Introduction
As a result of the loss of the periodontal ligament and its vascular support, tooth extraction can lead to alveolar bone resorption, which is a physiological occurrence (Barootchi et al. 2022). It is estimated that two-thirds of this resorption takes place in the first three months, primarily due to the thinner thickness of the buccal plate (Araújo & Lindhe, 2005). Consequently, impairment of this vascular support in the anterior maxilla, a region with significant esthetic significance and delicate thin buccal bone, has pronounced implications (Araújo & Lindhe, 2005). The subsequent soft and hard tissue deficiencies, particularly in the esthetic zone, can restrict the ideal placement of implants and impair the overall esthetics of implant-supported prostheses (Siormpas et al. 2018).
Over the past 20 years, studies have investigated various methods to preserve bone after dental extraction, including immediate implant placement, soft tissue augmentation procedures, palatal orientation of the implant in the socket, platform switching design, and several socket preservation techniques. While each of these methods offers some beneficial effects for bone preservation, it is important to note that changes to the peri-implant tissues cannot be entirely avoided over time (Saez-Alcaide et al. 2021).
Authors have discussed the preservation of dental roots as means to prevent alveolar resorption, reporting esthetic effects while maintaining soft tissues (Salama et al. 2007). Based on this idea, Hürzeler et al. (2010) introduced a technique known as socket shield (SS). The goal of this technique is to maintain the bundle bone at its level on the buccal side by performing a partial root extraction. Following the same biological principle, the concept of partial extraction treatments (PET) was recently introduced by Gluckman et al. (2017) with the SS technique being the most popular form of PET.
PET, specifically the SS technique, offers several benefits over hard and soft tissue augmentation methods, such as requiring only one surgical intervention, resulting in decreased patient morbidity, and eliminating the need for additional costs associated with bone grafts or barriers. However, it is a delicate tactic that necessitates careful planning. Additionally, there is still a lack of long-term scientific evidence to fully support the clinical efficacy and biologic plausibility of the SS approach as well as a need for prospective randomized comparisons between the SS technique and the conventional immediate implant placement protocol (Atef et al. 2021).
The socket shield technique
Classification of partial extraction therapies (PET)
The concept of (PET) involves the decoronation of a tooth that can no longer be repaired or that is indicated for extraction. This way, the periodontal tissues that are connected to the remaining part of the root can still be preserved. PET are classified into four procedures according to Gluckman et al. (2016):
- Root submergence:
Tooth is decoronated to the level of the crest and soft tissue closure is achieved to ensure healing through primary intention. In order to successfully plan a pontic site beneath a conventional fixed partial denture (FPD) or an implant-supported FPD, the root must be free of apical disease or have already had successful endodontic therapy. - Socket shield (SS):
Consists of preparing a tooth that is intended for extraction at a site for immediate implant placement, often in the anterior maxilla. - Pontic shield:
Involves similar preparation as the SS with no implant placement. The extraction socket is grafted with a slow-resorbing bone substitute material. The socket must be sealed with a soft tissue graft and left to heal for a minimum of 3 months. Pontic pressure may gradually be applied to develop the site. - Proximal pontic shield: It is mainly intended for the preservation of interdental papillae with immediate implant placement of two or more adjacent implants.
Step-by-step procedure
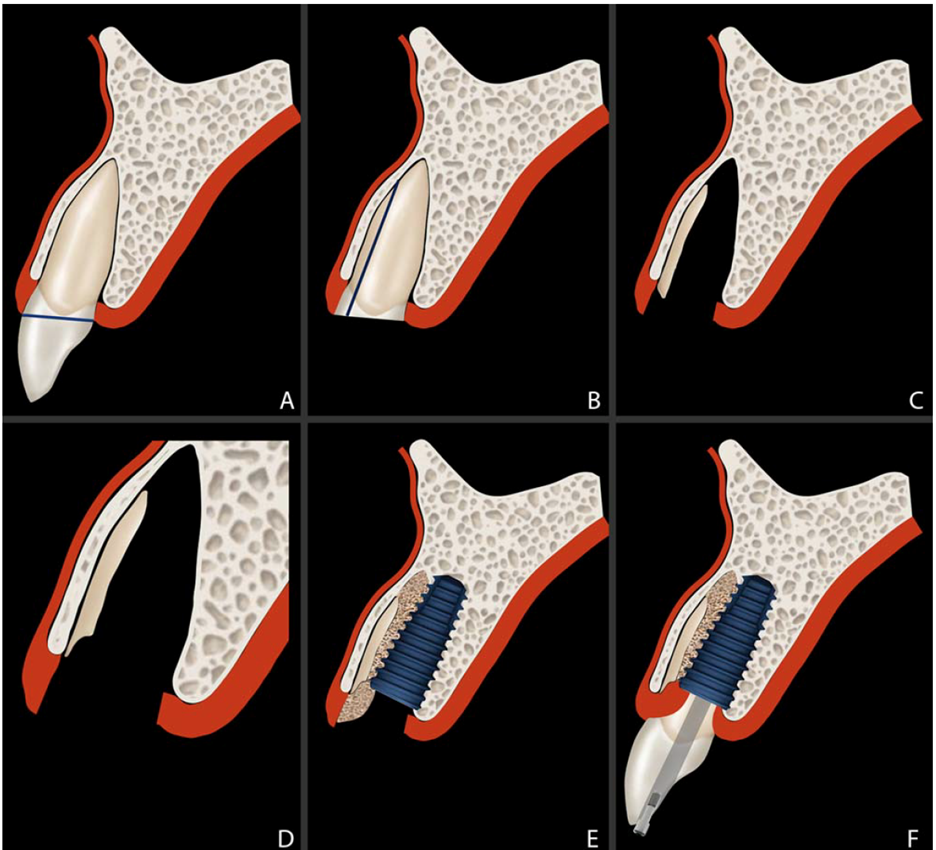
The technique is described by Gluckman et al. (2016) (Fig. 1):
- Following the administration of sufficient local anesthesia, the tooth is decoronated to the gingival level (Fig. 1A). The root is meticulously sectioned with a long shank bur longitudinally and mesiodistally halfway, using the canal as a reference point so that the labial and palatal halves are completely separated from one another from the coronal to the apical aspect (Fig. 1B).
- An endodontic file may be inserted into the canal to determine the direction of the root. Extreme caution must be exercised to avoid penetration into the mesial or distal adjacent tooth or bone. Periapical radiographs can be taken with the resection bur in place.
- Once the labial and palatal root halves have been adequately separated, the palatal root section is carefully displaced labially into the gap created. When introducing a microperiotome into the palatal periodontal ligament area, it is crucial to refrain from preparing the labial root, labial bone crest, or labial PDL space. Maintaining a finger rest on the buccal/labial ridge is crucial. This makes it possible to feel the drill location by touch when the apex is approached or if displacement of the socket shield or incomplete root sectioning occur. The palatal half should be gently elevated with a pair of micro-forceps (Figure 1B).
- The labial root segment that is still in place is probed on its inner side to check for immobility. Any infection remaining in the socket apex should be completely eliminated with saline irrigation. An irrigated big round diamond bur is then used to decrease and shape the coronal aspect of the root portion to 1 mm above the alveolar socket crest. To avoid damaging the gingiva, a gingival protector must be used (Fig. 1C). Experience has allowed the authors to reduce the socket shield to bone crest level to avoid complications (Gluckman et al. 2018).
- The labial root part is then reduced with a crescent-shaped concavity to match the labial appearance of the alveolus. Based on the clinician’s subjective judgement, the socket shield’s thickness is then assessed. A thick socket shield is stable but leaves no space for implant placement whereas an excessively reduced socket shield can be unstable. The thickness should be reduced by about half, according to the authors, from the root canal to the labial border. Most studies preconize a 1.5 – 2.0 mm thickness with a concave shape and an internal bevel of the shield (Kotsakis et al. 2023) (Fig. 1D). The apical root segment may remain thicker while the coronal segment becomes thinner.
- A periapical radiograph can be taken to evaluate the finished preparation and any necessary corrections be made. The socket shield is defined as the prepared buccal tooth segment ready for implant placement at its palatal aspect.
- If so intended, an immediate implant is then placed palatally to the socket shield after the preparation of the osteotomy site (Fig. 1E).
Indications
The SS technique is indicated in the following situations according to Gluckman et al. (2016):
- Unrestorable tooth crown or tooth indicated for extraction.
- Tooth root with or without apical pathology.
- Intention to preserve the alveolar ridge, specifically to prevent buccopalatal collapse.
- Immediate implant placement.
- Ridge preservation in conjunction with other PET.
Contraindications
It cannot be applied under the following conditions according to Mitsias et al. (2017):
- Present or past periodontal disease.
- Mobility or widening of the periodontal ligament.
- Vertical root fractures.
- Horizontal fractures below bone level.
- External/internal resorption.
Clinical Case
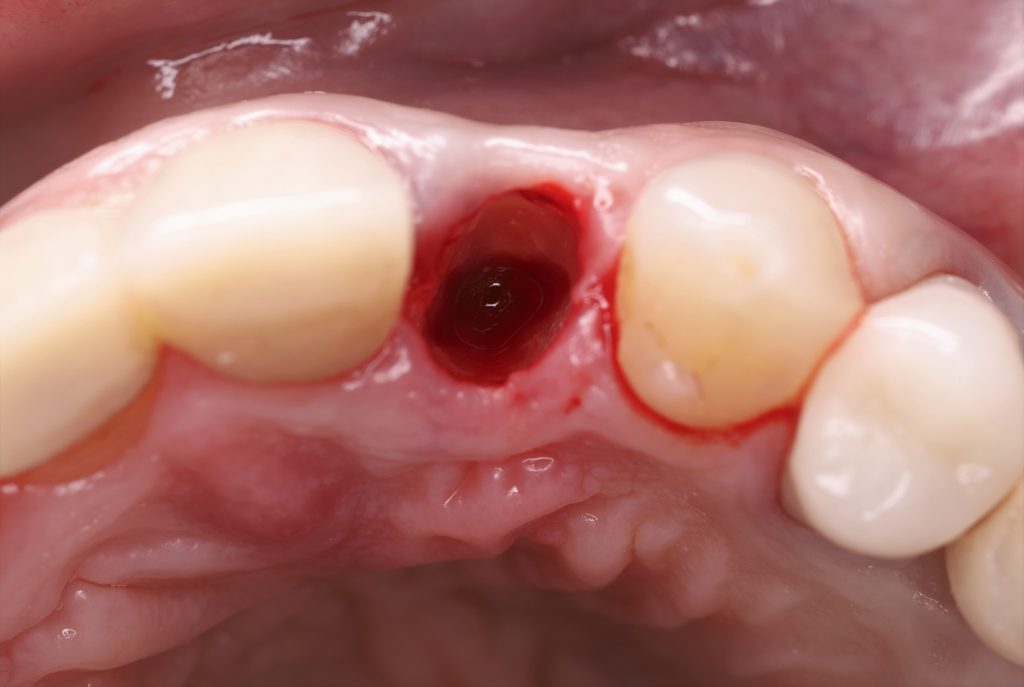
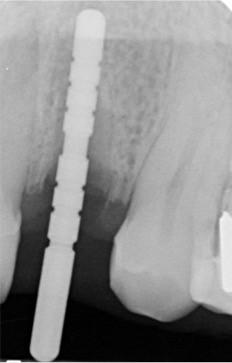
A 35-year-old, healthy, non-smoking male patient consulted with a repeatedly fallen crown on tooth #22 (tooth numbered by FDI World Dental Federation notation) (Fig. 2). Upon clinical and radiographic examination, the tooth had a poor prosthetic prognosis. After thorough investigation, it was decided to extract and replace it with an immediate implant. The CBCT sagittal cut revealed a buccal plate of 1mm thickness. Therefore, the case was treated using the SS procedure (Fig. 3). According to Gluckman et al. (2020), the presence of bone facial to the root must be verified.





After administering local anesthesia, a long shank root excision bur (Komet Dental, Germany) connected to a hydrated high-speed handpiece was used to dissect the tooth in a horizontal direction. After crown removal, the root was dissected in a mesiodistal manner along the long axis down to the apex. The root’s buccal and palatal segments were separated. The periodontal attachment holding the palatal fragment of the root to the socket was severed by inserting a periotome (Periotome #1, Nordent, USA) between the socket wall and the palatal fragment. The buccal segment was left intact while the palatal fragment was carefully removed.
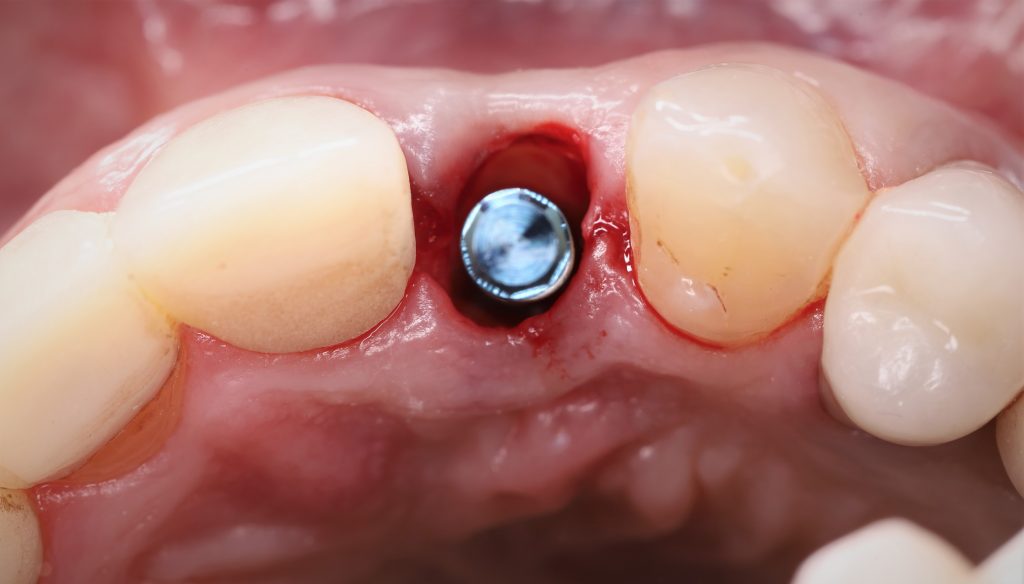
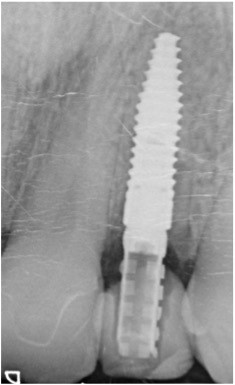
The buccal segment was carefully prepared apico-coronally and mesio-distally, providing a concave contour, then reduced to the level of the crest using a long shank round diamond bur (Komet Dental, Germany). With a pointed probe, the buccal shield’s stability was examined (Fig. 4A).
An immediate implant (Straumann® Bone Level Tapered Implant, NC 3.3 x 14 mm) was placed following successive osteotomy drilling in the palatal aspect of the socket (Figs. 4B, C, D, E, F). A deproteinized bone substitute of bovine origin (Bio-Oss, Geistlich Pharma,Wolhusen, Switzerland) was used to fill the gap between the implant and the shield. Using the patient’s own tooth, immediate temporization was carried out (Figs. 4G, H, I). The patient’s permanent crown was delivered 3 months later (Figs. 4J, K, L). After 1 year of follow-up, the patient presented with clinically stable results and positive soft tissue contour around the implant (Figs. 5A, B).










Complications of the socket shield technique
- Internal exposure of the socket shield: Considered as the most frequent complication of the SS procedure according to Gluckman et al. (2018). The coronal border of the shield and the subgingival contour of the crown should have enough space between them. A micro-flap is raised, the shield is trimmed to the crestal level, and any protruding edges are rounded off. To aid soft tissue closure, it is recommended to place a connective tissue graft.
- External exposure of the socket shield: Considered as the second most frequent complication of the SS procedure according to Gluckman et al. (2018). This is likely the result of the shield’s coronal aspect being overextended or the sharp coronal aspect piercing the soft tissue beneath. This often occurs where the facial bone is missing. A micro-flap is raised, the shield is trimmed to the crestal level, and any protruding edges are rounded off. To aid soft tissue closure, it is recommended to place a connective tissue graft.
- Implant failure: The shield’s stability is checked. If the shield is still intact, a new implant can be placed. The site can also be closed and left to heal before reevaluation as a pontic shield site. If the shield is unstable, it should be removed, and the implant replaced (Gluckman et al. 2018).
- Infection: Removal is essential whenever the infection is combined with mobility of the shield (Gluckman et al. 2017).
- Migration: Always necessitates the removal of the socket shield (Gluckman et al. 2017).
To fill or not to fill the gap?
Creating space between the root and the implant offers a twofold advantage: fostering new bone formation and mitigating potential complications. Placing the implant in close proximity to the root could increase the likelihood of implant failure by promoting tooth fracture. Therefore, it seems preferable to keep a space between the socket shield and the implant. However, there is still no agreement on whether or not to fill the gap.
According to Bäumer et al. (2015) in a pilot study conducted on beagle dogs, new bone formation was detected in the space between the root fragment and the implant surface without the use of any biomaterial. Bone is found in direct contact between the implant and the shield from the shoulder to the apical part of the implant. Junctional epithelium is only detected in contact with the root fragment in the coronal aspect. Mitsias et al. (2017) support the same concept, proving that the apical and medial thirds of the space between the shield and the implant are occupied by compact, mature bone. They state that it is a challenge to obtain such quality bone when using grafting material. Regarding the coronal third, non-infiltrated connective tissue was found and the absence of inflammation in this region can be viewed favorably. In observations of radiographic cross sections by Siormpas et al. (2014), the implant-root interface appeared to be delineated by a radiolucent line that was interrupted by areas of direct contact between the radiopaque root fragment and the titanium surface at either the coronal portion of the root fragment or the apical depending on the angulation of the implant in relation to the retained root fragment.
To fill the jumping distance of 2 mm or more, Hurzeler et al. (2010), Dayakar et al. (2018) and Gluckman et al. (2015) used xenograft material between the root part and the implant. It is recommended that grafts placed between the implant and shield be used carefully and only in situations where the gap exceeds 1 mm (Mourya et al. 2019).
Discussion
The outcomes of implants placed using the SS technique demonstrated comparable survival and success rate to those achieved with conventional immediate implants. A recent systematic review reported an implant survival rate of 98.6% with 9 implants failing out of 656 implants placed using the SS technique (Oliva et al. 2023). Bramanti et al. (2018) conducted a study involving 20 patients who received a single implant using SST, while another 20 patients underwent immediate implant conventionally. Both groups exhibited similar survival rates, but the SS group showed better marginal bone levels and Pink Esthetic Score (PES) values after a 3-year-of follow-up. In a one-year prospective clinical research, the implant survival rate was 100% in 30 individuals with 40 immediate implants with SS. There were no biological issues and few (2.5%) prosthetic complications (Gluckman et al. 2016). Similarly, a long-term assessment by another research team involving 250 implants in 182 patients over a 10-year period reported five implant failures yielding a cumulative patient-level implant survival percentage of 96.5% and a cumulative implant success rate of 87.9%, when considering mechanical and biological factors (Zuhr et al. 2020).
When it comes to hard tissue changes, (Siormpas et al. 2014) evaluated bone changes using radiography with only a 2-dimensional examination of spatial changes. The study confirmed crestal bone stability. The estimated mean bone loss was 0.18 ± 0.09mm and 0.21± 0.09mm, on the mesial and distal portions of the implants, respectively. Concerning buccal plate resorption, in a 6-month randomized clinical trial on 40 implants placed in the maxillary anterior jaw with the SS shield technique, the study group’s buccal plate experienced horizontal bone loss ranging from 0 to 0.26 mm, with a median value of 0.15 mm, and vertical bone loss varying from 0.11 to 0.55 mm, with a median value of 0.31 mm. However, the horizontal bone loss in the control group ranged from 0.03 to 0.44 mm with a median value of 0.32 mm, and the vertical bone loss ranged from 0.25 to 1.51 mm with a median value of 0.7 mm. A statistically significant difference was found in both the horizontal and vertical bone loss within each group and between the two groups. They concluded that the SS technique with immediate temporization can reduce the labial bone loss following tooth extraction (Abd-Elrahman et al. 2020). In a systematic review and meta-analysis, Lin et al. (2022) confirmed that implants treated with the SST achieve a better and more stable hard tissue profile compared to conventional IIP. MBL and changes in buccal bone width (cBBW) were reported less by 0.4mm and 0.19mm for implants treated with SS, respectively.
Regarding soft tissue changes, a recent retrospective study by Wang et al. in 2023 evaluating the clinical effect of SS technique for 5 years after immediate implantation and restoration in the esthetic area proved that this technique could maintain the gingival margin and labial alveolar bone and preserve the soft tissue contour with good esthetic outcome. Bäumer et al. (2017) conducted a retrospective pilot study with a 5-year-followup, investigating volumetric alterations that affect buccal soft tissues. The average amount of buccal soft tissue lost in the facial direction was 0.37 mm ± 0.18 with an average of 0.33mm ± 0.23 for mid-facial recession. With an average pink PES of 12, it was concluded that the SS is a promising technique for placing implants in the esthetic zone. In a systematic review and meta-analysis in 2021, Atieh et al. found that the SS technique can improve the soft tissue profile following immediate implant placement in the esthetic zone. They concluded that the buccal bone plate’s alterations in width and height, the levels of the peri-implant marginal bone, and the outcomes in terms of esthetics are all positively impacted by the SST in the short term.
Conclusion
Preserving the buccal portion of the root aids in maintaining the integrity of the buccal bone plate without interfering with osseointegration in immediate implant placement. The SS method requires significant surgical expertise while remaining minimally invasive. Regarding alveolar bone maintenance, marginal bone stability and esthetic outcomes of immediate implantation, it appears to be a proper procedure. However, further research is required to comprehensively comprehend the long-term outcomes and determine strategies for preventing complications when employing the SS technique.
List of abbreviations:
- SS: Socket shield.
- PET: Partial extraction treatments.
- FDI: Fédération Dentaire Internationale.
- CBCT: Cone-beam computed tomography
- PES: Pink esthetic score.







