Implant dentistry today is moving towards digital planning, guided insertion of the implants and potentially a flapless approach. However, before one, as a surgeon, can become active in this digital age, one must have knowledge of anatomy and basic surgical principles, as well as a good understanding of one’s own skills and limitations.
This article will describe the basic principles of flap design in dental implantology.
The purpose of raising a flap is to ensure adequate visibility and access to the surgical area. In this way local anatomical structures can be identified. These structures could be the mental foramen, the incisive canal together with local buccal and lingual concavities. Also, it is beneficial to be able to inspect the alignment of the roots of adjacent teeth during the implant osteotomy.
A flap must be raised with care to ensure that the blood supply to the flap is preserved, and that the soft tissue of the implant site and of the adjacent teeth are not damaged. Careful flap handling means that the flap should not be excessively twisted, stretched or grasped since this may damage the blood vessels supplying the flap. A consequence of such damage to the blood supply may result in flap necrosis, delayed healing and potential scarring of the soft tissue.
A plan must be made for raising as well as repositioning the flap after implant placement. The edges of the flap must be approximated again over healthy bone without applying any tension. The edges of the flap should lie passively close to each other just before suturing. Suturing must be performed with connective tissue opposed to connective tissue to ensure primary closure. No significant force should be used to make the edges line up with each other. To ensure close flap adaptation to the underlying bone, the formation of hematoma should be minimized.
If the edges do not line up, the flap must be mobilized by preparing a horizontal periosteal releasing incision. This incision is made at the base of the flap apical to the mucogingival junction. Once the periosteum has been released, the flap can be mobilized and moved coronally and it will then be possible to suture the flap without tension.
Flap complications
Tearing of the flap can be a common complication when the prepared flap is not large enough for visual inspection of the surgical site. Poor visibility of the surgical site may lead to the application of unnecessary force with the tissue retractor and other instruments in order to be able to perform the surgery. One result of this may be the formation of a flap dehiscence during healing. The dehiscence may expose the underlying bone, implants and bone augmentation material, respectively. The dehiscence may result in pain, bone loss, loss of augmentation material, delayed healing, increased scarring and potential failure of the treatment.
Treatment plan
The choice of flap design for implant therapy depends on the treatment plan and should therefore be selected in advance. It is usually not possible to change the flap design during surgery if the conditions of the anatomical structures, the amount of bone and/or the amount of soft tissue are not as expected.
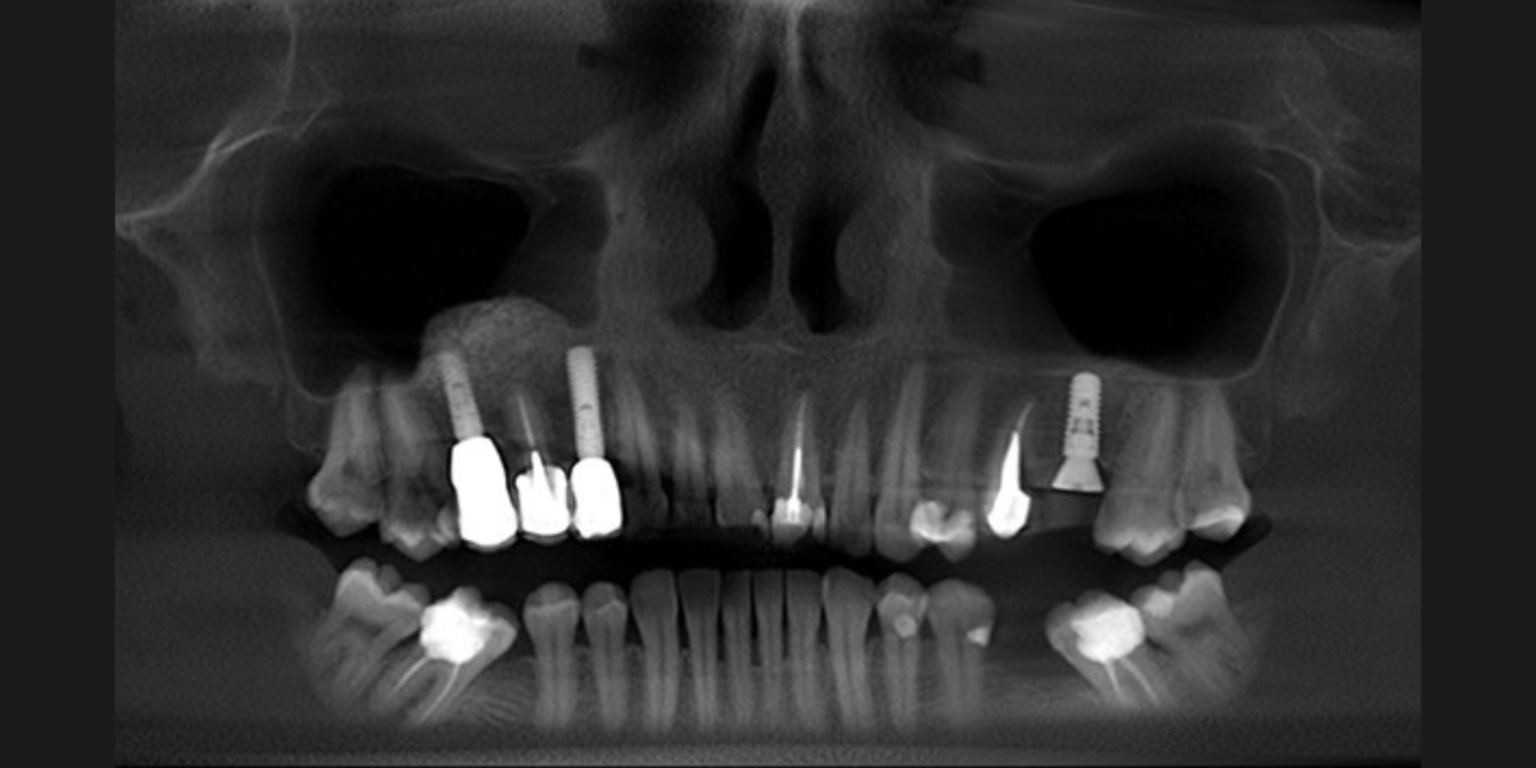
