Introduction
Implant-supported fixed complete dental prostheses (IFCDPs), when correctly indicated, are an excellent concept for restoring the quality of life of edentulous patients (SAC Classification 2nd Edition and E.E.R.A by L. Gonzaga, W. Martin & D. Morton). A variety of different restorative materials have been described in the literature and implemented over decades to fabricate these types of prosthetic devices.
Materials such as metal-acrylic resin, metal-composite resin and metal-ceramic have been considered the most popular choices due to their long-term follow-up in the scientific evidence, clinicians’/technicians’ experience over the years, and, in the case of metal-acrylic, simplicity, reduced cost and easy repairability.
Nevertheless, these materials have shown high rates of technical complications and, therefore, demanding and frequent visits for maintenance and repairs (Fig. 1) (Balshi et al. 2016, Bidra et al. 2017, Papaspyridakos et al. 2017). This could represent a significant drawback and financial inconvenience for both the clinician and the patient.

Owing to advances in digital manufacturing technologies in recent decades, the introduction and application of different groups of novel CAD/CAM materials in implant rehabilitations have significantly increased. Additionally, a new trend toward metal-free high esthetic, biocompatible, and long-lasting restorations has been observed. High-strength ceramics such as monolithic zirconium dioxide have been widely implemented to rehabilitate such clinical scenarios. The success and long-term stability of full arch implant-supported zirconia restorations can be achieved when essential considerations are followed meticulously.
This blog article aims to provide colleagues with important technical and clinical considerations based on our clinical experience and current scientific evidence when using monolithic zirconia in screw-retained fixed full arch cases.
Be aware of potential prosthetic complications
Even though zirconia IFCDPs have shown high cumulative survival rates with minimal prosthetic complications (Bidra et al. 2017, Papaspyridakos et al. 2019, Rojas Vizcaya F 2016), some possible technical complications we experienced in our patients (referring to those relevant to laboratory-fabricated components) were the chipping/fracture of veneering feldspathic ceramic material, de-bonding of the titanium interphases, and possible catastrophic fracture of the zirconia framework (Sailer et al. 2000). To reduce the potential risks of these complications and deliver long-lasting zirconia IFCDPs to our patients, significant technical and clinical considerations should be considered by the interdisciplinary team.
Clinical and technical considerations
The prosthetic volume
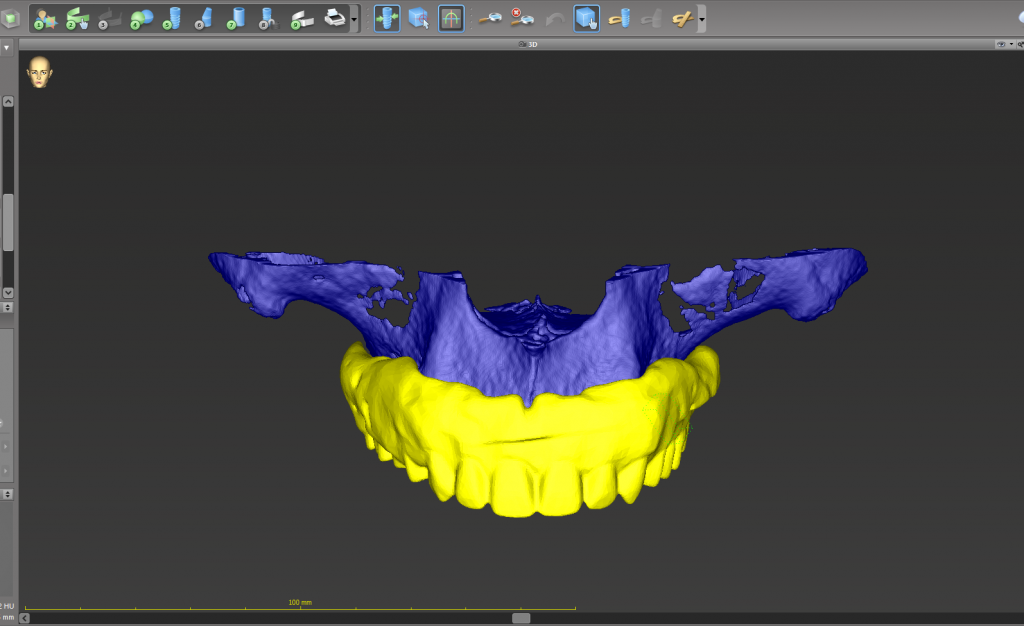
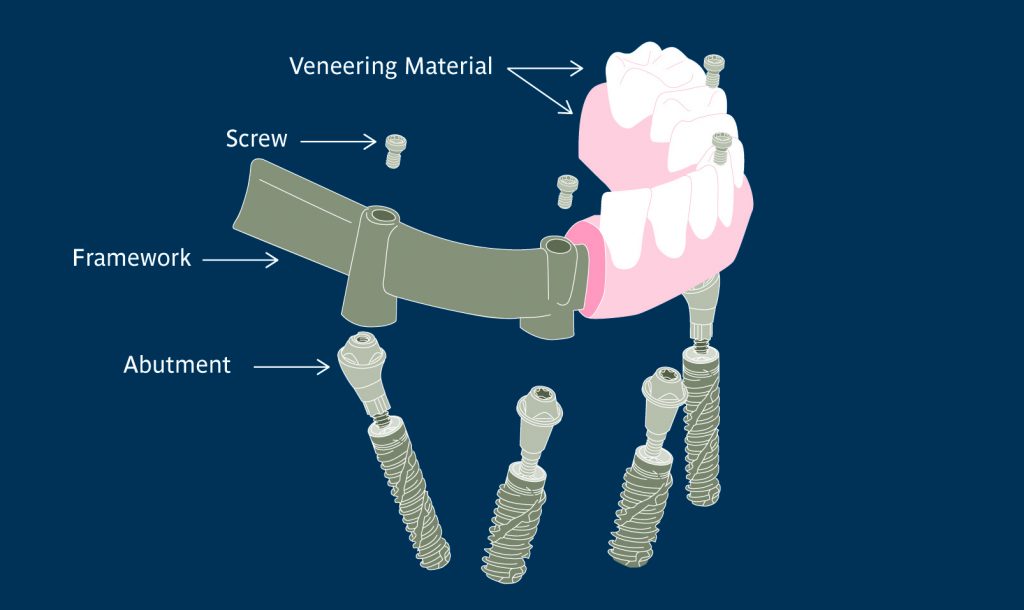
As described in the 2nd Edition of the SAC Classification in Implant Dentistry, this term refers to the 3D space required (mesiodistal, orofacial and interocclusal) for the prosthesis and implant components (framework, veneering material, abutments, copings, screws, etc.) allowing the ideal anatomy and optimal mechanical resistance (Fig. 2).
Depending on the type of prosthesis and material selected, there is more or less need for prosthetic space. For zirconia IFCDPs, the recommended interocclusal space is between 11 – 14 mm, measuring from the edentulous ridge (soft tissue) to the opposing occlusal table (Fig. 3).
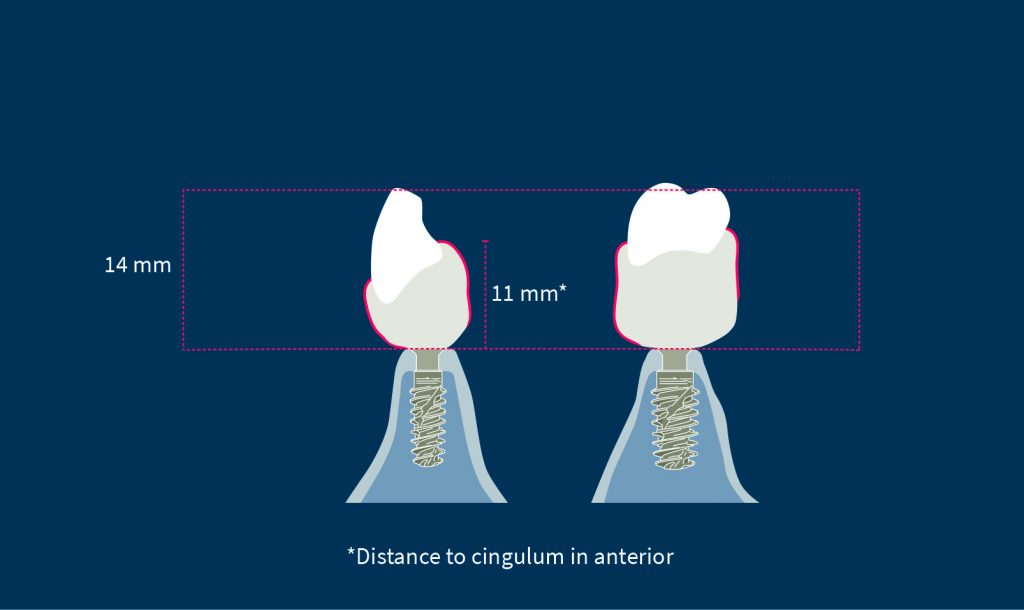
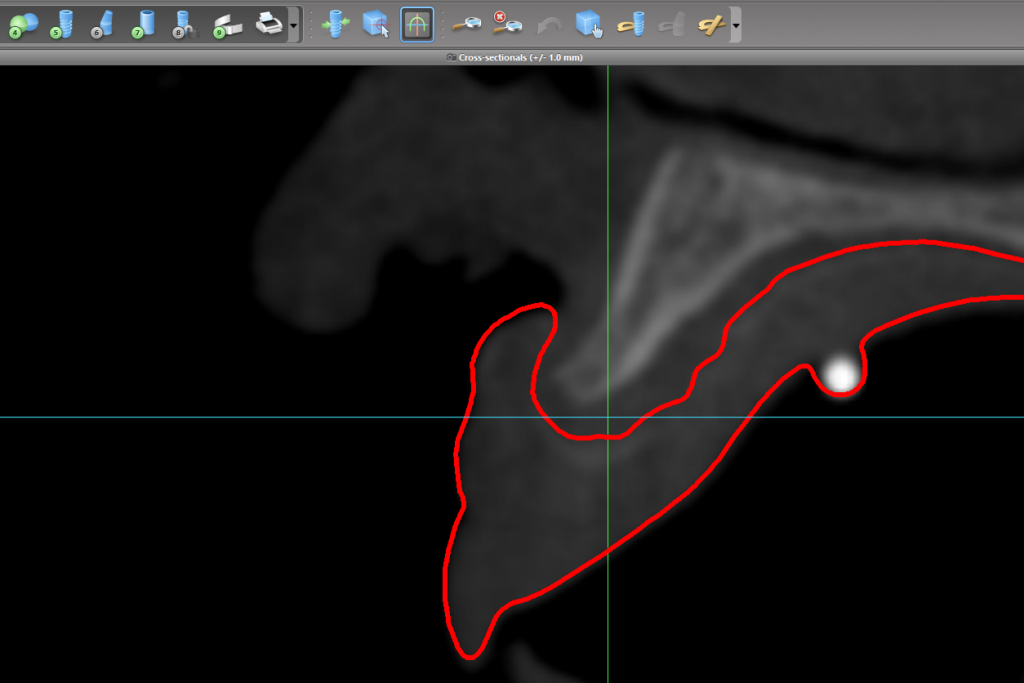
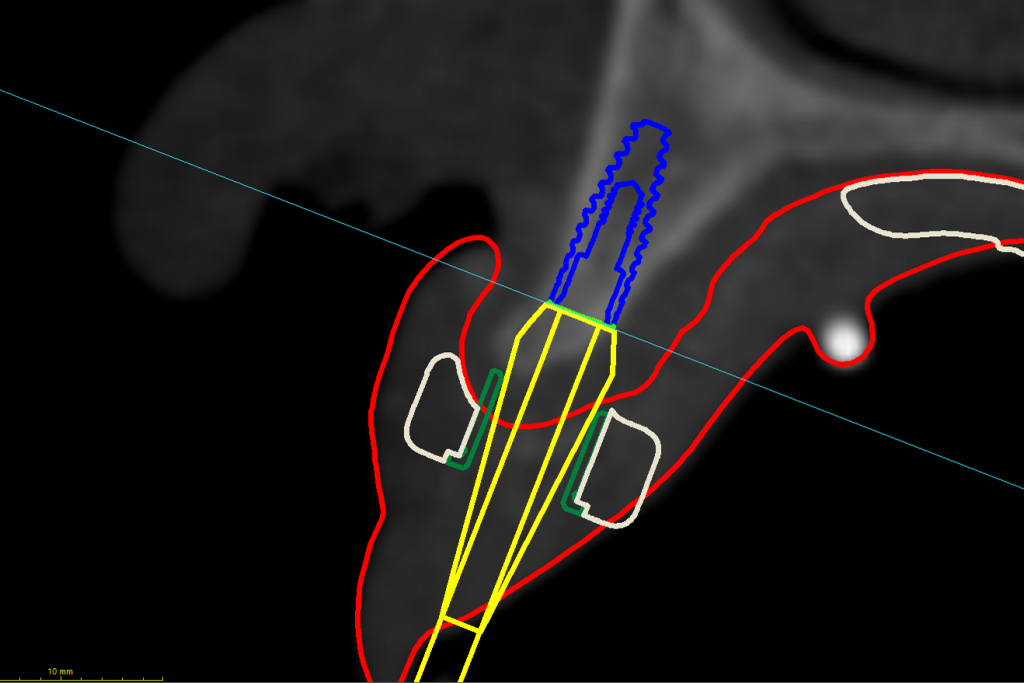
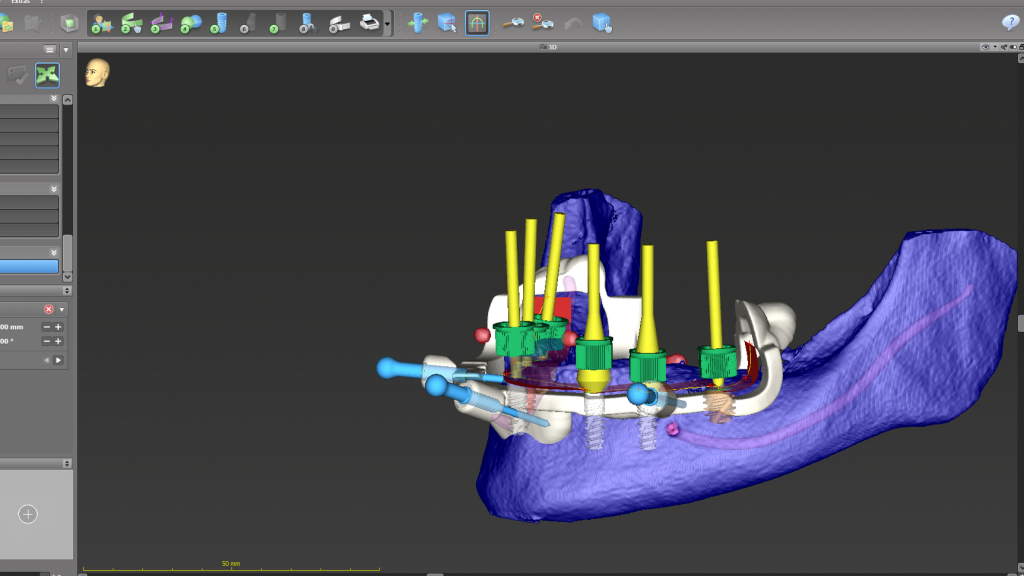
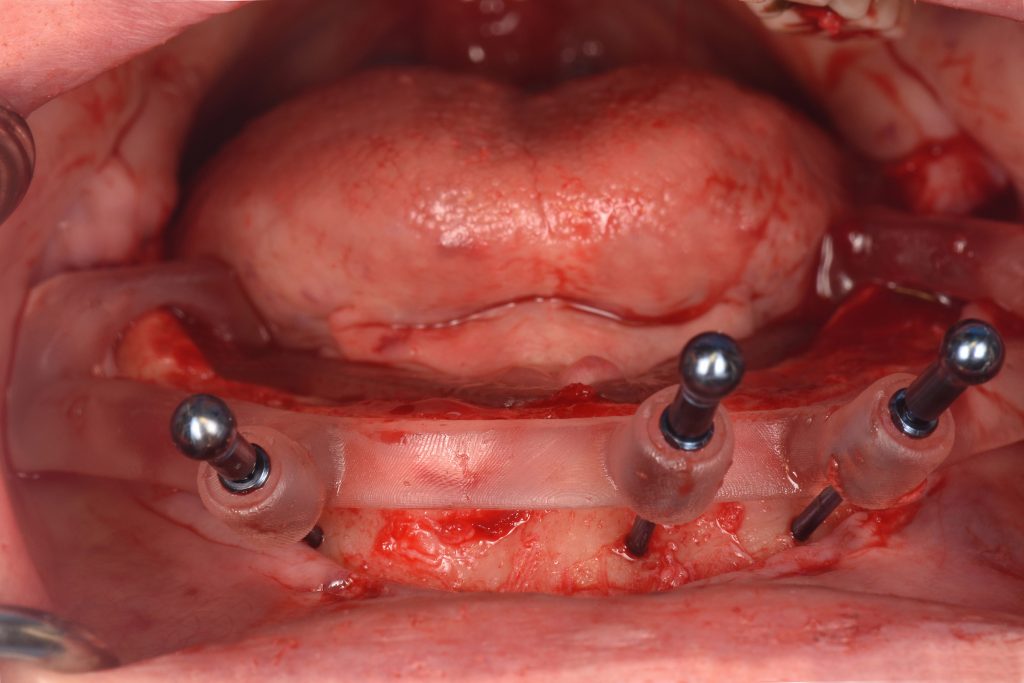
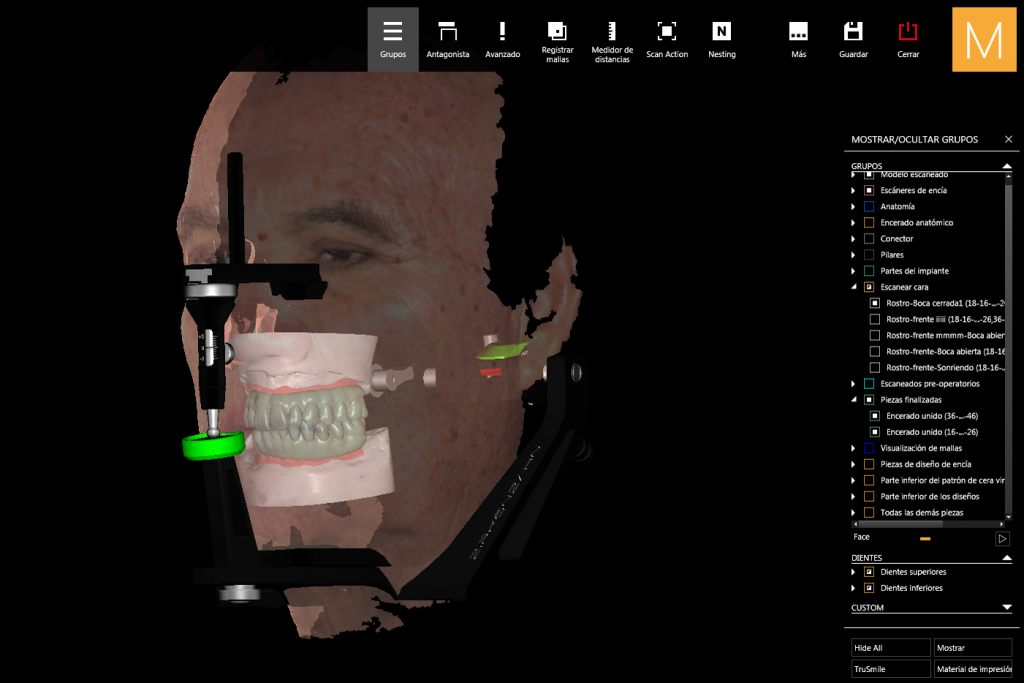
We consider the edentulous ridge an essential reference in this measurement since it is not uncommon that an excessive amount of soft tissue reduces interocclusal prosthetic space, thus jeopardizing the esthetics, mechanical strength, and durability of the final restoration. A dual scan protocol combined with implant planning software and static computer-aided implant surgery (sCAIS) allows for a prosthetic ideal implant position that considers the required prosthetic space (Figs 4a – 4c).
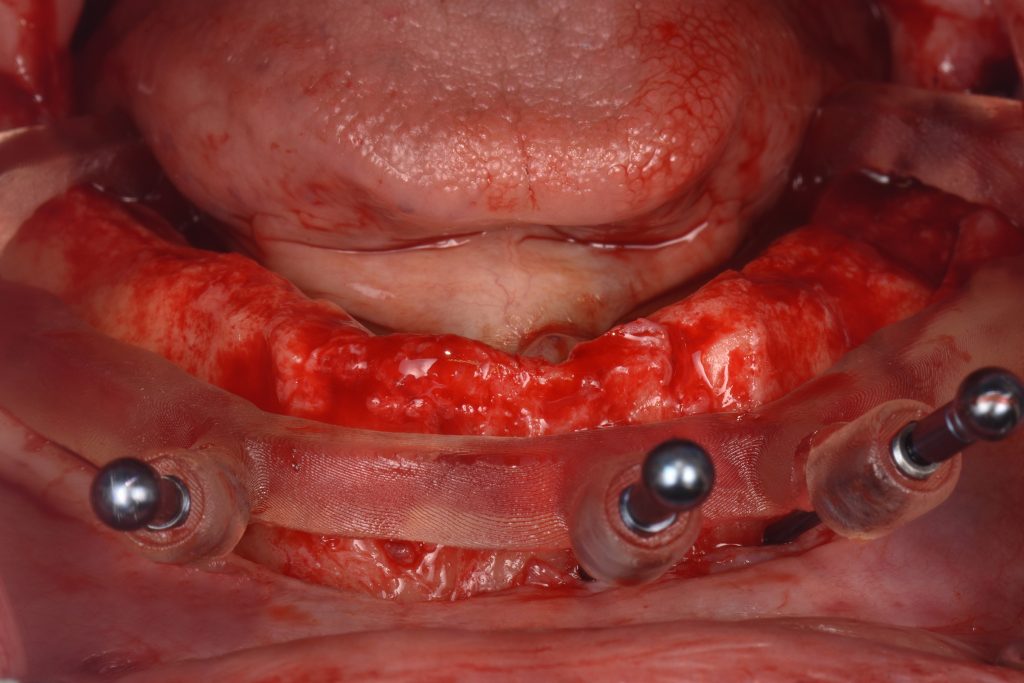
When prosthetic space is less than 11 mm (measured as above), an implant-supported fixed prosthesis without pink (FP1 and FP2), increasing the vertical dimension of occlusion (when indicated), or adjunctive therapy such as surgical bone reduction (Figs 5a – 5e) should be considered.
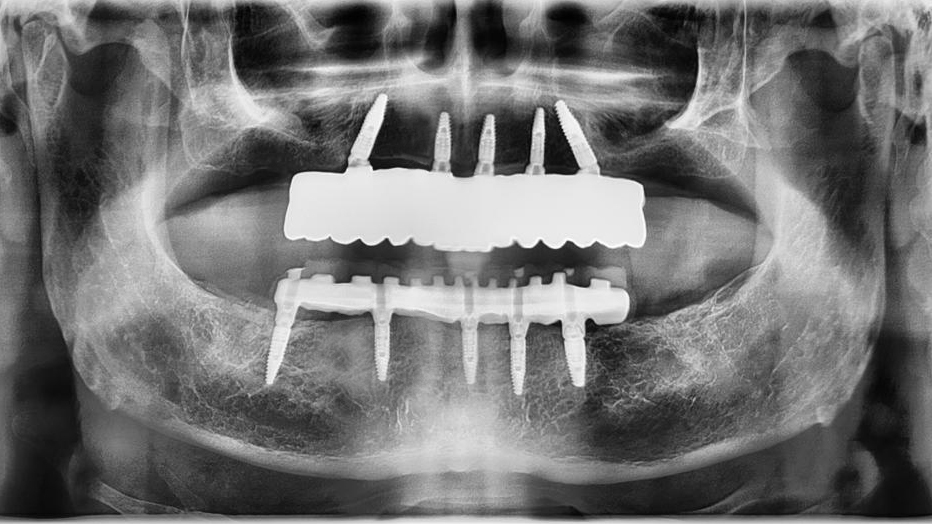
The number and distribution of implants
The number and distribution of implants to support a zirconia IFCDP in both maxilla and mandible should be considered a single factor during treatment planning. We recommend a thorough evaluation of critical aspects such as anatomical limitations, design of the prosthesis (one piece or segmented), opposing dentition (edentulous or dentate), interocclusal space, and financial status (Polido et al. 2018). Despite the controversy on this topic, the current scientific evidence supports the placement of 4 – 8 implants in the maxilla and 4 – 6 implants in the mandible. The adequate distribution of the implants ought to optimize the A-P spread, reducing distal cantilevers and an excessive span between implants (particularly when interocclusal space is limited), thus improving the support for the zirconia prosthesis.
Intentionally tilted and short implants can be considered an alternative when anatomical limitations are present (Figs 6 – 8).
Verification of the master cast using type IV stone jigs
As we know, the passive fit of an IFCDP is directly dependent on the accuracy of the impression and master cast fabrication. Even though a perfect passive fit is not feasible, obtaining the least possible misfit between the implants and prosthesis is our primary goal, especially for zirconia IFCDP. An absence of passive fit can lead to several prosthetic and biological complications that compromise the long-term success of the overall implant therapy.Regardless of the impression technique used, whether conventional (splinted open-tray impression technique) or digital (intraoral scanning), our recommendation is to always verify our master cast with a stone (type IV) verification jig before taking any further steps (Fig. 9).

If the verification jig is fabricated with a polymer material that can bend, the future zirconia IFCDP cannot fit! The minimal setting expansion and hardness are the main advantages of using type IV stone as the verification jig material. Therefore, as a brittle material, stone does not flex and will fracture in the mouth if the master cast is inaccurate.
Recently, the application of different technologies, such as digital photogrammetry in full arch implant impressions, has shown promising results in terms of trueness and precision (Hussein 2021).
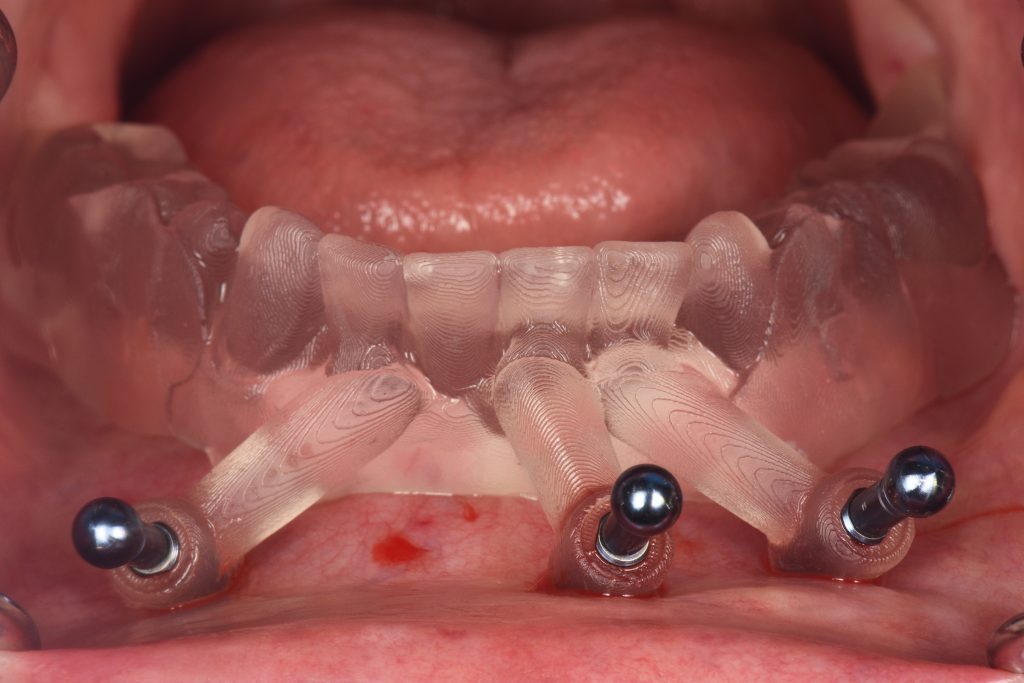
Use of prototypes before fabrication of the final restoration
CAD/CAM PMMA prototypes IFCDPs represent a cornerstone in all full arch cases in my practice. During this treatment’s transitional phase (6 to 8 weeks), we thoroughly assess the prosthodontic parameters before fabricating the final restorations. This evaluation comprises hygiene, functional and esthetic parameters. Any adjustments in the final zirconia IFCDP can induce phase transformation and micro-fractures of the material, reducing the mechanical strength of the prosthesis. Hence, testing the vertical dimension of occlusion, centric occlusal contacts, and dynamic occlusion in the transitional phase is critical for me (Figs 10 – 11).
Through this 6- to 8-week period, the patient can produce functional wear patterns and have any adjustments transferred to the laboratory by scanning the PMMA prototype to introduce the modifications into the CAD software.
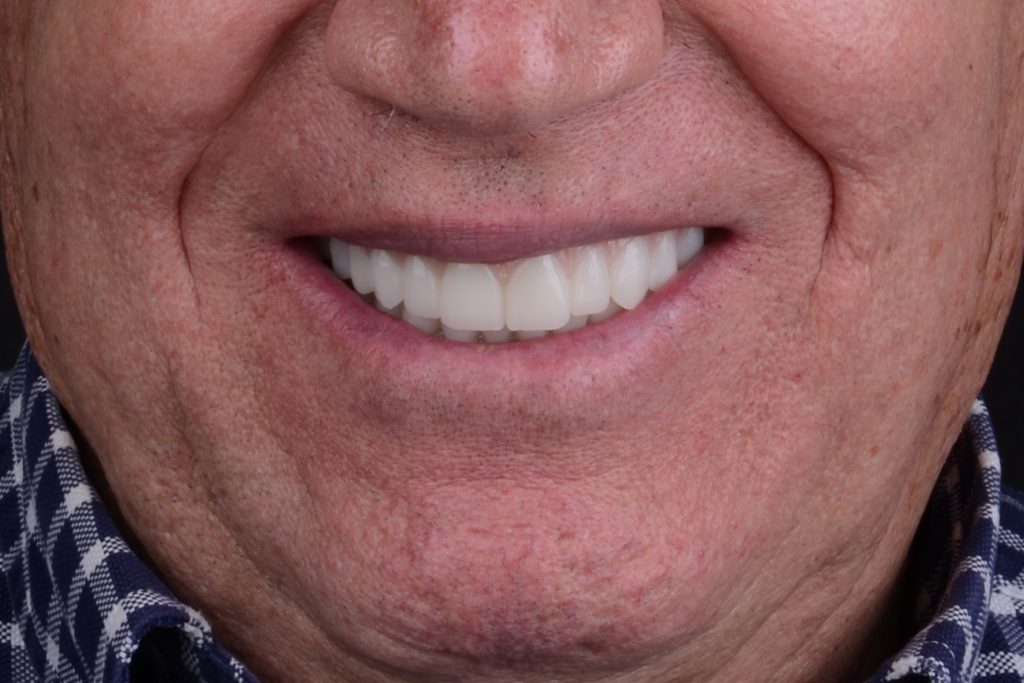
In addition to testing functional aspects, patients can use and approve the proposed esthetic design (Fig. 12), test phonetics, and the oral hygiene regimen through the prosthesis’s flat or convex intaglio surface (Fig. 13).
Not every zirconia is the same! Which type of zirconia (Y-TZP) should I select for IFCDPs?
Through modifications in sintering parameters (temperature and holding time), content/grain size of aluminum oxide, and percentage of yttria stabilizer, contemporary zirconia materials can have higher translucency (more cubic phase) and improved optical properties, making them an attractive alternative for monolithic restorations. However, we must be cautious when selecting zirconia in IFCDPs since higher translucency in ceramic materials is usually associated with lower mechanical properties. Using evidence-based restorative materials and rigorously following indications/recommendations from the manufacturer is critical. In our clinical practice, we usually indicate the strongest type of zirconia available for these reconstructions: the 3Y zirconia (3 mol% yttria).
Abrasiveness for opposing dentition
When I select zirconia as the final material for an IFCDP, there are two major reasons why I choose to design a full monolithic prosthesis, particularly in functional areas (Figs 14a – 14c).
The first is to avoid the high risk of chipping of veneering feldspathic ceramic. The second refers to the wear on the opposing dentition. As veneering feldspathic ceramic may fracture during wear, it creates a rough/sharp surface that abrades the opposing enamel. Contrarily, it has been shown that high polished monolithic zirconia produces significantly less wear on the opposing dentition than glazed restorations and veneering ceramics (Lawson et al. 2014).
Therefore, my preference is to avoid glaze application in the functional areas, keep away from adjustments after sintering, and follow a meticulous polishing protocol with extra-oral polishing kits and polishing pastes. Remember that surface roughness is the main cause of wear on the opposing dentition, not the hardness of the material!
Proper handling of the material in the laboratory
Optical and mechanical properties of zirconia IFCDPs are strongly influenced not only by the composition and homogeneity of the raw material but also by several steps during the fabrication of the prosthesis in the laboratory (Stawarczyk et al. 2013). Those critical steps are related to the milling unit, the burs, the color liquid infiltration steps (risk of contamination), the sintering unit (cleaning and maintenance), sintering parameters (heating rate, temperature, holding time, calibration of heating elements, etc), the proper selection of the veneering porcelain (if required) which needs to be compatible with the CTE of the zirconia, the firing cycles, slower heating/cooling rates, and last but not least the finishing/polishing protocol of the final restoration. Conducting all the laboratory steps with controlled protocols following the manufacturer’s instructions is fundamental to the ultimate quality of the restoration.
Framework design and limited feldspathic ceramic application
As clinicians, our ultimate goal is to fabricate an implant-supported zirconia restoration with the highest quality in terms of esthetics and natural appearance and mechanical resistance, reducing the risk of potential technical complications. To achieve this goal, our preference is to fabricate the final framework in monolithic design as follows:
- Using the high-quality milling refinement protocol normally given by the software CAD and small burs (Figs 15a – 15b).
- If desired, we can improve the detailed anatomy, macro/micro texture and characterization using manual instruments (Fig. 16).
- Performing a modified cutback design manually or digitally, maintaining all functional areas in monolithic zirconia and limiting the veneering porcelain application to the incisal third of the buccal surface (Fig. 17).
- Subsequently, color liquid infiltration following the recommendations of the manufacturer and the desired effects by the interdisciplinary team and patient (Fig. 18).
- After coloring, the framework needs to be sintered in the sintering furnace according to the manufacturer’s parameters (Fig. 19).
- Finally, application of the veneering porcelain in the gingiva and selected non-functional areas, finishing and thorough polishing are carried out (Fig. 20).
Using titanium interfaces
To connect ceramic monolithic reconstructions to the implants (directly or indirectly using intermediate abutments), our preference and recommendation is the use of titanium bases. The incorporation of prefabricated titanium abutments into the IFCDP must follow a meticulous bonding protocol and this step should be performed in a verified master cast. The above is key to reduce the risk of the abutments de-bonding from the zirconia prosthesis; the lack of passive fit and incorrect bonding protocols for titanium bases represent the main causes of de-cementation.
Once they have bonded, the fixed monolithic reconstruction can be screwed to the implants as a single piece. In some cases when the span between implants is excessively long, our preference is to design a milled titanium bar supporting the monolithic zirconia reconstruction (rail/overlay design). In this type of design, the milled bar must be bonded to the final zirconia overlay following the same principle as for individual titanium bases to produce a one-piece reconstruction (Figs 21a – 21b). After adhesive cementation, we recommend clearing residual cement and intaglio surface polishing.
Material selection for the edentulous opposing arch in bi-maxillary reconstructions
Material selection for the mandibular edentulous opposing arch in patients who wear a maxillary monolithic zirconia IFCDP has been a controversial topic with no clear conclusions. Based on my clinical experience rehabilitating such clinical scenarios, there are 3 major aspects that influence my selection criteria:
- The opposing material should compensate for the so-called “clicking” sound produced in cases of zirconia opposing zirconia. This sound has become a frequent complaint from patients treated with bi-maxillary zirconia implant-supported rehabilitations.
- The opposing material should permit progressive wear, transferring possible technical complications through the years of service just to one arch, acting as the weak link.
- Patient’s functional assessment. Parafunctional habits present a higher risk of minor and major technical/mechanical complications compromising treatment success.
For the aspects above, my preference when I rehabilitate both fully edentulous arches is to combine a maxillary monolithic high-polished zirconia IFCDP with a mandibular IFCDP fabricated in either densely high cross-link or high-performance polymers (Figs 22a – 22b).
Conclusion
Based on my clinical experience and current scientific evidence, the full arch fixed implant-supported reconstruction using monolithic zirconia as the final material has shown to be highly predictable. To improve long-term treatment success, 10 critical considerations were highlighted and recommended in this ITI blog article.