Introduction
Ridge preservation is defined as any procedure undertaken at the time of or following an extraction that is designed to minimize external resorption of the ridge and optimize bone formation within the socket as a consequence of bone remodeling.
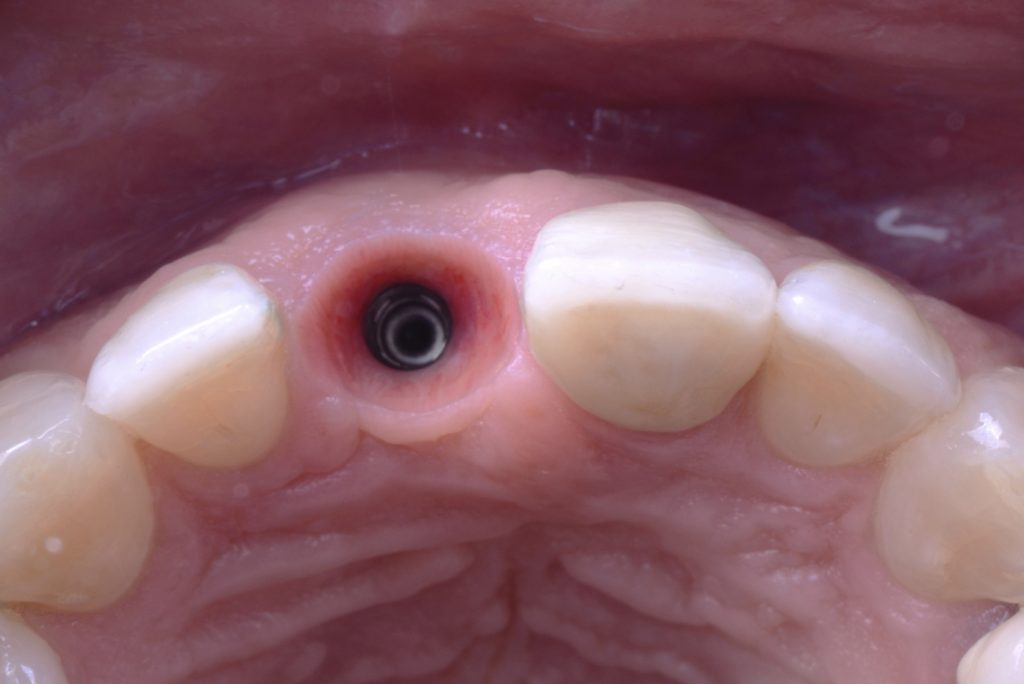
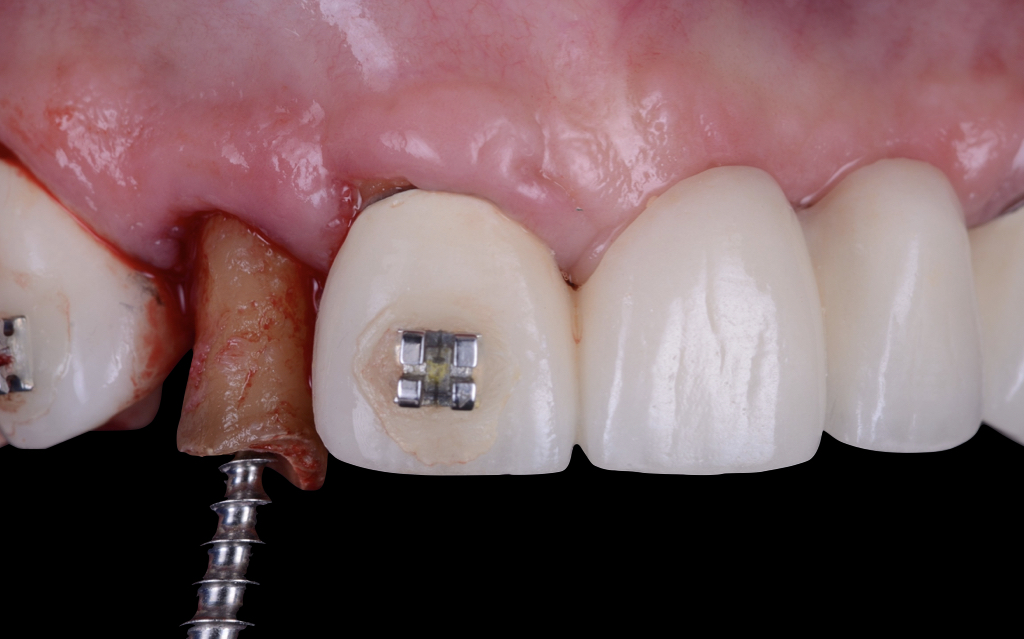
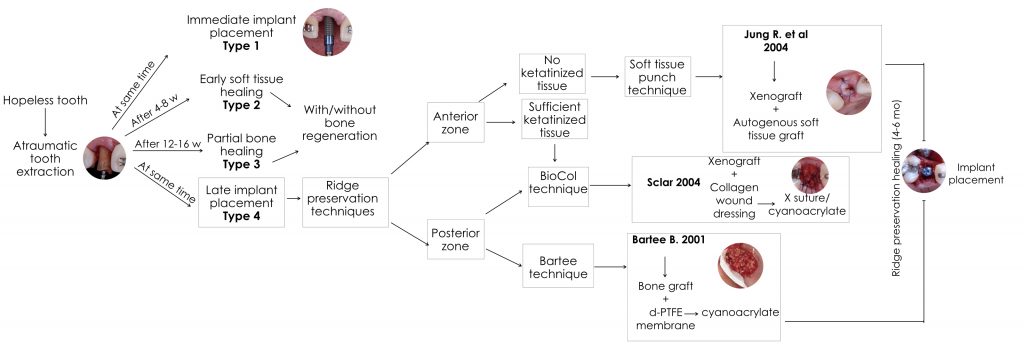
As far as possible, immediate implant placement with immediate restoration or a customized healing abutment (SSA) represent our treatment of choice to preserve both the ridge dimensions after tooth extraction and the natural architecture of the peri-implant mucosa (Figs 1-5).
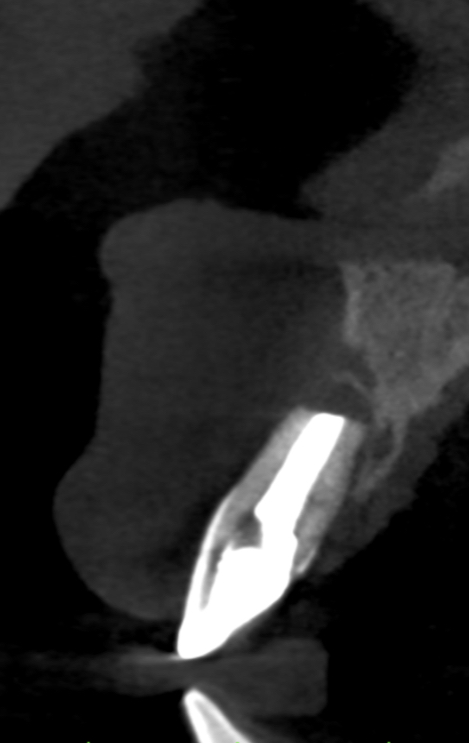
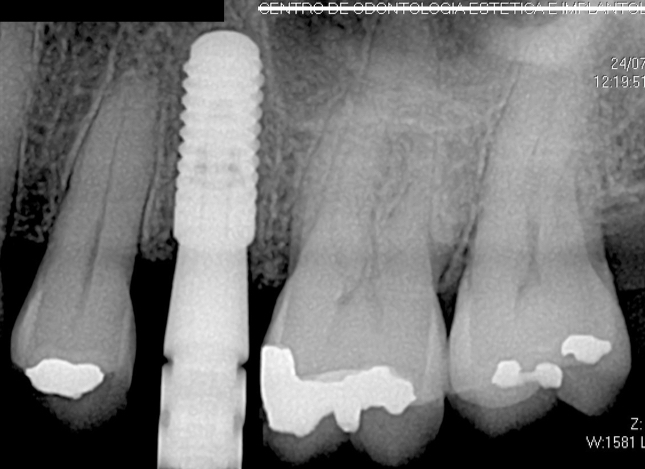
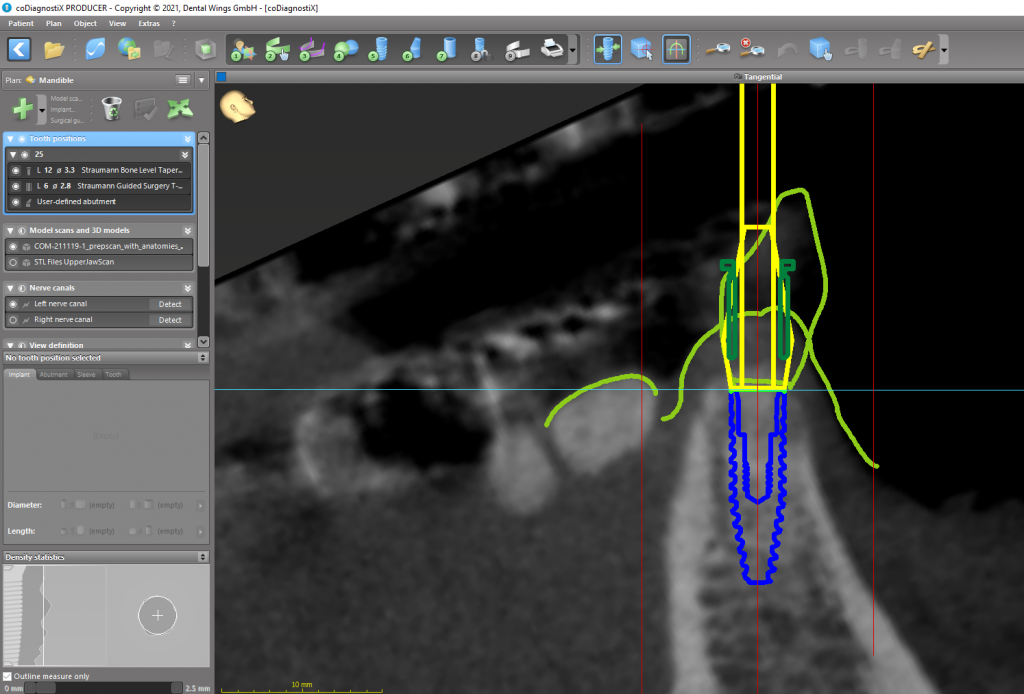
Nevertheless, there are clinical situations where immediate implant placement is not recommended due to site-specific reasons like purulent infection, lack of apical bone availability (Fig. 6) and large peri-apical bone lesions that can compromise prosthetically driven implant placement (Figs 7 and 8). Additionally, some patient-specific reasons such as too young adolescent patients, pregnancy and uncontrolled systemic conditions are considered important factors in daily decision-making. (Buser et al, 2017). In such scenarios, a late implant placement protocol represents a highly predictable alternative that is scientifically and clinically documented.
For this reason, when late implant placement is indicated, we recommend performing a ridge preservation procedure to minimize the dimensional changes and assure prosthetically driven tridimensional implant placement (Fig. 9).
In this clinical article, we describe some of the most frequently used ridge preservation techniques in conjunction with clinical recommendations based on our expertise for a decision tree for different clinical scenarios.
The soft tissue punch (Jung, 2004)
This is one of the most popular techniques for ridge preservation and is mainly used in the anterior region when we want to preserve both hard and soft tissue. This technique from Dr. Landsberg and Dr. Bichacho dates back to 1994 when they described a method in which the socket was grafted with bone substitute after tooth extraction and covered with a thick free gingival graft (socket seal surgery). In 2004, Dr. Jung and Dr. Hämmerle published a new postextraction tissue management named soft tissue punch technique that showed high predictability and good esthetic results (Jung R et al, 2004).
Surgical technique
- Removal of the tooth with atraumatic extraction device to avoid damage to the socket walls. Remember, do not elevate a flap. (Garg 2001) (Fig. 10).
- Afterwards remove any granulation tissue.
- De-epithelization of the gingival socket walls to help vascularization of connective tissue graft.
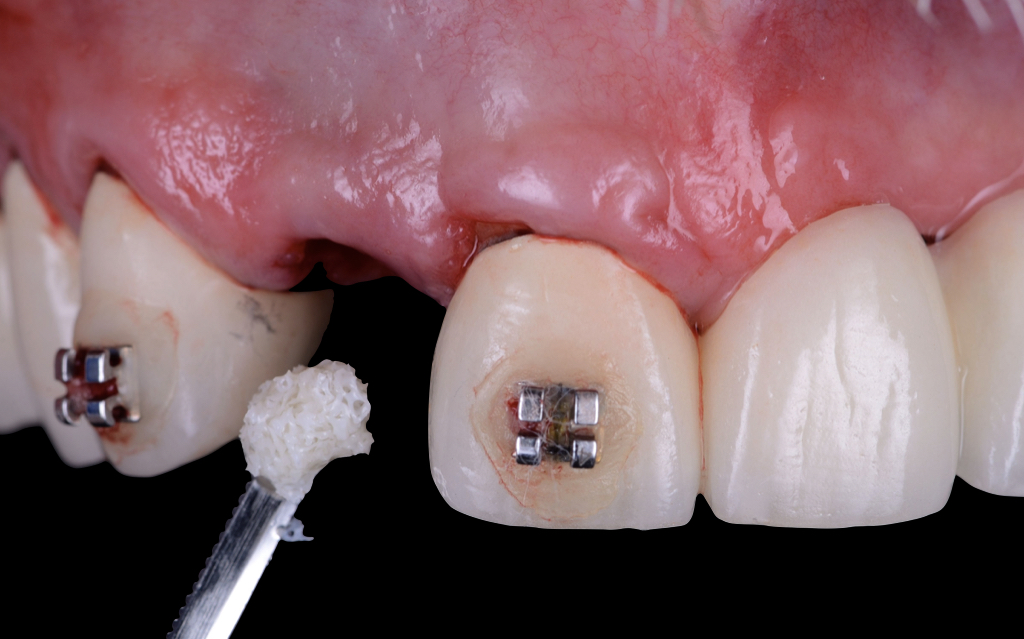
- The bone graft material (in the original technique the authors used a deproteinized bovine bone mineral with a collagen matrix) is placed into the socket without excessive compaction (a particulate graft can also be used) (Figs 11 and 12).
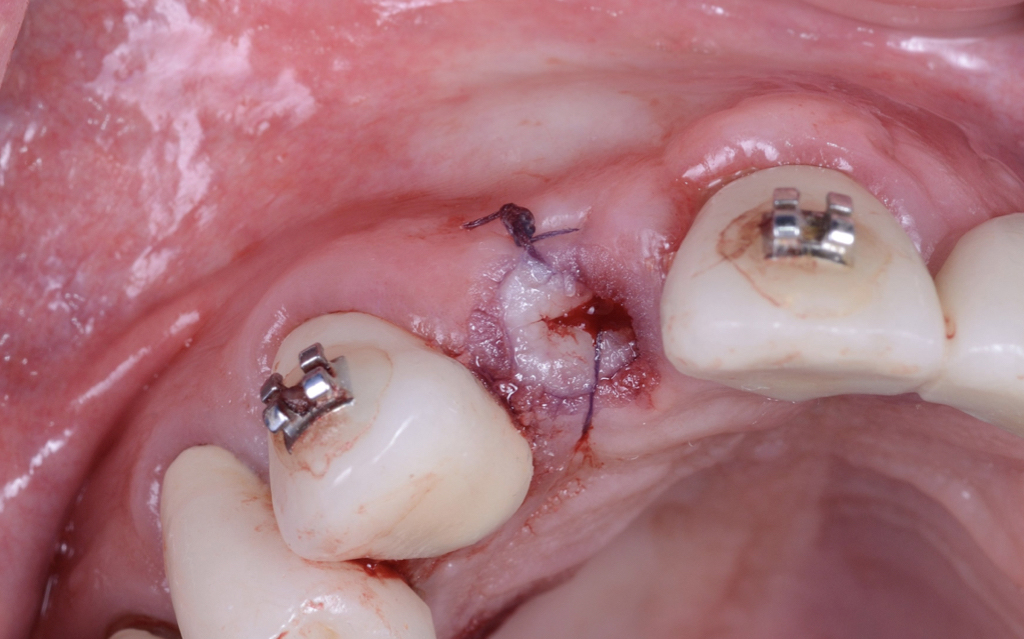
- Preparation of the donor site (palatal mucosa) with a soft tissue punch (the size corresponds to the socket orifice).
- Suture and assure the maximum stability of the gingival graft (place as many sutures as needed; it is preferable to use microsurgery sutures in combination with cyanoacrylate surgical glue) (Figs 13 and 14).
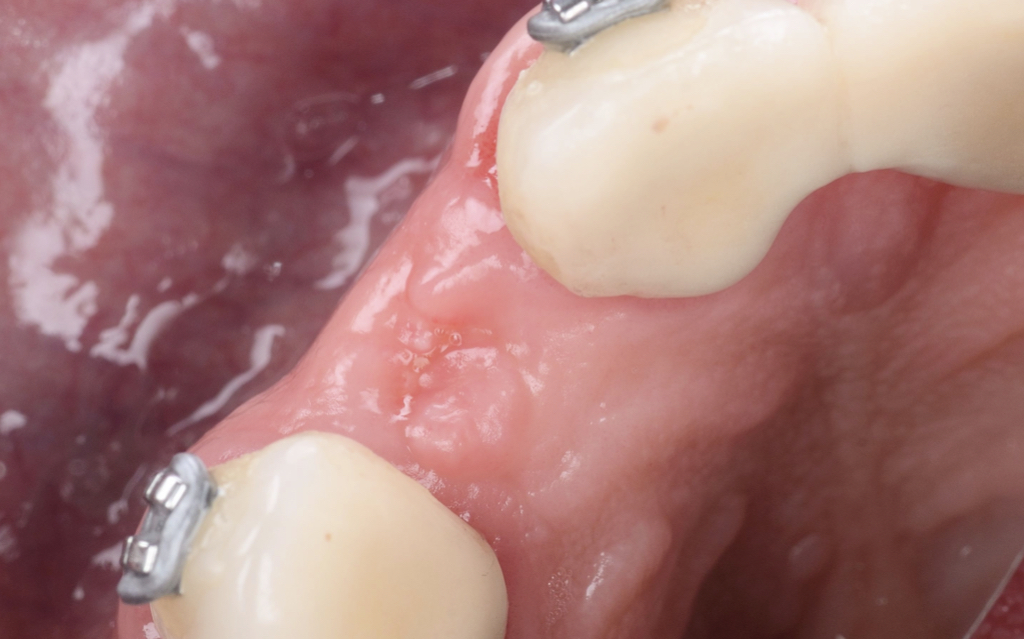
We recommend removing the recipient sutures after 10-15 days (Figs 15 and 16). The success of this technique depends on the free gingival graft vascular supply. We recommend using this technique in cases where we also need to gain keratinized tissue for the subsequent procedures. According to our clinical experience, we advise using this method is in the anterior zone due to the size of the free gingival graft to seal the socket.
The soft tissue punch technique requires more surgical experience to take the graft and also to accommodate and assure the blood supply without compromising the procedure.
The Bio-col technique (Sclar, 1999)
This technique could be used for either anterior or posterior teeth and, in the original publication, the author suggests it can also be used with immediate implant placement.
Surgical technique
- Atraumatic tooth extraction and removal of any granulation tissue (Figs 17 and 18).
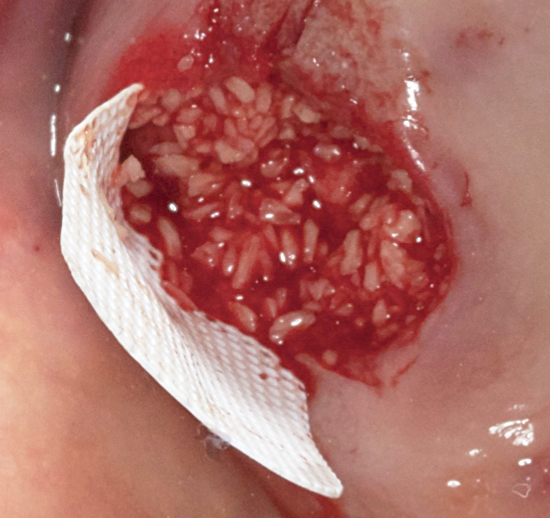
- Preparation of the bone graft previously moistened with sterile water (the original publication suggests using a xenograft) (Fig. 19).
- Placement of collagen wound dressing to seal and protect the bone graft.
- Suture with a traditional X technique to assure the collagen wound dressing. (Fig. 20). The collagen dressing helps to control bleeding and will be fully resorbed within 14 days; suture removal should be done at 10 days.
This is a straightforward technique since it avoids a free gingival graft. Our clinical recommendation is to use it on posterior teeth with a wide band of keratinized tissue.
The Bartee technique (Bartee, 2001)
It is well known that membranes help to prevent soft tissue and epithelial migration into the healing socket, however they must remain completely covered by the flap to avoid contamination and posterior infection. Nevertheless, there is a non-resorbable membrane that due to its low porosity (<0.2um) resists the incorporation of bacteria and can be left exposed without compromising the underlying bone graft. This membrane is a dense polytetrafluoroethylene (PTFE) named TXT-200.
Surgical technique
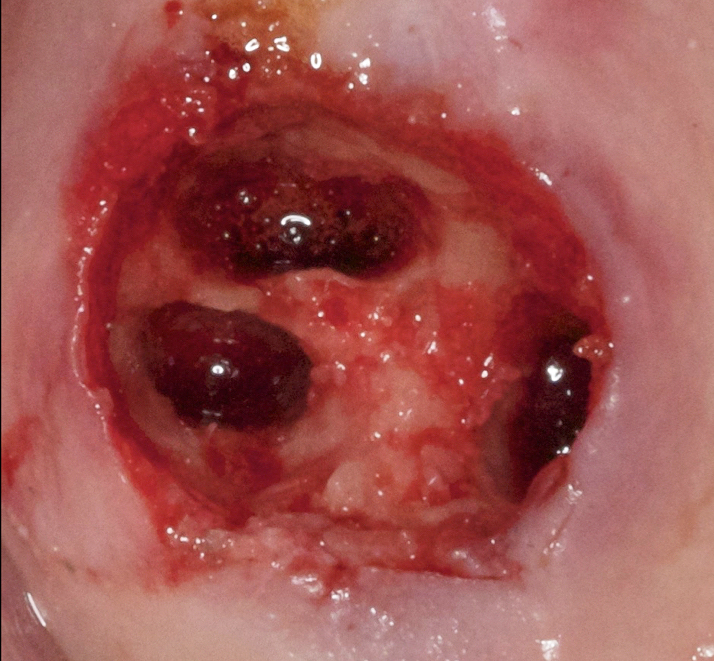
- Atraumatic tooth extraction (remember to do a hemisection if is a multirooted tooth) (Figs 21 and 22).
- Sharp curettage to remove remnants of periodontal ligament as well any granulomatous tissue.
- Perforation of the socket is optional (you can use a slow speed round bur) to improve blood supply.
- Preparation of the graft material and placement into the socket while avoiding overpacking.
- Carefully detach it with a periosteal elevator in preparation for the buccal and lingual tunnel .
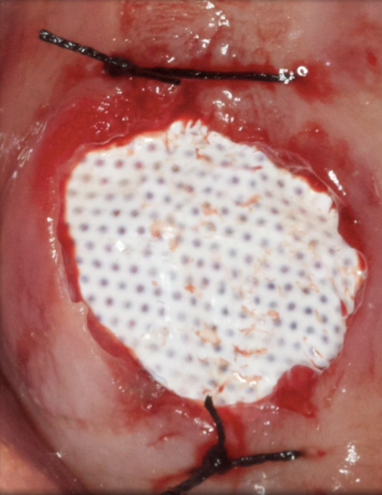
- Placement of the membrane (previously trimmed) extending 3-4 mm beyond the socket margins, it should fit over the site and under the tunnel preparation without wrinkling (Fig. 23)
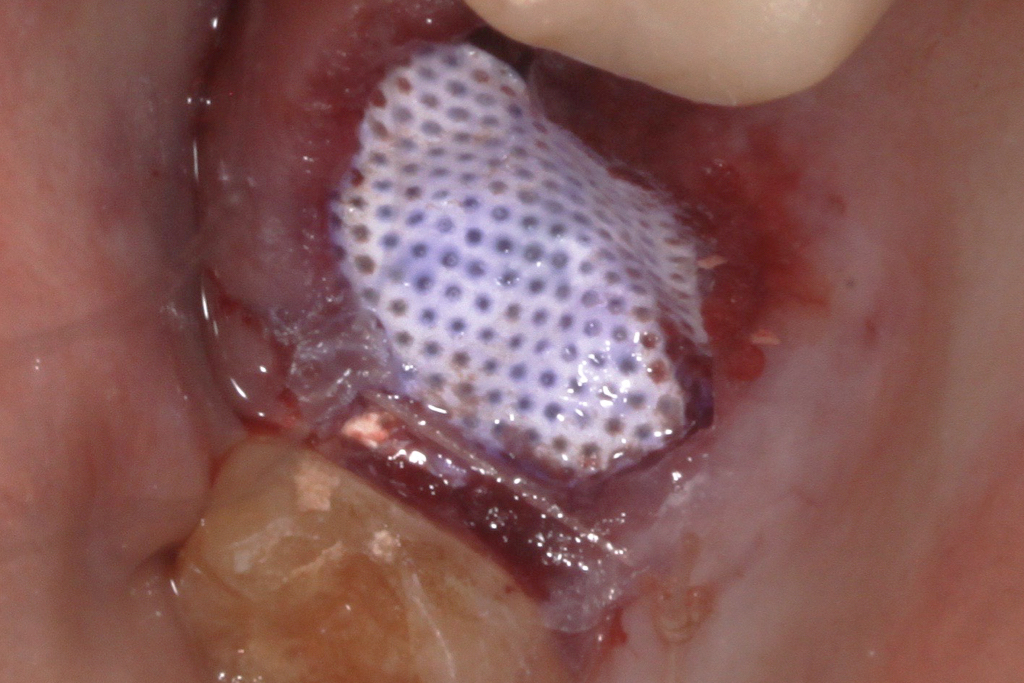
- Suturing is optional (according to the technique). Our clinical recommendation is placement of an X suture to help stabilize the membrane or use of cyanoacrylate above the membrane to act as a protective layer. (Figs 24a and 24b).
- The membrane should be removed without anesthesia after 21 to 28 days (Fig. 25). We recommend placing the membrane into the socket margins after tooth extraction to make placement of the bone graft easier. The advantage of this technique is to preserve the soft tissue architecture and keratinized mucosa. Although this method is indicated for either the anterior or posterior zone, our clinical recommendation is to perform this technique in the posterior section due to the exposition of the membrane that can compromise the esthetics.
In our experience as clinicians, we have had good results with all the ridge preservation techniques. There is no significant difference between techniques regarding bone formation and bone remodeling. Nevertheless, in scenarios where the treatment of choice is late implant placement, it is preferable to perform one of the above techniques, and the choice will depend on the clinical scenario, area or tooth of interest, and soft tissue availability. We also need to consider that this procedure is without flap and papilla elevation, so it is important to have the integrity of bone walls, otherwise the surgical treatment recommendation is guided bone regeneration.
Our goal was to review the guidelines for alveolar ridge preservation and create a diagrammatic representation of evidence-based techniques that will help clinicians in decision making in cases where late implant placement is an option (Fig. 26).