliable alternative treatment option, particularly in cases with resorbed mandibular alveolar ridge. However, further research is needed to evaluate the long-term clinical outcomes of MDIs retaining mandibular IODs.