The flap design must take into consideration the number and location of implants required to replace the missing teeth, and whether the implants are to be inserted in a one-stage or a two-stage procedure. The amount of bone should be assessed clinically and radiographically to decide if the implant can be placed with or without simultaneous bone augmentation or if bone augmentation should be performed as a separate surgical procedure. A special esthetic risk assessment should be done before placing implants in the esthetic zone to determine if the flap design needs to be varied to minimize esthetic complications.
There are many variations in the design of surgical flaps for dental implant surgery, often with subtle differences according to the clinical conditions and preference of the clinician. Although it is not possible to cover every variation, there are certain situations where specific flap designs can be considered.
Horizontal incisions – crestal incisions – one-sided flaps
Horizontal incisions, also referred to as crestal incisions or one-sided flaps, are usually made in the median position of the ridge. The crestal incision extends intrasulcularly around the neighboring teeth. This type of incision may be chosen when inserting implants in posterior areas with sufficient bone volume. This incision can be altered to a paramedian position, either buccally or lingually to the mid-crest. When the remaining keratinized mucosa at the crest of the ridge is minimal, a horizontal incision placed at the median part of the ridge would result in the incision being made into non-keratinized mucosa. In order to maintain keratinized tissue at the edges of the buccal and lingual flaps, the horizontal incision often needs to be made in a lingual position. On flap closure, a region of keratinized tissue is then maintained on both the buccal and lingual sides of the implant.
For implant surgery in the anterior maxilla, where esthetic outcomes are important, paramedian incisions are made on the palatal side of the crest to increase the volume of soft tissue on the buccal aspect of the implant. Paramedian incisions are also used to facilitate closure of the flaps, when bone augmentation procedures are being considered. In this situation the paramedian incision is a part of a larger incision, as a two-sided or three-sided flap.

Two-sided flaps
A crestal incision, extending intrasulcularly around the neighboring teeth is usually not sufficient to gain access to a surgical area. Access can be improved by a vertical releasing incision to convert the flap to a two-sided design. As a fundamental rule, a vertical releasing incision must not compromise the blood supply of the flap and in general it is therefore placed anteriorly and at an angle that ensures a broad base to the flap. The two-sided flap design generally provides sufficient visualization of the surgical field in sites with sufficient bone volume, or when only minor bone augmentation is required in conjunction with implant placement. It is possible to treat minor residual peri-implant defects and still ensure a tension-free adaptation of the flap with this design.
Peri-implant fenestration or dehiscence defects occurring after implant placement require simultaneous bone augmentation. If these kinds of defects are expected, a two-sided flap and sometimes even a three-sided flap should be raised. The aim is to expose the whole surgical site to provide access for implant placement and bone augmentation, and to be able to mobilize the flap for primary closure using horizontal periosteal releasing incisions.

Three-sided flaps
The trapezoid or the three-sided flap can be recommended for larger bone augmentation procedures such as block grafts.
A crestal incision at the palatal aspect is performed together with two vertical releasing incisions. Reflection of the flap starts anteriorly to gain optimal flap control and overview. The trapezoid flap allows very good visualization of the surgical field. However, more bleeding can be expected because vessels running from the posterior to the anterior jaw region may be cut when the posterior vertical releasing incision is made.

Implants in the esthetic zone
Cases requiring implant placement in the esthetic zone are classified as Advanced or Complex according to the SAC Classification. SAC stands for Straightforward, Advanced and Complex. Advanced and Complex cases require great care in soft tissue handling. The smallest mistake or unsuitable incision will result in scarring of the soft tissue, which may compromise the esthetic outcome. Damage to the papilla, particularly if there is resorption of the underlying proximal bone on the adjacent teeth, will result in tissue recession leaving black triangles between the neighboring teeth and the implant crown. Extensive mobilization of the flap may induce a movement of the mucogingival border in a coronal direction. In patients with a very distinct border between the keratinized and non-keratinized mucosa, in particular, the esthetic outcome may be unsatisfactory. Specific incision techniques apply to preserve the soft tissue at the adjacent teeth and soft tissue in the esthetic zone.
Parapapillary incisions
To preserve the interdental papillae, a limited flap design may be used. In this type of flap design, parapapillary incisions are prepared. The interdental papillae are not included in the mucoperiosteal flap but are left attached to the bone at a width of 1 to 2 millimeters. This approach may preserve more of the interproximal crestal bone than a wider flap that includes the interdental papillae.

Small flaps – drawbacks
Raising very small flaps, especially in the esthetic zones, may be beneficial to bone and soft tissue healing. However, the visibility of the surgical area is reduced and will not reveal potential bone concavities or bone fenestrations occurring during implant placement. Also, the position and angulation of adjacent roots cannot be seen.
In addition, simultaneous bone augmentation will be almost impossible to perform, as proper adaptation of the flap may not be possible. Another disadvantage of the limited flap design is the risk of soft tissue scarring, especially if the margins of the flap are not adequately adapted.
Flapless surgery
Implants may also be placed without elevation of surgical flaps. This is referred to as flapless surgery and results in reduced morbidity and post-operative pain. However, it is a “blind” procedure and a high level of operator skill and experience are required. Careful planning is necessary with three-dimensional radiographic imaging combined with radiographic and surgical templates. The procedure can be performed in healed sites, where there should be sufficient bone volume to allow the implant to be placed in the correct three-dimensional position. A sufficient area of keratinized mucosa must be available to ensure that the implant emergence is entirely within the zone of keratinized tissue.
Immediate implant placement
In extraction sockets, implants may also be placed without the elevation of a flap. Prerequisites to performing this approach are intact socket walls and a facial bone wall of at least 1 millimeter in thickness, which can be verified at the time of extraction. The soft tissue must be thick and the site must be free of infection. The treatment can only be successful if there is sufficient bone apical and palatal to the socket to allow adequate primary implant stability. According to the SAC risk assessment, immediate implant placement is an advanced to complex procedure.
Conclusion
When it comes to surgery and implant placement, treatment planning is the key to success. This means that the surgeon must have a specific plan for the flap design. The flap design depends on the area where the implant is to be placed. Is the implant to be placed in a posterior area or in an esthetic zone? The number and position of the implants have an impact on the flap design as do a potential simultaneous bone augmentation or the expectation of a peri-implant defect occurring after placement of the implant.
Irrespective of the individually chosen flap design, the soft tissue must be handled with care. This means careful incision, careful reflection of the flap and careful re-adaptation and tension-free suturing. However, even if the treatment is performed carefully, complications such as flap dehiscence may occur with potentially compromised healing as a result.
Flaps may be one-sided when placing implants in posterior areas with sufficient bone volume, whereas two-sided flaps are chosen when simultaneous bone augmentation is planned or peri-implant defects are expected. Three-sided flaps are recommended for staged bone augmentation procedures. In esthetic zones, smaller incisions like the parapapillary incision can be used if no simultaneous bone augmentation is expected. Flapless surgery requires careful radiographic and clinical planning, sufficient bone volume and an experienced surgeon.
For further references, check out the following content pieces on the ITI Academy: