Introduction
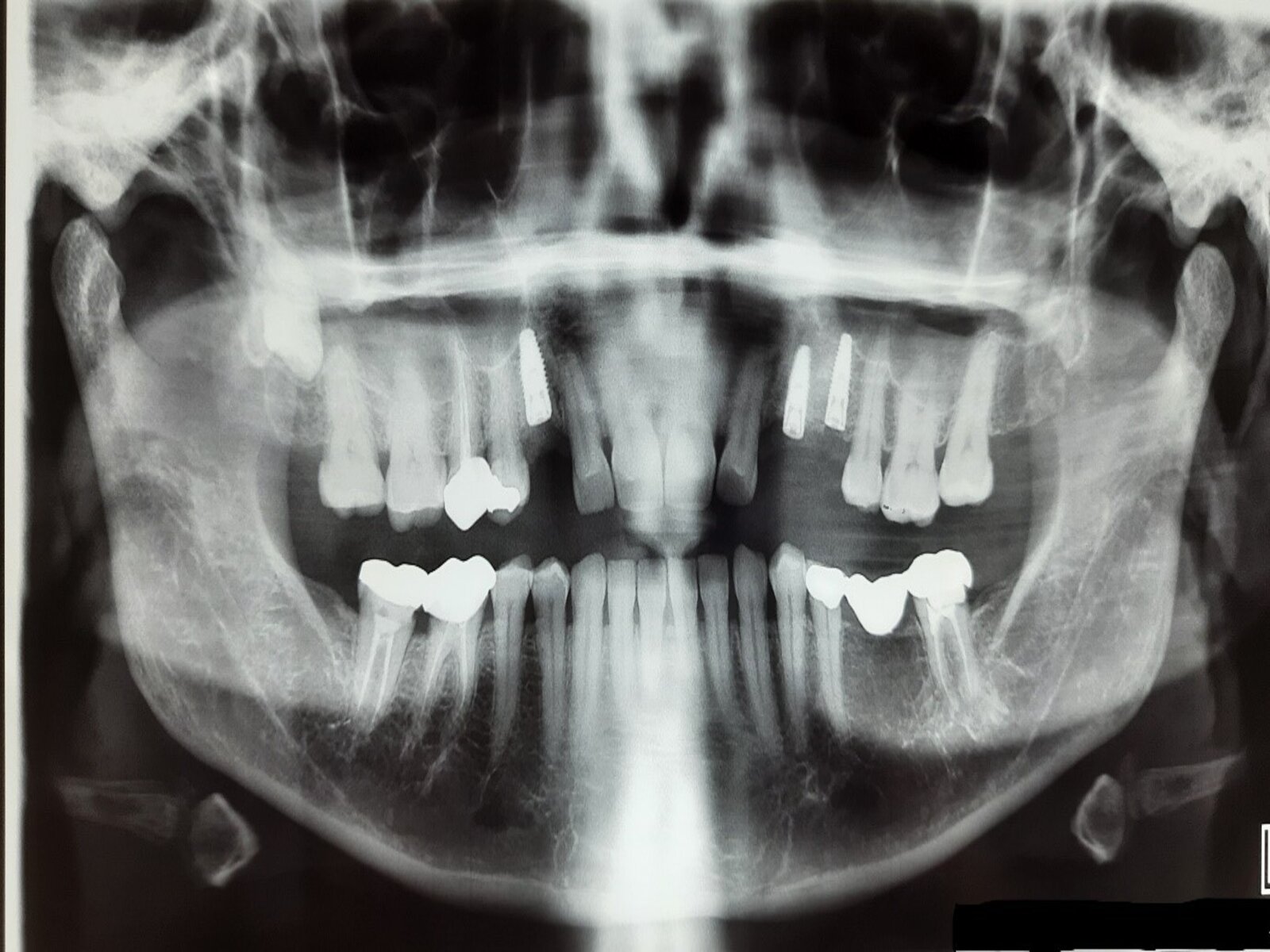
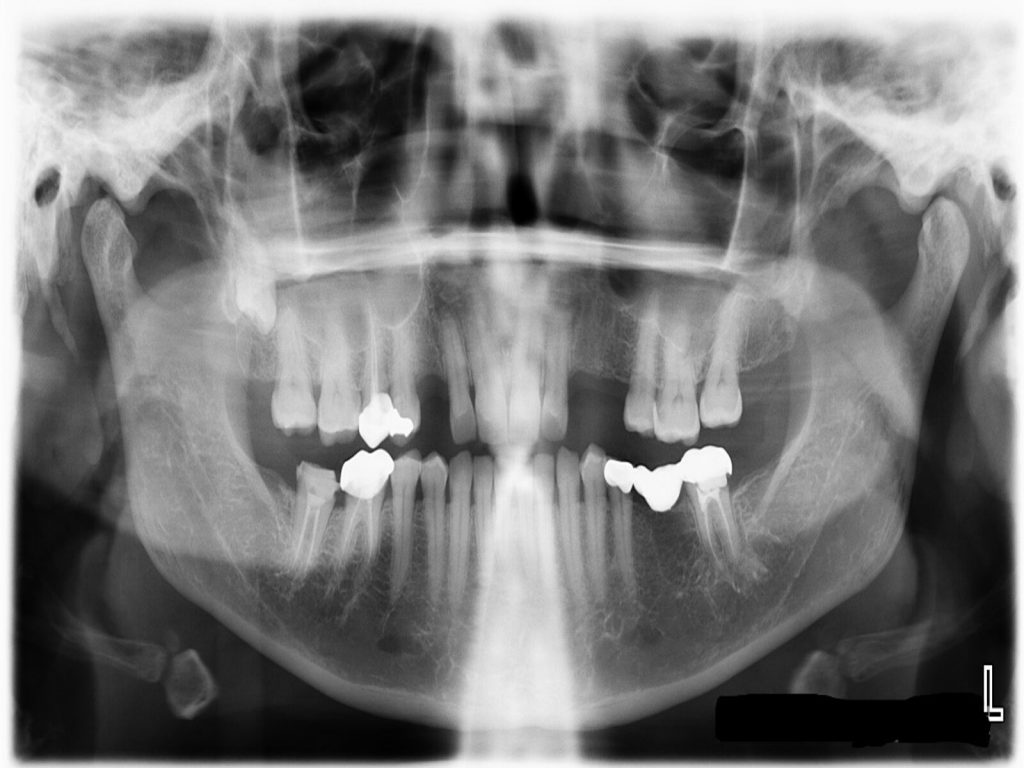
Insufficient bone volume is a common problem faced during the rehabilitation of the edentulous posterior maxilla with implant-supported prostheses. The bone available for implant placement in the posterior maxillat may be limited by the pneumatization of the maxillary sinus following tooth loss, resulting in unfavorable alveolar ridge dimensions. In the literature, low success rates were documented for implant restorations in posterior maxilla. These can be attributed to poor bone density, complicated anatomy and loading protocols favoring shorter healing periods (Adell et al.1991, Jaffin & Berman et al. 1991). The low success rates can also be attributed to the use of longer implants, and practice of bicortical anchorage by implant dentists (Bahat 1993). In the third part of this blog article, we will be covering the treatment options available for implant restorations in the posterior maxilla with insufficient bone.
Approaches to the sinus floor elevation procedure
The sinus floor elevation procedure can be performed using either a transcrestal approach or lateral window method. When a transcrestal approach is utilized, the sinus floor is elevated through the prepared implant bed. If the lateral window technique is employed, a full thickness flap is raised in the premolar-molar region, a window is prepared on the lateral sinus wall, the bone on the window retained or discarded, the sinus membrane lifted and finally augmentation material placed between the bony maxillary sinus floor and the lifted sinus membrane. The implant may be placed simultaneously along with the sinus lift procedure as in a one-stage technique or delayed as in a two-stage technique. A brief outline of the techniques, along with intra- and post-operative complications are highlighted in the sections below.
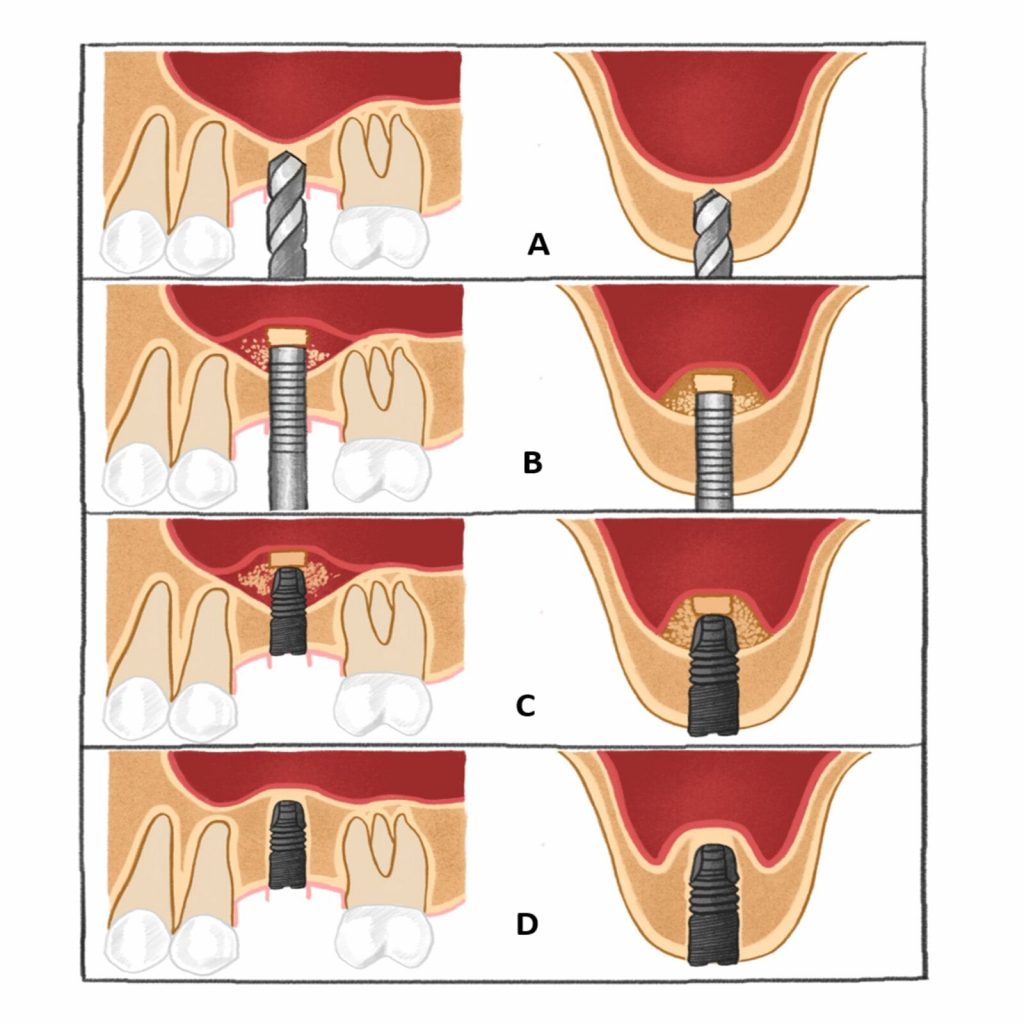
A = the site is prepared with a series of osteotomes with increasing diameter to a depth approximately 1-2 mm away from the maxillary sinus floor boundary.
B = an up-fracture of the maxillary sinus floor is made using a mallet under light tapping and the sinus membrane with the maxillary sinus floor is carefully elevated with the osteotome.
C = the implant is inserted at the prepared site, with the implant tip exposed in the lifted area.
D = new bone formation around the implant tip.
Transcrestal technique
The transcrestal approach was described by Summers in 1994 and is based on fracturing the sinus floor employing osteotomes or burs. Since the sinus floor is elevated through the prepared implant osteotomy site, the sinus floor is fractured using concave oe convex tipped osteotomes. The augmentation material/bone graft material is then introduced into the space beneath the elevated sinus membrane. Simultaneous implant placement is required to maintain the graft in place. Two clinical conditions should be met for the selection of this technique: Firstly, the sinus floor should be flat in the mesio-distal and bucco-palatal direction, and secondly, the residual ridge should be sufficiently wide and at least 6 mm high to ensure primary stability after implants are placed using the transcrestal technique. This technique permits the elevation of the sinus floor by a modest 2-4 mm.
In some cases, where the desired elevation of the sinus floor is less than 2 mm, use of graft material is considered optional. The implant supports the sinus membrane like a tent pole, and the space occupied by the coagulum is later replaced by bone as healing progresses (Lundgren et al. 2017). The main advantage of utilizing a graftless approach is reduced chairside time, less expensive treatment, and, in the case of undetected perforations, less probability of the graft material entering the sinus. However, the absence of graft material during the initial healing period does not imply a shortened healing time (Buser et al. 2017). Graft material is recommended in situations where the elevation of the sinus floor/gain in bone height exceeds 2 mm.
Bone augmentation is performed using autogenous bone material, bone substitutes or a mixture of both. Autogenous bone can be harvested from intraoral or extraoral sites. However, it is beneficial to harvest the bone from intraoral sites in the vicinity of the surgical site to reduce morbidity and treatment costs, and avoid an additional surgical site. The greater the proportion of the autogenous bone material, the greater the rate of new bone formation. The main benefit of mixing autogenous graft material with bone substitutes with a low replacement rate is that it maintains the volume of the augmented site over a longer period of time. A radiographic study, conducted by Pjetursson & Ignjatovic et al. (2009), assessed the intra-sinus vertical alveolar bone gain after osteotome-mediated sinus floor elevation and simultaneous installation of implants. They found significant bone gain with a grafting material compared to situations where no graft material was used. A 10-year prospective radiographic study by Nedir & Nurdin et al. (2016) found that the intra-sinus new bone formation was only 3 mm without the use of a graft material, and bone formation was more pronounced during the first year with increases seen for up to three years.
Various systematic reviews and meta-analyses, assessing implant survival after osteotome-mediated sinus floor elevation and simultaneous installation of implants with or without the use of a graft material have revealed an implant survival rate higher than 90% (Shi et al. 2016; Chen & Shi 2017).
Risk factors
The risk factors discussed in the first part of this blog article also apply in this context. The transcrestal approach is preferable if the sinus floor is relatively horizontal, since an oblique shape, or the presence of a sinus septae can increase the chances of membrane perforation. Other factors known to contribute to complications are poor bone density in the proposed area of sinus lift, the presence of pathological/inflammatory conditions resulting in a thickened sinus membrane or habits like smoking (Schwarz et al. 2015). The presence of bone with poor density at the proposed site interferes with primary stability and could result in early implant loss. To address low bone density, modifications in the osteotomy site or the implant design are made to enhance primary stability. Transcrestal sinus floor elevation is more safely performed in cases where the sinus membrane exhibits mild thickening. However, any infective condition contributing to the thickening of the sinus membrane should be ruled out to minimize complications during and after surgery. Although smoking is not an absolute contraindication, there is a higher risk of intraoperative and postoperative complications (Schwarz et al. 2015).
The transcrestal technique for sinus floor elevation is a predictable technique with a low incidence of intra-operative and post-operative complications. However, this depends on the careful screening and selection of the patient after identification of risk factors. Despite appearing to be less difficult, it should only be performed by experienced surgeons since a lateral window approach is the alternative in the event of any complications resulting from perforation or ingress of graft material inside the sinus (Katsyuma & Jensen 2011).
Intra-operative complications
The most common complication of transcrestal sinus floor elevation is sinus membrane perforation. Although, the incidence of membrane perforation has been reported to be between 0 and 21.4%, it may be underreported due to the closed nature of the transcrestal approach (Tan WC et al. 2008). Hence, it is important to verify or confirm the integrity of the membrane using the Valsalva maneuver or endoscopy. Apart from its invasive nature, the use of a fiberoptic endoscope, though accurate, lacks feasibility in routine clinical settings. Usually the membrane perforations are small in size. It is essential to detect them since the augmentation material can disperse into the sinus cavity through the perforation. The options for managing perforations are limited to repair using a collagen membrane placed through the osteotomy site. In cases where large perforations are detected, abortion of the procedure and repairing the site using a lateral window technique is advocated. If the procedure is aborted, the clinician can make another attempt after an interval of 3 to 6 months. Other complications seen in relation to the transcrestal technique involve loss of primary stability and hematoma due to rupture of the posterior superior alveolar artery during the sinus floor elevation procedure (Pjetursson & Lang 2014).
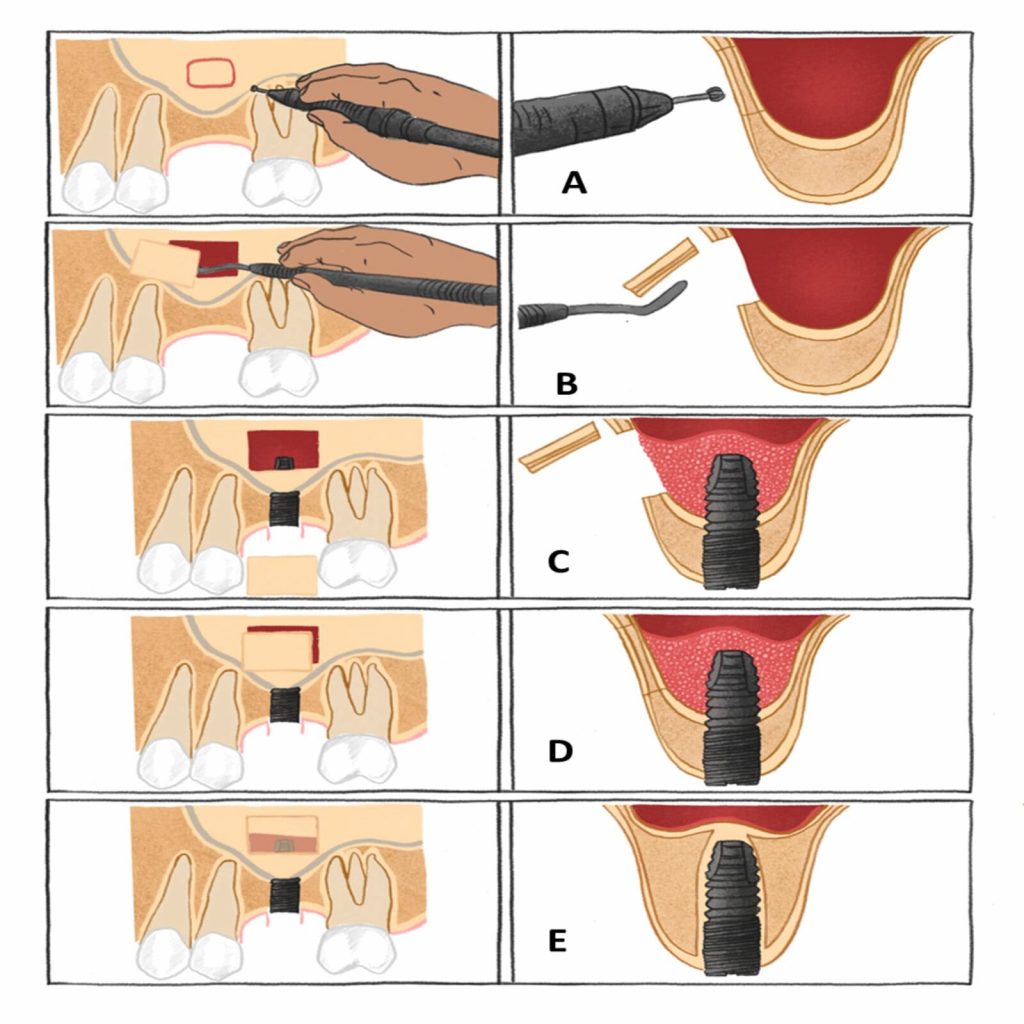
A = trapdoor osteotomy is performed on the lateral wall of the maxillary sinus.
B = the lateral cortical bony window is dissected free and removed from the underlying Schneiderian membrane, which is carefully elevated from the maxillary sinus floor to create a compartment for placement of the implant.
C = a blood coagulum is formed around the exposed implant tip in the secluded compartment between the elevated Schneiderian membrane and the original floor of the maxillary sinus.
D = the window to the maxillary sinus is covered by the dissected lateral cortical bony window.
E = new bone formation around the implant tip in the previous created compartment
Please note: In case grafting is planned, the trapdoor can be infractured, sinus floor membrane carefully dissected and elevated from the maxillary sinus floor to create space for placement of the graft material. The implant placement can be performed simultaneously with augmentation material tightly packed around the implant.
Lateral window technique
The lateral window technique for sinus floor elevation was introduced in the 1980s and has become a standard technique (Boyne & James 1980; Tatum 1986). In this procedure, a full-thickness mucoperiosteal flap is elevated to gain access to the lateral wall of the sinus. Subsequently a window is prepared in the lateral sinus wall, employing high speed surgical burs, and the sinus membrane is gently elevated to allow for the placement of the augmentation material into the maxillary sinus. Although the principles of the technique have not changed since it was introduced, the introduction of piezoelectric instruments has led to a few modifications in an attempt to reduce intra- and post-operative complications (Wallace at al. 2007).
The lateral window technique can be performed along with simultaneous placement of implants. An implant site is prepared to receive the implants in a manner such that the implant body is visible in the compartment created in the maxillary sinus. The graft material is then densely packed around the exposed implant body to expedite bone formation. The lateral window to the maxillary sinus is then covered with a resorbable collagen membrane to prevent ingrowth of fibrous tissue. A systematic review by Pjetursson et al. (2008) showed better implant survival in patients where the lateral window had been covered by a membrane. If primary implant stability is less than optimum or compromised, implants are inserted 4 to 12 months after the augmentation step. The final prosthetic solution is then performed 3 to 6 months after the implant placement procedure. Although simultaneous implant placement would be beneficial to the patient in terms of a reduction in the number of surgical appointments, it is dependent on the quality and quantity of bone available coupled with the potential implant dimensions and preparation of the osteotomy site. When the available ridge height is less than 4 mm and the ridge width is less than 6 mm, implant placement is delayed to a later date since primary stability may not be achieved.
The considerations for bone graft materials mentioned under the transcrestal technique also hold true for the lateral window technique. Bone augmentation is performed using autogenous bone material, bone substitutes or a mix of both. Studies have not found any difference in the implant survival rates due to differences in the graft material used or the time of implant placement (Starch-Jensen et al. 2018; Ting et al. 2017). Starch-Jensen et al. (2018) assessed the long-term implant treatment outcome after maxillary sinus floor augmentation with autogenous bone graft, mix of autogenous bone graft and bone substitutes, or bone substitutes alone.They concluded that the maxillary sinus floor augmentation procedure was a highly predictable and successful surgical procedure which enhanced the vertical alveolar bone height of the posterior part of the maxilla, before or in conjunction with implant placement, with a high implant survival rate observed.
Risk factors
Apart from the general risk factors discussed in the first segment, local factors like the presence of the sinus septa and a residual bone height of less than 3.5 mm increase the risk of a sinus membrane perforation if the lateral window technique is employed (Schwarz et al.2004).
Intra operative complications
Most intra-operative complications are common to both the transcrestal and lateral window techniques. Perforation of the sinus membrane are the most common intra-operative complication, although they do not seem to influence the final treatment outcome (Lee et al. 2013; Geminiani et al. 2017).The risk of sinus membrane perforation was seen to be higher when the lateral cortical bony window was dissected free and removed from the underlying Schneiderian membrane (Starch-Jensen et al. 2017).
Damage to the alveolar antral artery during the sinus floor elevation can result in bleeding complications. To prevent such complications, the site should be evaluated using a CBCT pre-operatively. The use of piezosurgical instruments instead of conventional rotary instruments is found to reduce the risk of bleeding complications. Limiting the superior border of the window is also an option since the distance between the alveolar ridge and the alveolar antral artery is, on average, about 18 mm (Tavelli et al. 2017).
Post-operative complications of sinus lift
- The incidence of post-operative infection has been reported to be 2 to 5.3%. This incidence is mainly attributed to membrane perforations, active infection at or around the operative site, lack of aseptic measures during the surgical procedure, use of an excessive amount of graft material after sinus membrane elevation, and poor compliance by the patient after the surgery. The symptoms along with an infection might appear as early as 48 hours after the surgical procedure. Clinical findings include wound dehiscence and exposure of graft along with pus discharge at later stages. Patients normally complain of pain, discomfort, a bad taste and odor.
In most cases, the infection may extend to the maxillary sinus and cause acute or chronic sinusitis. Sinusitis may remain confined to the maxillary sinus or involve other sinuses with serious consequences. Clinical signs and symptoms will vary according to the nature and severity of the condition (Schwarz et al. 2015, Ghasemiet al. 2017).
- There is a high risk of wound dehiscence in smokers with a partial or total loss of grafts. Other risk factors contributing to wound dehiscence include placement of a non-resorbable membrane over the augmentation material, flap closure with tension, and use of an incorrect incision design that compromises the vascular supply to the flap (Schwarz et al. 2015).
- Implant loss has been seen in cases where sinus floor elevation is performed. The loss is mostly seen within the first year after surgery. The primary reasons for implant loss include infection of the graft material, lack of adequate primary stability or early loading of implants before sufficient healing (Starch-Jensen et al. 2018)
- Persistent and excessive bleeding from the flap into the oral cavity occurs in rare circumstances. This is likely to occur in patients on anti-platelet or anti-coagulant medication. It is always recommended that bleeding should be controlled during surgery and a cold pack should be applied over the site during the 24 hours after surgery.
- A rare complication seen in relation to sinus floor elevation using the transcrestal technique is benign paroxysmal vertigo, or repeated brief-duration vertigo induced by head movement. Although the incidence rate at 3% is extremely low, it is hypothesized to occur as a result of percussive and vibratory forces produced by tapping the osteotome with a mallet. The symptoms usually resolve within 6 months. In patients with preexisting vertigo, the use of osteotomes should be avoided and alternatives like the lateral window technique utilizing piezosurgical instruments is encouraged. In other patients, excessive and forceful tapping of the osteotome with the mallet should be avoided (Su et al. 2008; Pjetursson et al. 2014).
- Another complication, though rare, is the displacement of the implant into the sinus cavity. In such situations, the implants must be removed using a lateral window approach. If this approach is not successful, endoscopy under general anesthetic is required to remove the displaced implant. If the implants migrate to deeper cranial regions, assistance from medical specialists is warranted (Kim 2017).
Conclusion
Sinus floor elevation is a predictable surgical procedure. However, patient evaluation and selection are critical to a successful outcome. There are various techniques for performing a sinus lift. Once the potential risk factors have been identified, a suitable technique is identified and communicated to the patient for consent and compliance.
Stay tuned for the third part of this blog article!
Related content: