Introduction
Insufficient bone volume is a common problem encountered during the rehabilitation of the partially/completely edentulous posterior maxilla with implant retained/supported prostheses. The pneumatization of the maxillary sinus may limit the bone support for dental implants following tooth loss along with loss of alveolar bone height. In such a scenario, gaining space to place an implant of appropriate dimension in an ideal position might only be possible after a sinus floor elevation procedure. Sinus floor elevation is frequently combined with the use of autogenous bone or biomaterials.
The patient’s health status, medical history, habits, and compliance need to be assessed as a part of the overall evaluation prior to sinus floor elevation surgery. Any systemic condition or medication that compromise the individual’s healing capacity or add to the risk of the surgical procedure should be duly noted. For instance, poorly controlled diabetes, patients on immunosuppressive therapies, and patients taking antiresorptive or anticoagulation medication should be treated with great caution after assessment of risk and benefits.
Contraindications for sinus floor elevation
The clinician should be aware of the following contraindications and risk factors related to sinus floor elevation.
- Absolute contraindications include radiation therapy including the maxilla, ongoing chemotherapy, antiresorptive medication for the treatment of bone malignancies, and the lack of compliance.
- Relative contraindications include patients with poor glycemic control (Glycaeted hemoglobin levels less than 5.7% implying no diabetes, 5.7% – 6.4% signals pre-diabetes, 6.5% or higher implies diabetes), or patients who are smokers and alcoholics. Patients with history of allergic rhinitis or chronic sinusitis may develop exacerbation of symptoms following sinus floor elevation due to increased mucus production and irritation of the sinus membrane from the implant or the graft material. Hence a previous consultation from an ENT specialist is recommended for the benefit of the patient. Smokers should be warned about the risk of failure of the procedure and encouraged to stop smoking or at the least cut down significantly before the surgery and during the healing period (Schwarz et al. 2015).
Risk factors
Treatment can only proceed when the patient has understood the following risks and given their explicit and continuing consent.
- Presence of teeth with chronic, acute, or apical periodontitis in vicinity of the maxillary sinus should be treated before the sinus floor is elevated.
- The presence of sinus septa and residual bone height less than 3.5 mm are the main risk factors increasing sinus membrane perforation rates. Smoking is also shown to increase the risk of membrane perforation, sinusitis, and wound dehiscence in sinus lift procedures (Schwarz et al. 2015).
- Lack of residual bone height might affect the primary stability of the implants. A staged approach might be beneficial in such situations whereby the implants are placed after implanted bone or biomaterial has healed sufficiently.
Pre-surgical evaluation of maxillary sinus
The risk factors indicate that an in-depth evaluation of the surgical site needs to be performed to ensure success in surgery. Radiographic imaging is vital to determine the sinus anatomy and develop the most appropriate treatment approach. According to few authors, intraoral and panoramic radiographs alone are not sufficient, and judgment should be based on computed tomography (CT) or cone-beam computed tomography (CBCT) (Chan et al 2014; Goller-Bulut et al. 2015; Rahpeyma & Khajehahmadi 2015; Rancitelli et al. 2015; Torretta et al. 2013).
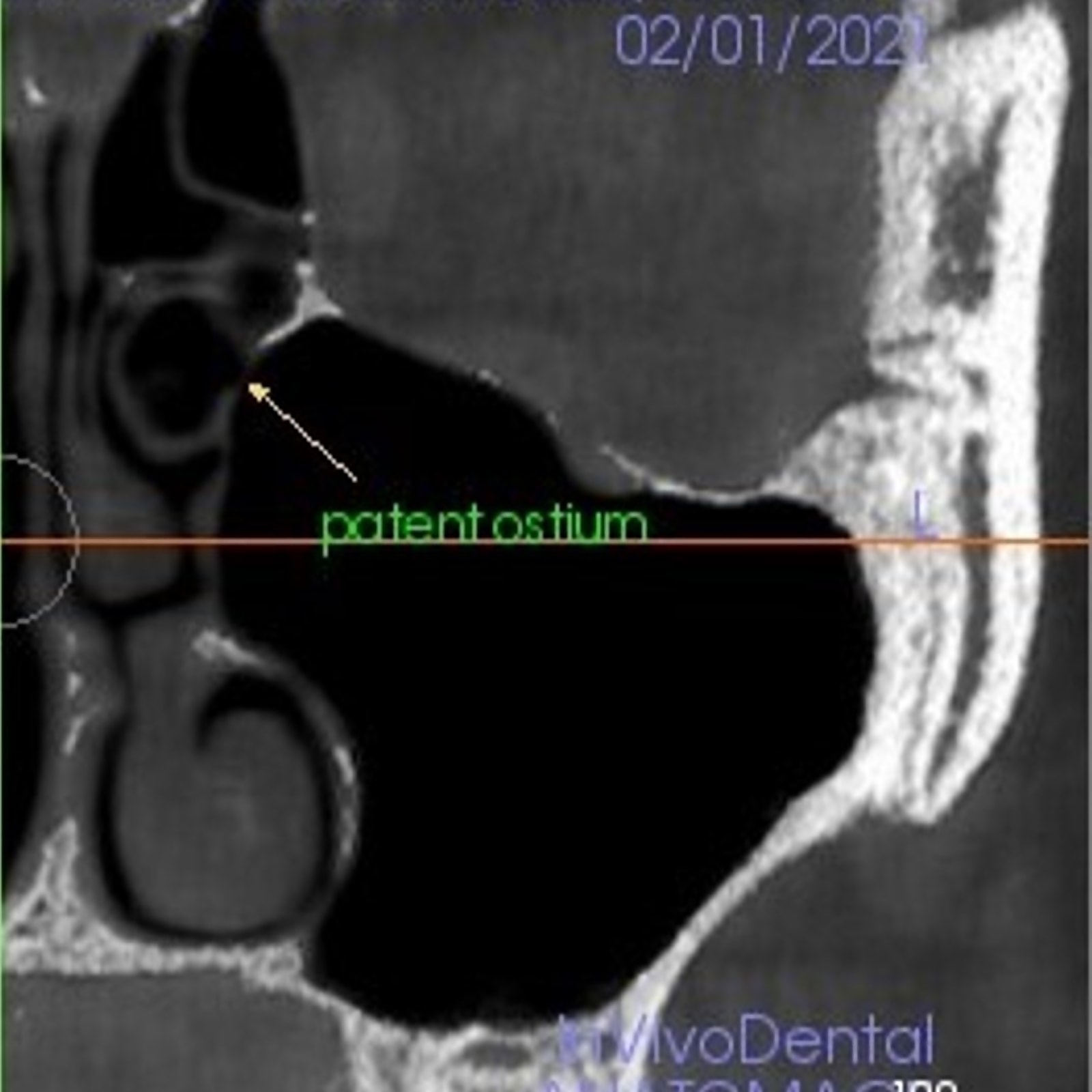
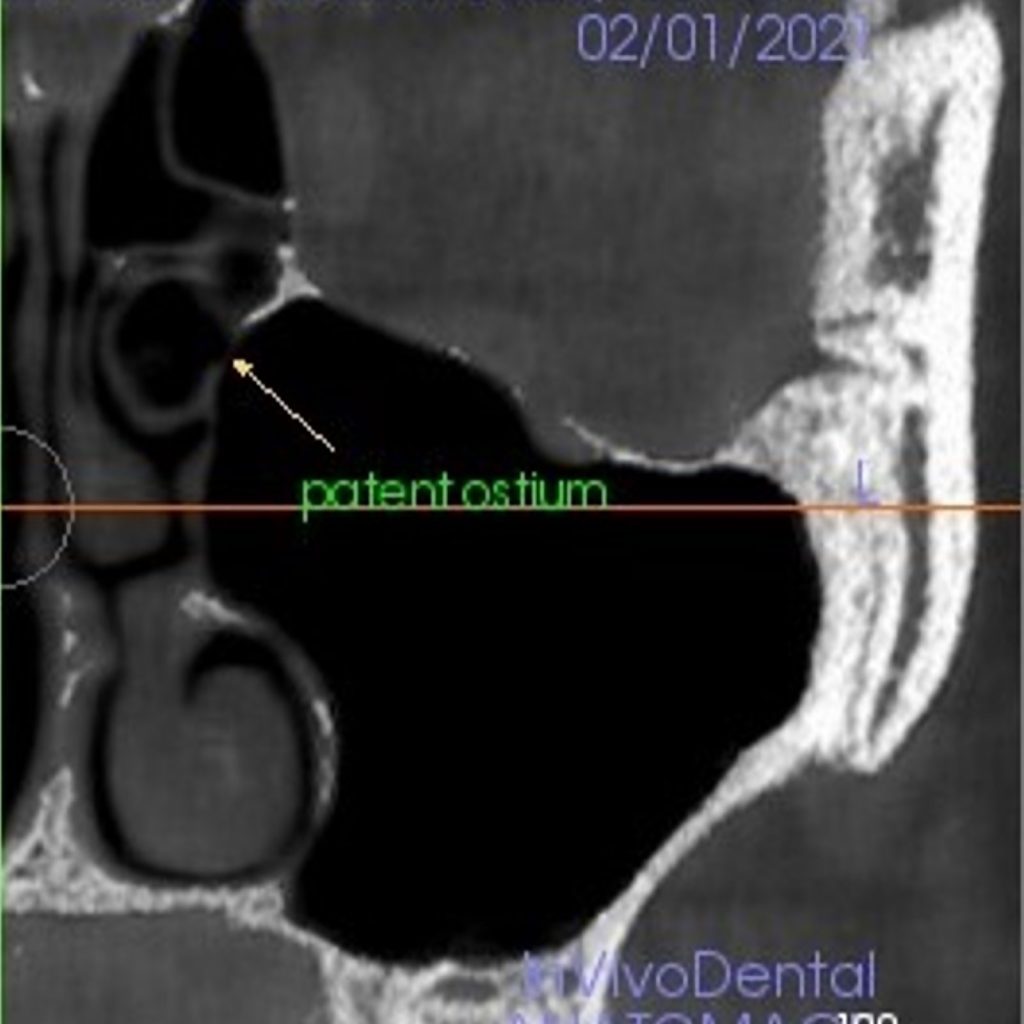
CT) and CBCT provide detailed three-dimensional images; however, CBCT is preferred as it involves a significantly lower effective radiation dose than conventional multi-slice computed tomography. Literature has shown that post-operative complications or pathologies are significantly less if the sinus floor elevation surgery is planned in the absence of ENT contraindications (Torretta et al. 2013). A healthy maxillary sinus is filled with air and radiolucent with a thin mucosal lining and a patent ostium which reflects correct muco-ciliary clearance (Fig 1) (Harris et al. 2012; Shanbhag et al. 2014).
According to Tavelli et al. (2017), the factors that need to be evaluated concerning the maxillary sinus are listed below:
- The thickness of membrane lining the sinus
- Presence of sinus septa
- The angle of the buccolingual maxillary sinus wall
- Presence of teeth/implants approximating the sinus floor
- The thickness of bone on the buccal side
- Residual alveolar ridge height and width
- Width of the sinus
- Presence of alveolar antral artery
The thickness of the membrane lining the sinus
Different values of average sinus membrane (Schneiderian membrane) thickness are reported in the literature, with variations seen among individuals. Some studies consider a membrane thickness up to 1 mm as physiological while membrane thickness exceeding 4 mm as pathological, since thickened sinus membranes have also been observed in asymptomatic patients (Rancitelli et al. 2015; Aimetti et al. 2008; Cakur et al. 2013).
Studies employing CBCT have demonstrated the thickness of the membrane in a physiologically healthy state to range from 0.8 to 1.99 mm. According to a study published by Wen et al. (2015), the chances of perforation increase if the thickness of the membrane is less than 0.5 mm or greater than 3 mm (Wen et al. 2015). A favorable thickness was concluded to range from 1.5 to 2 mm. There is an increased risk of sinusitis after sinus floor elevation, for membrane thickness over 2 mm, with a greater risk of ostium obstruction for value over 5 mm. If the thickness of the sinus membrane exceeds 5 mm, it shall be deemed inoperable unless otherwise stated by the ENT specialist.
Presence of sinus septa

Sinus septa, also known as Underwood’s septa, vary in shape, position, and development and are known to be present on the maxillary sinus floor in around 38% of the population (Rancitelli et al. 2015.Their presence is generally considered to increase the chances of membrane perforation during sinus lift procedure.
Sinus floor elevation becomes complicated if sinus septa are incomplete or run longitudinally, compared to a transversal orientation. The absence of sinus septa is considered a favorable situation.Various modifications in surgical approaches have been suggested to reduce the rate of perforation in the presence of sinus septa, including preparation of a wider window during lateral window approach or preparation of two separate windows on each side of a septum (Beretta, et al. 2012; Jung et al. 2019). The key to a successful sinus floor elevation procedure would lie in proper preoperative assessment leading to localization of the septae and formulating a plan to minimize possible complications.
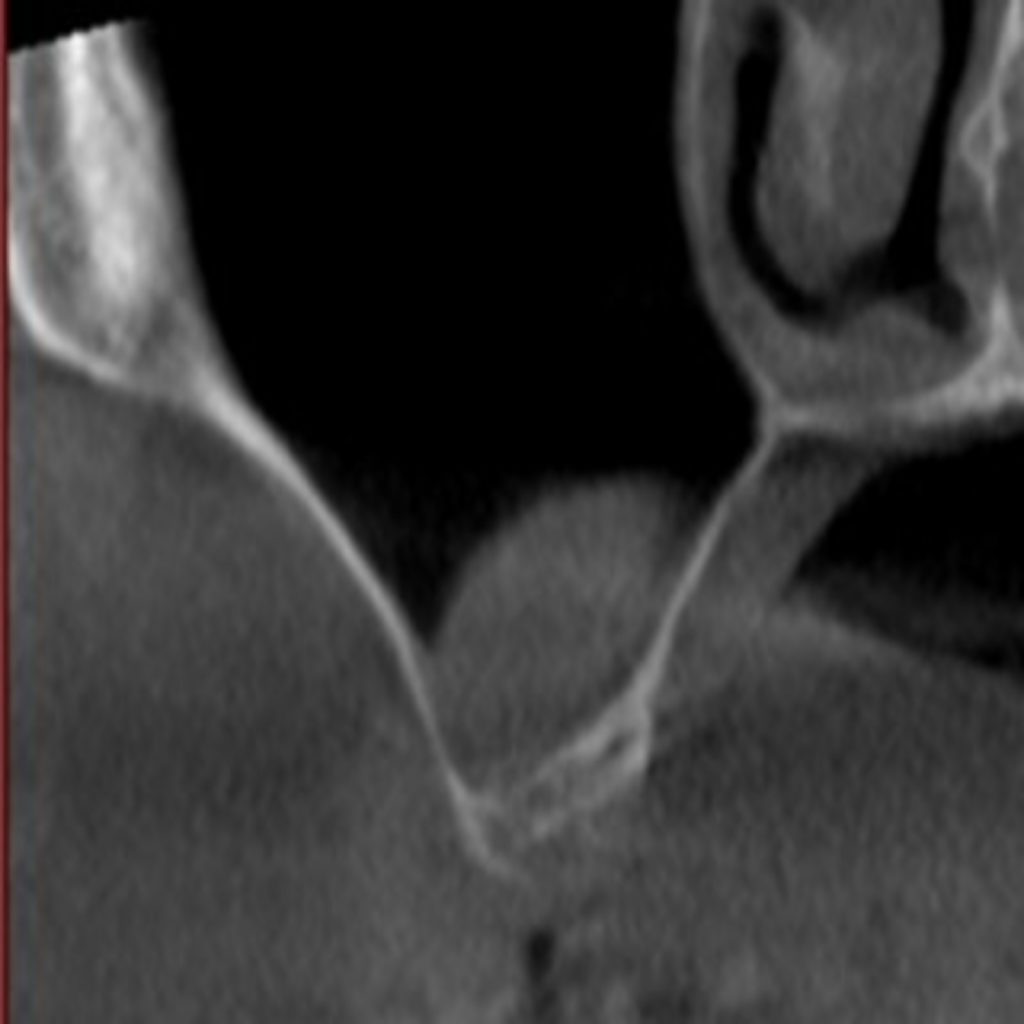
The angle of the buccolingual maxillary sinus wall
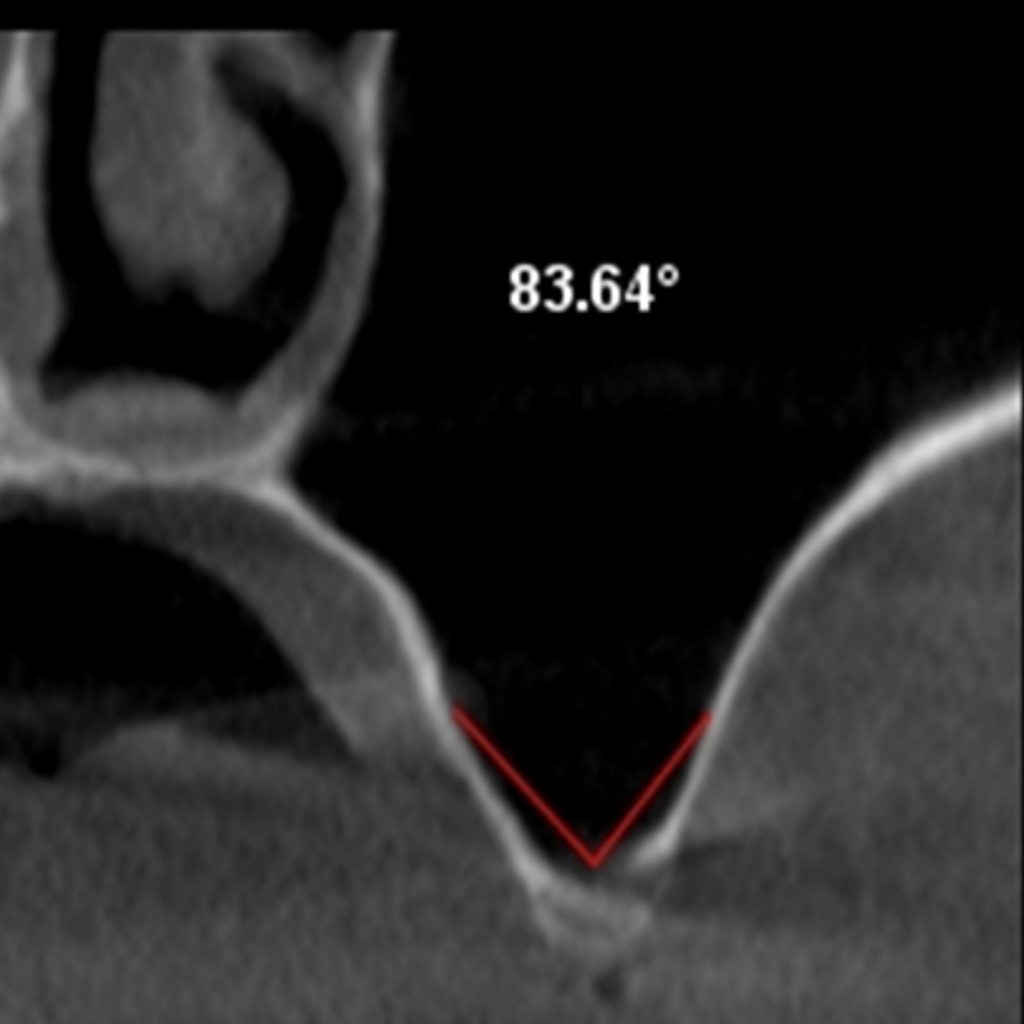
The buccolingual angle of the maxillary sinus is defined as the angle formed between the palatal and vestibular walls of the sinus. According to a study conducted by Cho et al. (2001), the chances of perforation are highest when this angle is less than 30 degrees. The chances of perforation reduce when the angle is in range of 30 to 60 degrees (commonly seen), with the chance of perforation almost zero if the angle is larger than 60 degrees (Cho et al. 2001). When the clinician opts to perform a sinus lift procedure utilizing the lateral window technique, in cases where the angle is less than 30 degrees, it is recommended to place the mesial margin of the window anteriorly. A study by Velloso et al. (2006) established that the steeper angles are in the vicinity of the second premolar, and the chances of perforation were higher in the anterior region of the sinus (Velloso et al. 2006).
Presence of teeth/implants approximating the sinus floor
The loss of the alveolar ridge and an increased sinus pneumatization are seen as a consequence of tooth loss in the posterior maxilla. Furthermore, it was found that the dentition status influenced the location of the posterior superior alveolar artery and the ease of reflection of the sinus membrane (Velasco-Torres et al. 2016). When intimate contact occurs between the roots of the teeth and the sinus membrane, especially in single missing posterior teeth, the chances of perforation increase. This is due to the irregular sinus floor morphology with indentation in a small area. A favorable clinical situation would be a wider edentulous area with missing teeth in the posterior maxilla.
The thickness of bone on the buccal side
Studies have established that the mean maxillary buccal bone thickness for the partially and completely edentulous, in the area between the premolar and molars, is around 1.5 – 2 mm (Monje et al. 2014; Yang et al. 2012). The buccal bone thickness is generally seen to increase from the premolar to the molar region. The thickness of buccal bone should be estimated correctly since it has a bearing on the technique employed, and the correct detachment of the membrane from the overlying bone.
A thin buccal bone of less than 1 mm thickness is considered favorable since it allows both variants of lateral wall sinus elevation (trap door/complete removal of lateral bone) to be performed. It is preferable to utilize piezoelectric or ultrasonic cutting inserts directly in the case of thin buccal bone. Buccal bone with a thickness greater than 2.5 mm is considered unfavorable with increased chances of perforation of the Schneiderian membrane.
Residual alveolar ridge height and width
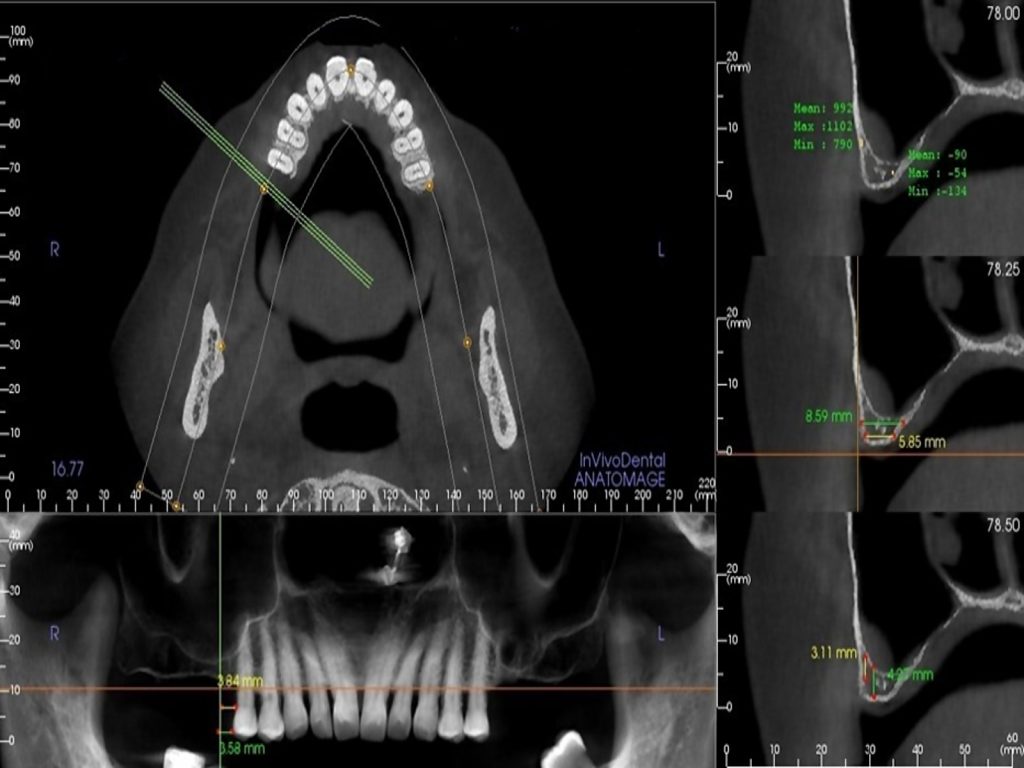
The factor of residual ridge height has been linked to the sinus membrane thickness and prognosis of implant treatment following sinus floor elevation. A thinner sinus membrane is observed at sites with reduced residual ridge height, implying that the chances of perforation during the sinus lift procedure are high. A residual ridge height of 4 mm or less is considered severely deficient, and a sinus floor elevation utilizing the lateral window approach is recommended. If the residual ridge height is 2 mm or less, it is considered to be a challenging or unfavourable situation (Testori et al. 2012; Yilmaz & Tozum 2012).The residual ridge width influences the diameter of implants and the probability of placing the implants along with the sinus floor elevation. It is suggested that at least 1.5 mm of bone should surround the implant to provide crestal bone stability and reduce marginal bone loss (Berglundh & Lindhe 1996; Esposito et al. 1993; Hermann et al. 2001; Tarnow et al. 2000).
Width of the sinus
Kamrody et al. (1977) established that, on average, the volume, height, and width of a maxillary sinus were 15 ml, 23, 25 and 34 mm, respectively (Karmody et al, 1977).A classification for the maxillary sinus width was proposed based on the upper and lower boundaries during sinus floor elevation utilizing the lateral window technique (Chan et al. 2014).
Kutkut et al. (2011) demonstrated that narrow sinus width was accompanied by better healing outcomes and bone regeneration than wide sinuses, and was considered favourable (Kutkut et al. 2011).
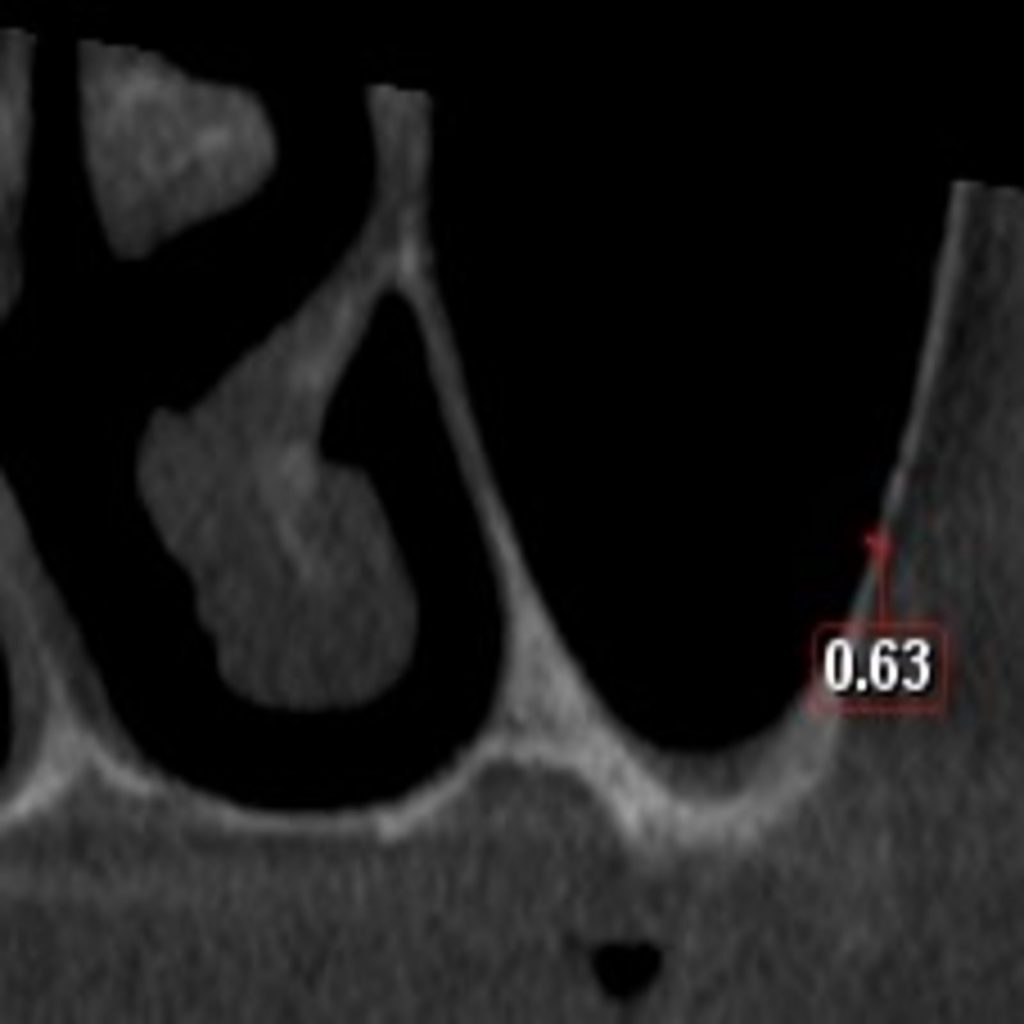
Presence of alveolar antral artery
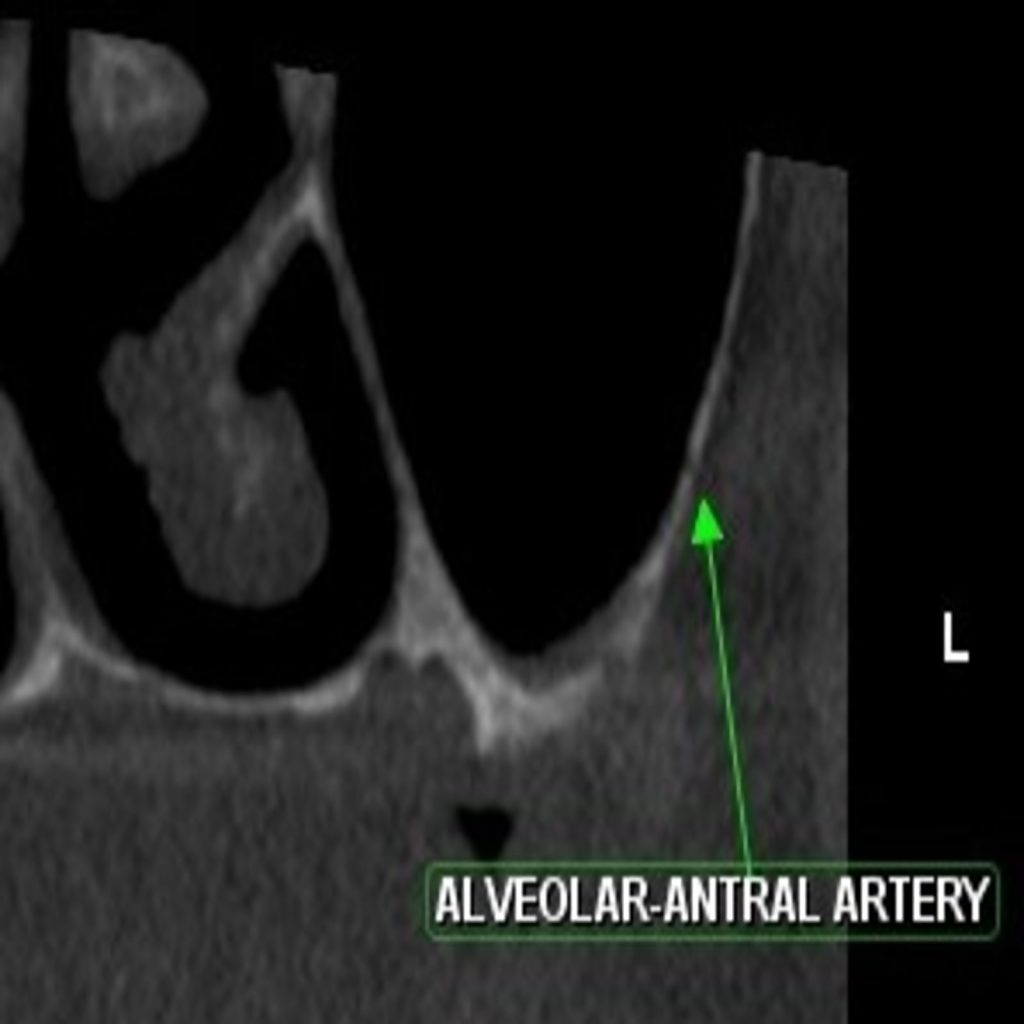
The intra-osseous anastomosis, also known as the alveolar antral arteries, is an anastomosis between the posterior superior alveolar artery and infraorbital artery. Since, hemorrhage is a frequent complication during sinus lift procedures, it would be prudent to ascertain the presence of the alveolar antral arteries at the site of the proposed osteotomy. In 2016, Valente ressviewed the existing literature on the alveolar antral artery and concluded that the vessel’s course would mostly be intra-osseous, with a diameter of less than 1 mm on most occasions (Valente 2016). Valente also reported that the mean distance of the vessel from the alveolar ridge and sinus floor was 11.25 – 26.90 mm and 5.8 – 10.4 mm, respectively. To avoid hemorrhaging during surgery, precautions range from visualization of the artery using CBCT (cone beam computed tomography) before surgery, modifying the lateral window technique, and limiting the superior border of the lateral window to 18 mm from the residual ridge (Güncü et al. 2011; Maridati et al. 2014) . If the alveolar-antral artery cannot be detected radiographically or its diameter is 1 mm or less, it is considered a favourable situation. If the diameter is greater than 2mm, it is unfavourable for the operating clinician since the chances of profuse bleeding are higher during the procedure.
Conclusion
Sinus floor elevation is a predictable surgical procedure. However, patient evaluation and selection are critical for a successful outcome. The potential risk factors need to be identified after analyzing the anatomical structures for formulating a sound treatment plan.
Discover more about this topic: