In dentistry, making evidence-based decisions is essential for ensuring effective patient care and efficient practice management. Recent studies highlight the cost-effectiveness of periodontal treatments compared to dental implants, offering important insights for treatment planning. Evidence-based dentistry (EBD) supports this approach by combining clinical expertise, patient preferences, and the latest scientific findings. This framework enables practitioners to deliver high-quality care, reduce potential risks, and use resources wisely. By integrating solid evidence into clinical decisions, dental professionals can better evaluate treatment efficacy, manage costs, and align care with individual patient needs.
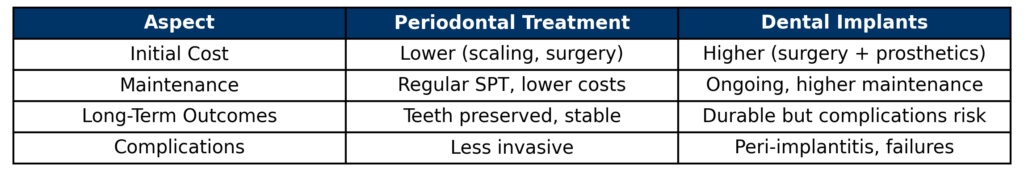
The rising prevalence of periodontal disease and tooth loss has encouraged clinicians to weigh the benefits of preserving natural teeth through periodontal treatments against replacing them with dental implants. Recent research emphasizes the importance of cost-effectiveness in treatment planning, as both approaches differ significantly in initial costs, long-term maintenance, and clinical outcomes. Periodontal treatments, such as scaling, root planing, and supportive periodontal therapy (SPT), aim to maintain compromised teeth, while dental implants offer a durable but costly alternative. Understanding which option provides better economic and clinical value is critical for informed decision-making in dental care. A systematic review by Afrashtehfar et al. (2024) addresses this question by synthesizing evidence on the cost-effectiveness of these interventions, offering valuable insights for clinicians and patients.
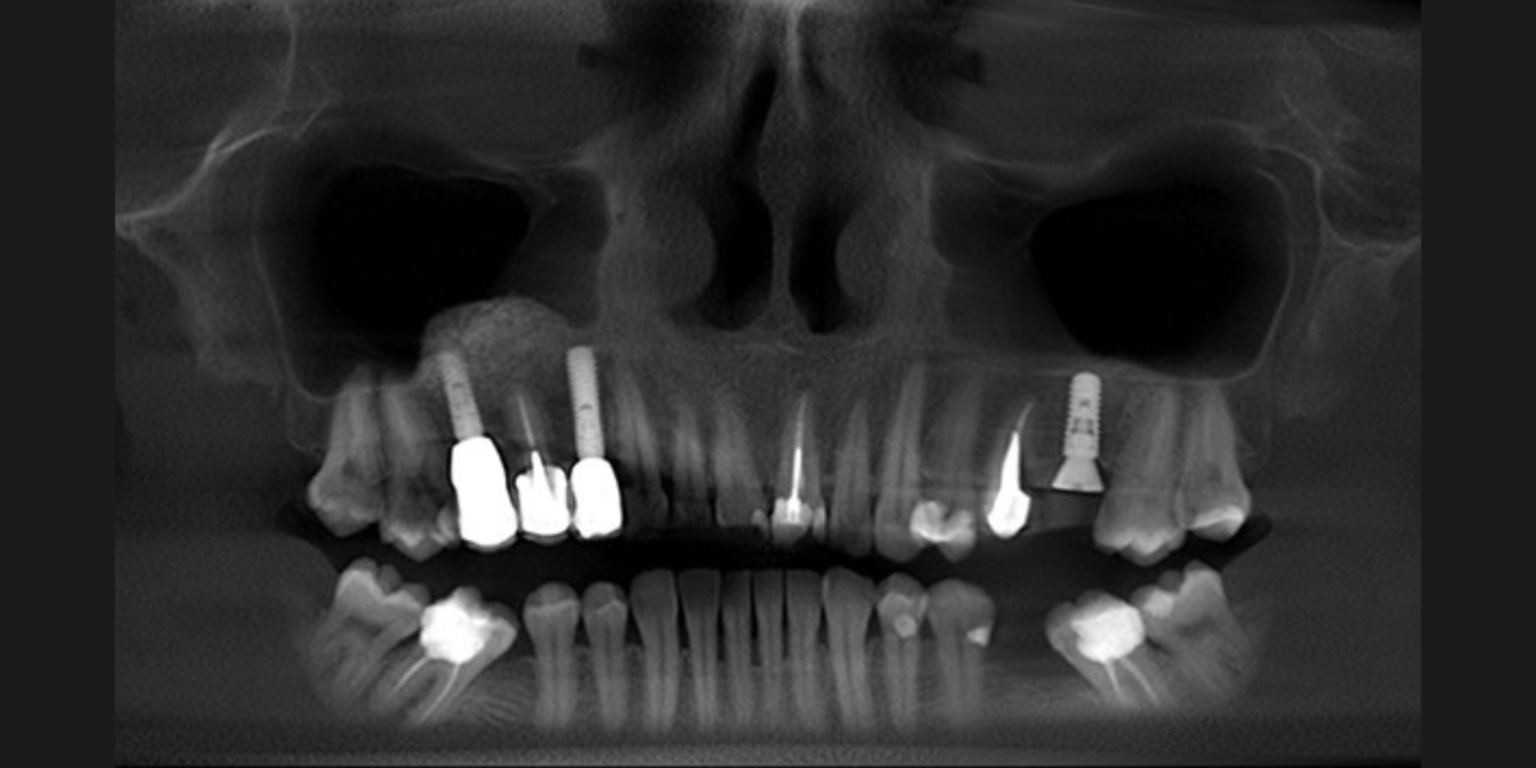
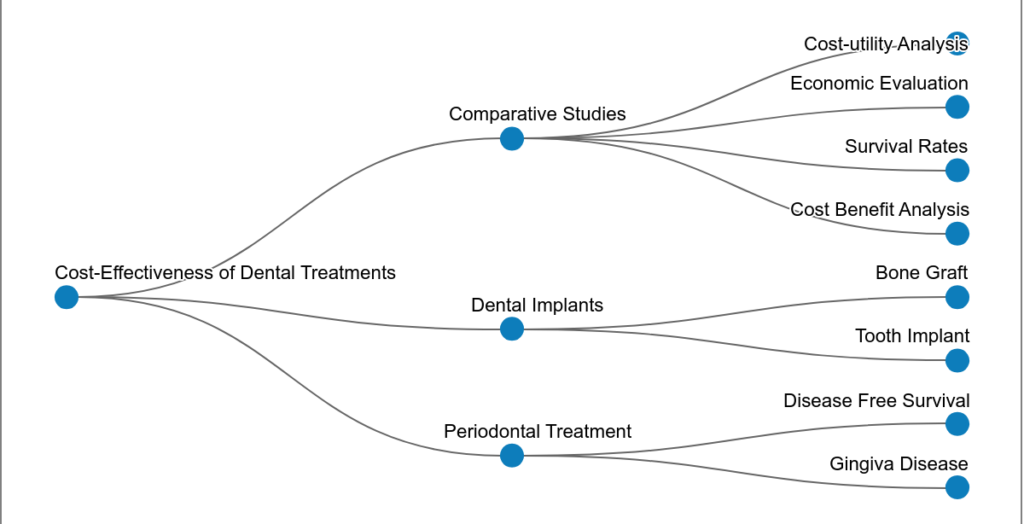
The review by Afrashtehfar KI, Assery NM, Alblooshi KAK, and Schmidlin PR (2024) identified 633 studies on periodontal treatment and 114 on dental implants through a comprehensive search of databases. To ensure high-quality evidence, the authors applied strict inclusion criteria: (1) studies had to directly compare the cost-effectiveness of periodontal treatments (e.g., non-surgical or surgical therapies, SPT) or dental implants; (2) they needed to report quantitative economic outcomes, such as direct costs (e.g., treatment, maintenance) or indirect costs (e.g., patient time, complications); (3) they required a minimum follow-up period of 36 months to capture long-term outcomes; (4) only peer-reviewed studies published in English between 2008 and 2018 were considered; and (5) studies had to employ robust methodologies, including retrospective, prospective, or model-based analyses, with clear reporting of data sources and assumptions. After rigorous screening using Joanna Briggs Institute (JBI) critical appraisal tools and adherence to PRISMA guidelines, 9 studies on periodontal treatment and 3 on dental implants were included. These studies, predominantly from Germany, featured a mix of retrospective, prospective, and model-based analyses. Follow-up periods ranged from 36 months to 33 years, offering a broad perspective on long-term outcomes.
Key findings
1. Cost implications
• Periodontal treatment: Costs increase with disease severity. Surgical treatments are more expensive than nonsurgical ones, with supportive periodontal treatment (SPT) representing the highest cost share.
• Dental implants: Maintaining implants is generally more costly than maintaining teeth, especially in cases of peri-implantitis. A 2013 study found that maintaining implants was five times costlier than maintaining teeth.
2. Specific cost data
• Chronic periodontitis: Total treatment costs per tooth were €222 ± €98 over 18.7 years.
• Aggressive periodontitis: Costs were €267 ± €148 over 16.9 years.
• Regular SPT: Cost €806 per tooth per year over 28.7 years, with significant cost variations across studies.
• Implant-supported crowns (ISCs), identified as the most expensive treatment option in a 2018 study, carry significant cumulative costs—not only from the initial surgical placement but also from ongoing maintenance, potential complications, and long-term follow-up care.
3. Comparative cost-effectiveness
• Only one study directly compared costs for the same patient, finding periodontal treatment to be more cost-effective than implants.
• Costs increased with irregular SPT, aggressive periodontitis, and specialist treatments compared to regular SPT, chronic periodontitis, and treatments by general dental practitioners.
4. Quality of studies
• The quality of included studies scored between 45% and 84.6%, indicating moderate to high quality. Methodological issues included unclear strategies for handling confounding factors and incomplete follow-up.
Role of practice-based research networks
Practice-based research networks (PBRNs) play a crucial role in enhancing the evidence base in implant dentistry. These networks consist of practicing dentists and academic researchers collaborating to investigate real-world clinical questions. By participating in PBRNs, dental practitioners can contribute to large-scale studies that reflect everyday clinical practice, leading to findings that are highly relevant and applicable. For instance, the National Dental PBRN has established the first dental implant restoration registry, which aims to gather extensive data on implant outcomes and complications (https://www.nationaldentalpbrn.org/). Such initiatives help bridge the gap between research and practice, ensuring that clinical decisions are informed by robust, practice-based evidence.
Although, dental implants are an effective solution for replacing missing teeth, they often involve higher long-term costs due to surgical placement, prosthetic components, ongoing maintenance, and the risk of biological or mechanical complications. In contrast, retaining and managing periodontally compromised teeth, when clinically feasible, is generally more cost-effective over time. This approach often requires less invasive intervention, lower maintenance costs, and fewer complications. Therefore, when planning treatment, it is crucial to weigh not only the clinical prognosis but also the long-term financial and biological implications of each option. Evidence suggests that in many cases, preserving natural teeth through periodontal therapy offers a more sustainable and economical path for both patients and healthcare systems.
There is a pressing need for more studies comparing the long-term cost-effectiveness of saving teeth versus replacing them with implants. Such research should consider various factors to aid in informed clinical decision-making.