Tissue-level implants have a long history and are still relevant for today’s practice in implant dentistry. Although bone-level implants dominate the implant market nowadays, the significant advantages of tissue-level implants are still valid, especially when restoring the posterior non-esthetic region. While advocating caution in the use of tissue level implants, this article lists four reasons why dentists and oral surgeons should choose tissue-level implants when placing dental implants in non-esthetic posterior sites. The article also outlines four situations in which bone-level implants are recommended in posterior sites.
In this article, “tissue-level implant” refers to the Straumann Standard implant or Standard Plus implant and “bone-level implant” refers to the Straumann bone-level implant or bone-level tapered implant.
Four reasons to choose tissue-level implants for posterior sites
1) The built-in emergence profile for the transmucosal part can achieve an optimal emergence profile for posterior restoration
In most cases after tooth removal the width of the alveolar ridge becomes narrower than before. Therefore, the implant diameter must be narrower than the root of the extracted tooth. However, the dimension of the restored tooth crown should not be smaller than that of the original tooth. Consequently, the emergence profile of the implant tends to be a wide-spreading configuration compared to that of the original tooth.
To compensate for this profile, the platform of the implant neck should be wider than that of the implant platform. The tissue-level implant serves this requirement with a wide emergence profile and favorable esthetics, as shown in Figure 1.
In contrast, bone-level implants have a platform-switching design in the implant platform; therefore, the platform of the implant is narrower than the implant body, which is the opposite of the ideal configuration to optimize the emergence profile, as mentioned.
Consequently, the emergence profile of restorations on bone-level implants tends to be frequently ridiculed as a “pumpkin on a stick,” as shown in Figure 2.
2) Minimal intervention around peri-implant tissue
Tissue-level implants have the abutment on top of the implant in one component and follow non-submerged healing. This treatment protocol enables osseointegration of the rough surface of the implant body and soft tissue attachment to the polished implant abutment during the same healing period after implant placement. In addition, subsequent prosthetic steps deal only with the part above the soft tissue attachment; therefore, soft tissue attachment is not disturbed by repeated abutment removal and reconnection, which is inevitable when we use bone-level implants.
3) Lower susceptibility to peri-implant disease
It has been retrospectively proven that bone-level implants are more susceptible to peri-implant disease than tissue-level implants. Derks et al. analyzed the prevalence of peri-implant disease among approximately 600 Swedish patients and compared the implant manufacturer and prevalence of peri-implant disease. As a result, tissue-level implant design, among others, have a significantly lower prevalence of peri-implant disease.
This is probably because the platform of tissue-level implant is 2.8 mm or 1.8 mm from the alveolar bone if the smooth/rough interface is placed at the crest. Although the platform of the bone-level implant is horizontally distant from the bone/implant interface, it is closer to the alveolar bone compared with tissue-level implants.
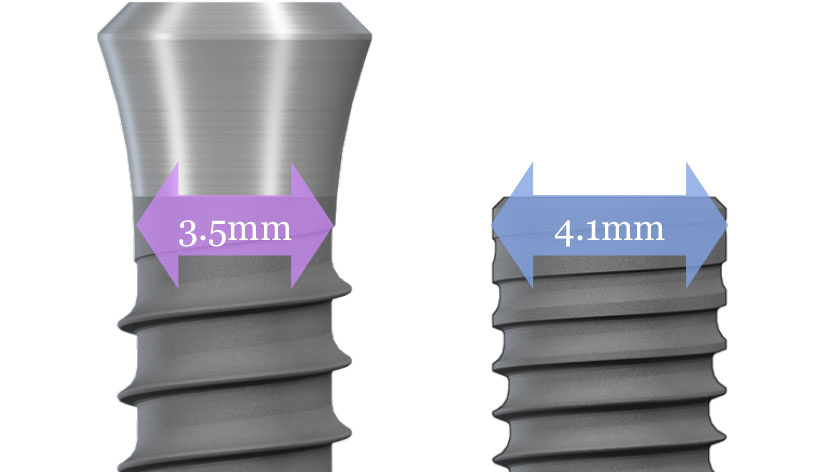
4) Intrabony diameter of tissue-level implants is narrower than bone-level implants
Due to the densely threaded design of bone-level implants, the virtual diameter of the cervical part of the implant is 4.1 mm for regular size. However, tissue-level implants have a lower thread distribution, especially around the cervical part, with a diameter of 3.5 mm as the regular size. Therefore, exposure of implant rough surfaces is less likely for tissue-level implants, which can minimize the need for a bone-grafting procedure.
Four situations in which bone-level implants are recommended in posterior sites
1) Situation requires simultaneous bone-grafting when placing the implant
Simultaneously guided bone regeneration is frequently performed to eliminate bone defects around implants. In this situation, tissue-level implants make it difficult to close the flap to submerge the implant; therefore, the selection of bone-level implants makes the procedure easier.
In addition, when we perform sinus augmentation procedures at the same time as implant placement, a bone-level implant might be favorable.[2] In this situation, the stability of the implant around the cervical part is crucial to primary implant stability. If we use a tissue-level implant in this situation, because of the few threads around the implant neck and parallel implant body configuration, it is sometimes difficult to achieve sufficient initial implant stability. However, bone-level implants have a degree of taper around the neck and a densely distributed thread, which becomes wider close to the implant neck, allowing the surgeon to achieve initial stability more easily.
2) Limited mesio-distal dimension

Typically, in the upper premolar sites, as shown in Figure 4, the mesio-distal dimension is not sufficient to accommodate the relatively large platform of the implant neck of the tissue-level implant. The neck diameter of the standard implant is 4.8 mm, whereas that of the bone-level implant is 4.1 mm
3) Limited vertical space toward opposing dentition
Since the height of tissue-level implants is 2.8 mm or 1.8 mm for the polished neck part, restoration of the edentulous ridge with limited vertical space is challenging unless it is compensated by sinking the implant neck deeper or reducing the height of the opposing teeth. As shown in Figure 5, limited vertical space for implant-supported crowns leads to a compromised crown profile, fracture of veneering materials, and screw exposure on the occlusal surface of the crown.

4) Esthetically demanding patients for whom metal color exposure at the implant neck is unacceptable
As peri-implant mucosa recession and subsequent implant neck exposure can occur over the years (Figure 6), practitioners should be cautious when selecting tissue-level implants for patients with high esthetic expectations. Although most patients are unconcerned, others complain about it, and this cannot be prosthetically recovered.

Related ITI Academy module








