Introduction
Even though new technologies and techniques have dramatically improved the treatment of edentulous patients over the years, clinicians still need to be aware of the challenges when managing these patients during treatment planning. The main reason is that, when implant-related treatments are involved, certain site-specific anatomic characteristics should be considered in treatment planning for either mandible and/or maxilla full-arch implant-supported prostheses. One of the challenges faced by the clinician could be related to data collection allied with the perception of a 3D setup of teeth and gingiva reconstruction according to the patient’s facial parameters. This step is well-known to be associated with specific maxillary anatomic and patient physiological characteristics like the quality of bone, bone resorption pattern, speech, and labial & facial support (Taylor et al., 1991; Schnitman, 1999; Zitzmann & Marinello, 1999). Fortunately, even in this scenario, several publications have reported high survival and success rates and low rates of esthetic complications for full-arch mandibular prostheses supported by dental implants (Malo et al., 2011; Polido et al., 2018).
Clinicians should know the anatomical limitations related to treatment planning for edentulous patients. It is important to gather as much information as possible in the most organized way. The ITI provides the best up-to-date scientific evidence related to implant dentistry, and this cannot be more true for edentulous scenarios. The Edentulous Esthetic Risk Assessment (EERA) is an independent checklist found in the ITI SAC Classification. It is capable of identifying and showing the most critical key factors related to full-arch maxillary restorations to which facial support, labial support, upper lip length, buccal corridor, smile line, and maxillomandibular relationship are integral. Among the characteristics mentioned above, one of the most important aspects of implant planning for maxilla and mandible full-arch implant-supported prostheses is the prosthetic volume and the minimal interocclusal space required for a prosthesis with adequate thickness for its materials that still allows good clearance for efficient self-cleaning of the prosthesis by the patient. Therefore, knowledge of interocclusal space values per arch and the materials/components necessary for the rehabilitation need to be assessed. Thus, the objective of this article is to discuss some important topics regarding the planning of the interocclusal space for a full-arch implant-supported prosthesis in the maxilla and the mandible.
Prosthetic volume and interocclusal space
According to the SAC Classification 2.0 in implant dentistry, the prosthetic volume refers to the general 3D space required for the prosthesis, taking into account the material that will be used as the infrastructure for artificial teeth and the height of the abutments. It is determined by the interocclusal space between the arches, mesiodistal dimensions, and orofacial dimensions required for adequate restorative space in the given scenario.
The definition of interocclusal space, according to the literature, may vary according to the measurement reference point, which can be:
- Implant platform to the opposing occlusal table
- Abutment level platform to the opposing occlusal table
- Planned restorative margin to opposing occlusal table
- Residual alveolar ridge to opposing occlusal table
The guideline within the SAC 2.0 should be used to prevent complications. It is essential to verify these four reference points before using published metrics, such as a difference of ~ 3 mm (when utilizing bone-level implants) can exist between reference points 1 and 4. To the best of our knowledge, the best way to manage the interocclusal space is to combine as much data as possible from that described above. It is essential to take into consideration all the characteristics of each patient individually and apply the prosthetically driven implant placement concept.
Throughout the treatment planning phase, clinicians face multiple questions. One of them is: is there enough space to restore? The answer is: it depends on the type of treatment. It depends on critical data that will be discussed in the following sections of this article. Taking into account the knowledge about the prosthetic volume and the interocclusal space, the type of prosthetic material that can be used to fabricate the prosthesis and the prosthesis design, the minimum interocclusal space necessary for full-arch implant-supported prosthesis, when using the alveolar ridge to the opposing occlusal table reference, is (SAC Classification 2nd E.E.R.A by L. Gonzaga, W. Martin & D. Morton):
- Fixed Dental Prosthesis (FDP): 7 mm
- Overdentures with individual attachments: 8 to 11 mm (e.g., Locator, Novaloc [Straumann])
- Overdenture bar with attachments: 14 mm
- Hybrid prosthesis: 12 to 15 mm (denture tooth, acrylic resin, and framework)
- Monolithic zirconia hybrid prosthesis: 11 to 14 mm
Esthetic and functional assessment of an edentulous patient for full-arch implant-supported prosthesis
Fabrication of a new setup of teeth or a new complete denture along with a photographic protocol provides valuable information regarding the interocclusal space available for full-arch implant treatment. For edentulous maxillary patients, a simple record of the patient fully smiling without the denture shows how much residual alveolar ridge will display during a smile. Thus, for patients who show the maxillary residual alveolar ridge during a full smile, the indication of a different prosthesis design may be requested (Taylor et al., 1991). Also, lip and facial support must be assessed for edentulous implant solutions in the maxilla to deliver the best prosthesis design according to the patient’s anatomic characteristics (Avrampou et al., 2013). However, anatomic site characteristics of the patient can be modified through adjunctive therapies to achieve lip support and sufficient space for the planned fixed solution (e.g. hybrid metal-acrylic full-arch implant-supported fixed dental prosthesis). These additional steps may provide a better prosthesis profile and, if possible, hide the interface between the restorative margin and the prosthesis contour under the smile. Additionally, determining a complete denture’s esthetic and functional aspects is key to helping identify the interocclusal space and prosthetic volume scenario. These factors are the position of the central incisor edge with the lip at rest, occlusal plane, smile line, and vertical dimension of occlusion (Sheppard & Sheppard, 2006). This information allows the 3D perception of the position of the teeth and its relation to the vertical space available for maxilla and mandible edentulous implant cases. The optimal vertical dimension of occlusion (VDO) is also essential for determining the interocclusal space and the prosthetic volume. However, the individual characteristics of the patient can also dictate the vertical dimension of occlusion. The optimal VDO must be assessed with the prosthetic volume, as not only is the position of the white esthetic of the teeth important, but the position of the pink esthetic also plays an integral role in determining the VDO that will result in different interocclusal space available to restore (Fig. 1).


How to measure the interocclusal space
According to the SAC 2.0 Classification, complex cases, like implant treatment of the edentulous maxilla and mandible usually involve more steps with a multidisciplinary approach. Prosthetically driven implant placement is a fundamental concept, and clinicians should follow this concept. The intraoral space can be measured after a new teeth setup or using a duplicate of the patient’s existing complete denture, this is carried out “flangeless” if facial support is not required. Interocclusal space measurements can be made with working casts mounted on a semi-adjustable articulator, measured intraorally or digitally. The use of one or more methods can help increase implant case predictability.
Conventional workflow
In a conventional workflow, the measurements are made in a semi-adjustable articulator and with an intraoral teeth setup. As mentioned, an esthetically and functionally correct setup of the teeth must be fabricated (Fig. 2) to verify the interocclusal distance between the residual alveolar ridge and the opposite occlusal table. The setup must follow the basic concepts of a complete denture, where lip support, buccal corridor, the position of the central incisor edge, smile line, midline, and finally, the record of the vertical dimension of occlusion with centric relation. Unlike a conventional try-in appointment for a complete denture, in a fixed reconstruction the clinician often uses a “flangeless” teeth setup. In this workflow if a flange is required for facial support, a putty silicone jig on the buccal aspect of the teeth on the stone cast is made together with the working cast before removing the flange (Fig. 3).



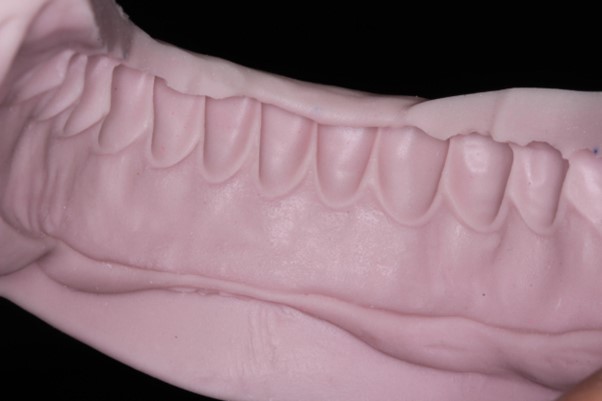
This procedure records the flange of the teeth setup performed on the previous appointment, allowing the reconstruction of this area before processing the prosthesis. Additionally, the putty silicon in the working cast is repositioned to measure the residual alveolar ridge and the three-dimensional positioning of the teeth (Mericske-Stern et al., 2000). This procedure can also be performed intraorally by positioning the “flangeless” teeth setup. This simple procedure shows the relationship between the residual alveolar ridge, the cervical of the teeth, and the vertical space between them (Fig. 4), assessing the lip and facial support, simplifying the decision on which prosthesis design is best indicated for the patient. This exact procedure can be performed digitally, as demonstrated by Avrampou et al., 2013. It is essential to point out that the flange in the most posterior region (upper molar region) and the palate need to be maintained for better stabilization of the setup in the mouth.


Tip 1: use a “flangeless” teeth setup or duplicate a complete denture using transparent acrylic resin
Combining conventional and digital workflow
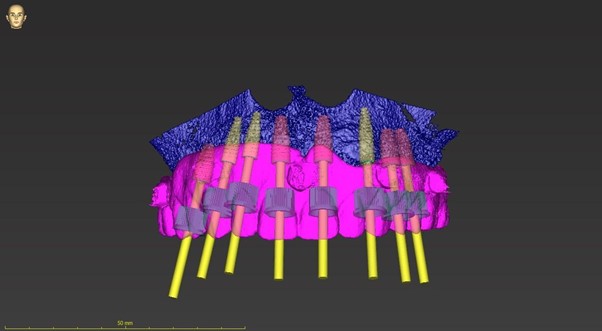
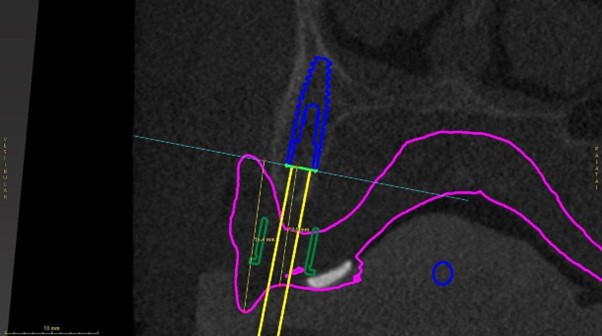
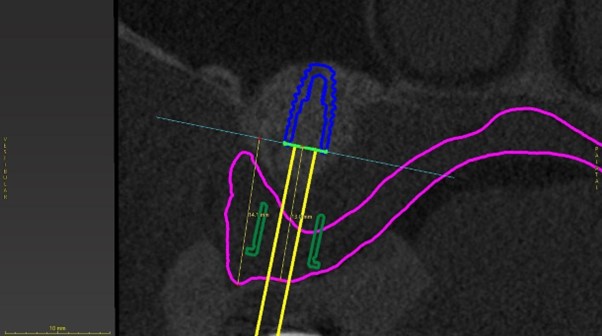
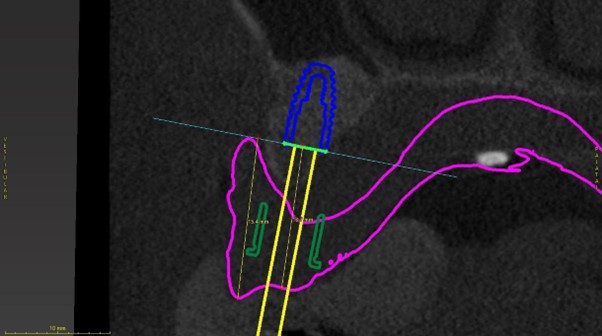
On the other hand, CAD/CAM software can also help the clinician to measure from point A to point B in multiple planes. Many different techniques can achieve this, one of the more simple and straightforward methods would be the digital dual scan (DDS) technique (Vercruyssen et al., 2014) for planning edentulous scenarios. In this method, two CBCT digital images are required, one with the patients wearing the teeth setup with radiopaque markers stabilized by an occlusal bite record. The subsequent CBCT would be the teeth setup with the radiopaque markers. If the teeth setup is an existing complete denture, the denture must be relined prior to the CBCT scan in line with all esthetic and functional requirements. After the acquisition of DICOM files through the CBCT scan, both files are imported into the software and merged. By merging the DICOM files, it is possible to plan the implant positioning, which is performed in an adequate three-dimensional distribution to obtain adequate interocclusal space and prosthetic volume for the emergence profile of the future full-arch-supported implant prosthesis (Fig. 5). Finally, after merging the DICOM files, prosthetically driven virtual implant positioning can then be planned. The measurements can then be performed either from the residual alveolar ridge, implant shoulder, or abutment platform to the virtual teeth setup to check if sufficient prosthetic space is present.
Tip 2: When using an old denture (with good esthetics and functional aspects in place) to perform a DDS technique, the intaglio surface of the prosthesis needs to be relined before the two scans, due to the residual alveolar ridge resorption over time.
Final considerations
When assessing the interocclusal space required for a reconstruction, the Edentulous Esthetic Risk Assessment (EERA) must be considered (E.E.R.A, ITI SAC 2.0, pg.21-26). It is critical to understand which defect is present in your patient’s ridge and lip horizontally, and the prosthetic tooth and ridge vertically to classify whether your case falls into the category of esthetic risk only or combined with structural risk. The EERA checklist is used to determine the risk difficulty (E.E.R.A, ITI SAC 2.0, pg.22). Subsequently, the knowledge related to the issue of interocclusal space and prosthetic materials allows the clinician to provide the best oral health service and prosthesis design to the patient, preventing random clinical approaches and decreasing the chance of esthetic and functional problems by providing precise information about the clinical situation. Maxillary full-arch implant-supported prostheses are more complex than mandibular ones regarding the esthetic planning of the smile, lip, and facial support. Regardless of the method used to measure the interocclusal space, clinicians must make sure that there is enough space available for a particular type of prosthesis design and prosthetic material and that it follows the patient’s individual characteristics.