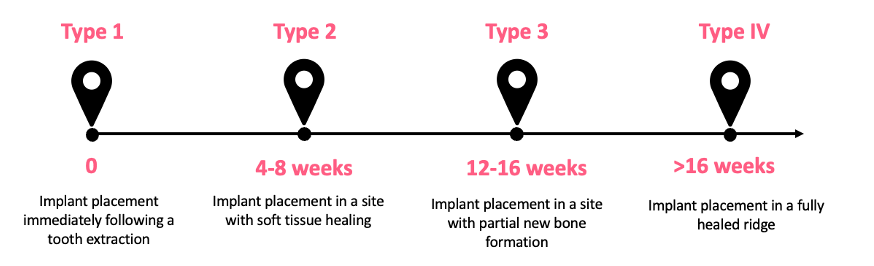
Timing of implant placement, definition of terms
Historically, dental implants were predominantly placed into a completely healed site after several months (Adell et al. 1981, Branemark et al. 1977). Nowadays, clinicians have an important choice to make when selecting the timing for implant placement between four treatment options (Fig.1). Unfortunately, when it comes to the timing of implant placement, the “one fits all” approach cannot be taken, which introduces challenges to clinical decision-making as soon as a tooth is planned for extraction.
Esthetic results can be attained regardless of the timing of implant placement. Based on the data presented in the systematic review by Francisco and co-workers (Francisco et al. 2021), assessing esthetic outcomes such as mid-facial mucosa changes, papilla height, and esthetic indices, no specific recommendation can be made in favor of a particular timing for implant placement. Given that the current literature also doesn’t favor a specific timing for implant placement or loading in terms of implant survival, clinicians should carefully weigh all pertinent biological, anatomical, and esthetic factors before deciding on one of these procedures (Donos et al. 2021).
This article aims to discuss different timing options for implant placement, highlighting advantages and disadvantages based on the new evidence, and to provide some tips for decision-making.
Type I – Immediate implant placement
Due to high patient demand, busy lifestyles, and time constraints, immediate implant placement is becoming the clinician’s ultimate first choice. However, is it always a suitable and reliable method in terms of the long-term prognosis?
Immediate implant placement provides great benefits: it reduces the number of surgical procedures required, improves overall treatment time and cost-efficiency, and provides an opportunity to attach a provisional restoration (Tonetti et al. 2019, Hammerle et al. 2009).
In contrast, it is more complex to achieve primary stability, and simultaneous hard and soft tissue grafting procedures demand more advanced clinical skills. Clinicians should bear in mind the dimensional changes of the alveolar ridge that are going to take place during the healing period that immediate implant placement fails to prevent (Araujo et al. 2005, Araujo et al. 2006a, Botticelli et al. 2004).
Type 1 site selection criteria (Chen and Buser, 2014, Morton et al. 2023):
- Intact socket walls – This can be evaluated with a diagnostic CBCT, however, it should also be assessed following the extraction.
- Facial bone wall at least 1 mm in thickness – Thin facial bone is more prone to vertical resorption, which may lead to resorption of the graft placed into the facial peri-implant gap, resulting in exposure of the rough surface and midfacial recession of the peri-implant mucosa (Chen et al. 2007, Sanz et al. 2017).
- The horizontal distance between the implant and the facial bone “jumping gap” – The presence of at least a 2-mm gap or larger increases implant survival (Hamilton et al. 2023). This is in line with previous studies which demonstrated that a larger horizontal gap leads to a greater amount of bone covering the buccal implant surface (Araujo et al. 2006b) and promotes a thicker buccal bone wall (Levine et al. 2022). Grafting the gap with deproteinized bovine bone mineral (DBBM) and immediate grafting reduces the bone dimensional changes (Seyssens et al. 2022).
- Thick soft tissue phenotype – Sites with thick soft tissue phenotype, defined as > 2 mm (Avila-Ortiz et al. 2020), have less risk of midfacial mucosa dehiscence (Cordaro et al. 2009). Systematic reviews have indicated that the use of a connective tissue graft (CTG) should be considered when a higher risk of dehiscence is expected (e.g. thin phenotype or reduced buccal bone thickness) since it seems to have a protective effect (Seyssens et al. 2021).
- No acute infection at the implant placement site – In the presence of acute infection, it is likely that one or more socket walls are damaged, and inflamed soft tissue might be more challenging to handle. Nevertheless, a chronic periapical infection associated with the tooth is not a contraindication if primary stability can be achieved.
- Healthy adjacent teeth
- Sufficient bone (at least 3 mm) apically, palatally to the socket or interseptally in molar areas to provide primary stability (Hamilton et al. 2023).
- Ability to place an implant in the correct three-dimensional position for restoration.
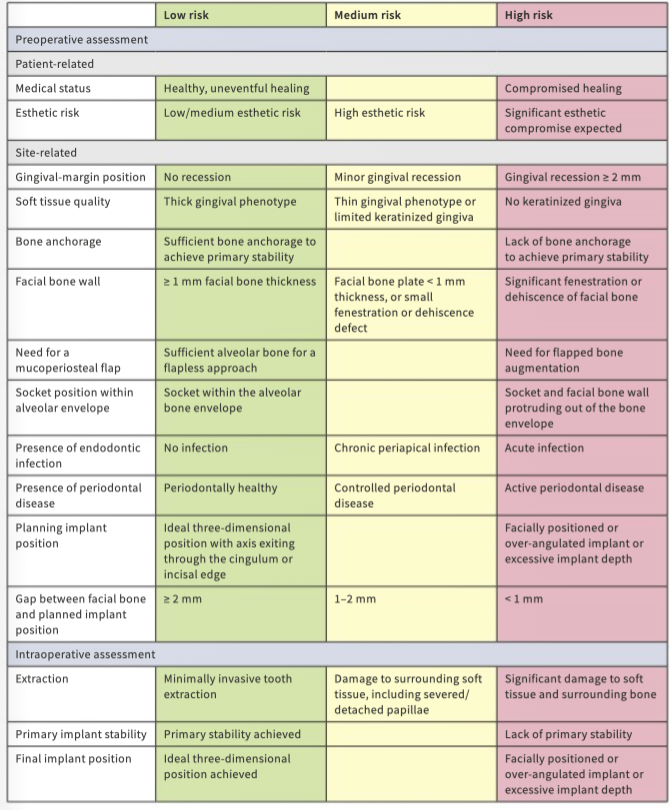
A very detailed summary of risk assessment criteria for immediate implant placement, clinical cases and the latest guidelines can be found in the latest ITI Treatment Guide Volume 14.
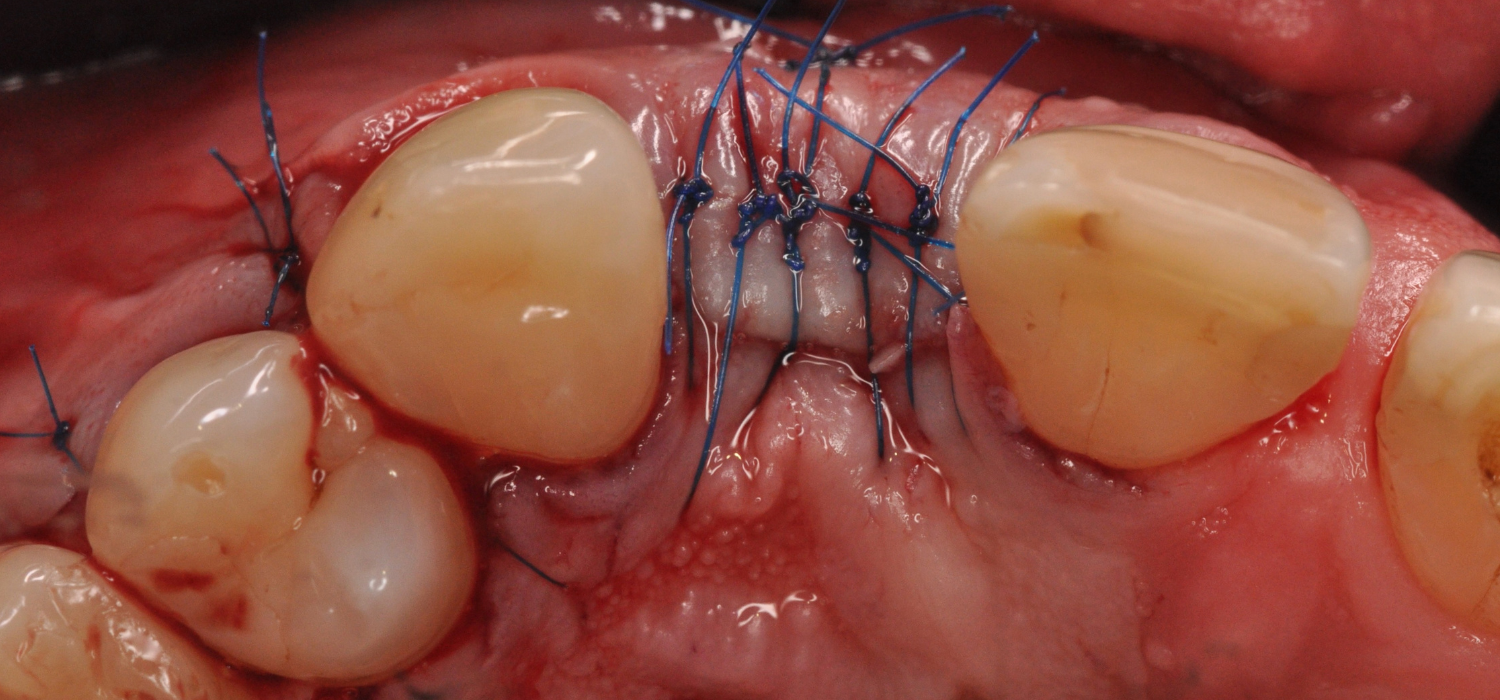
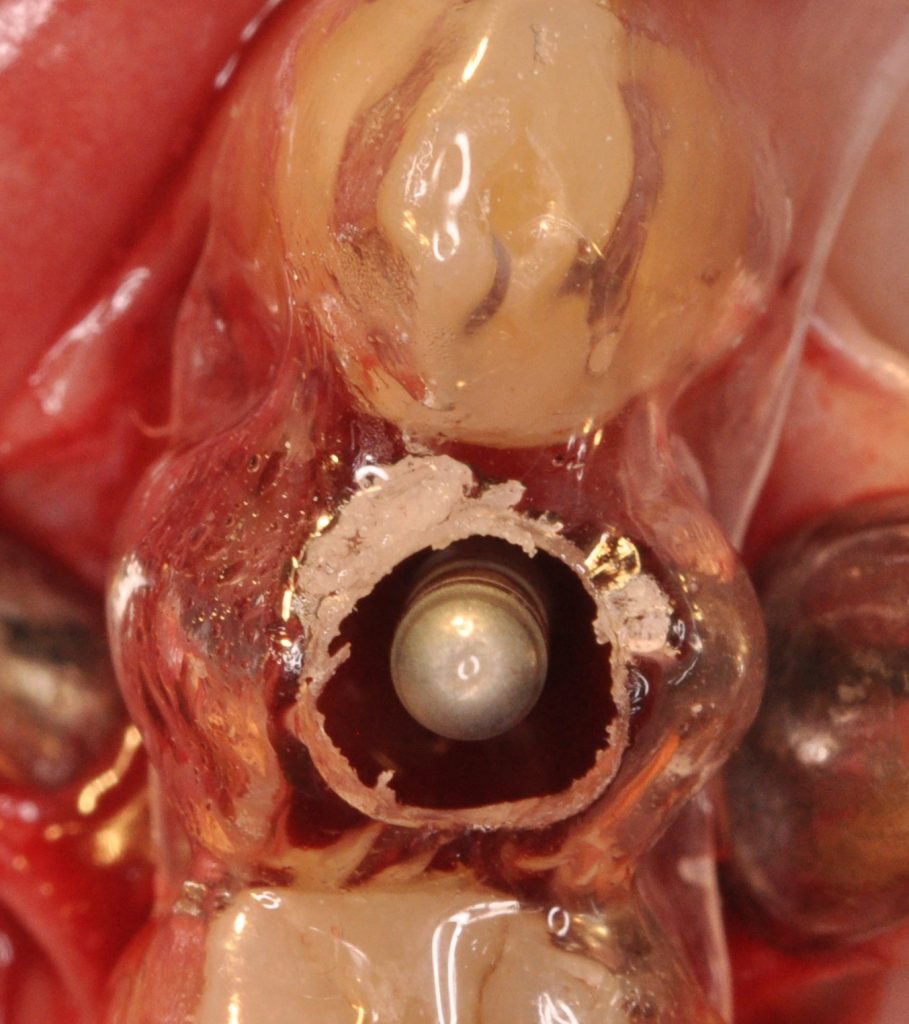
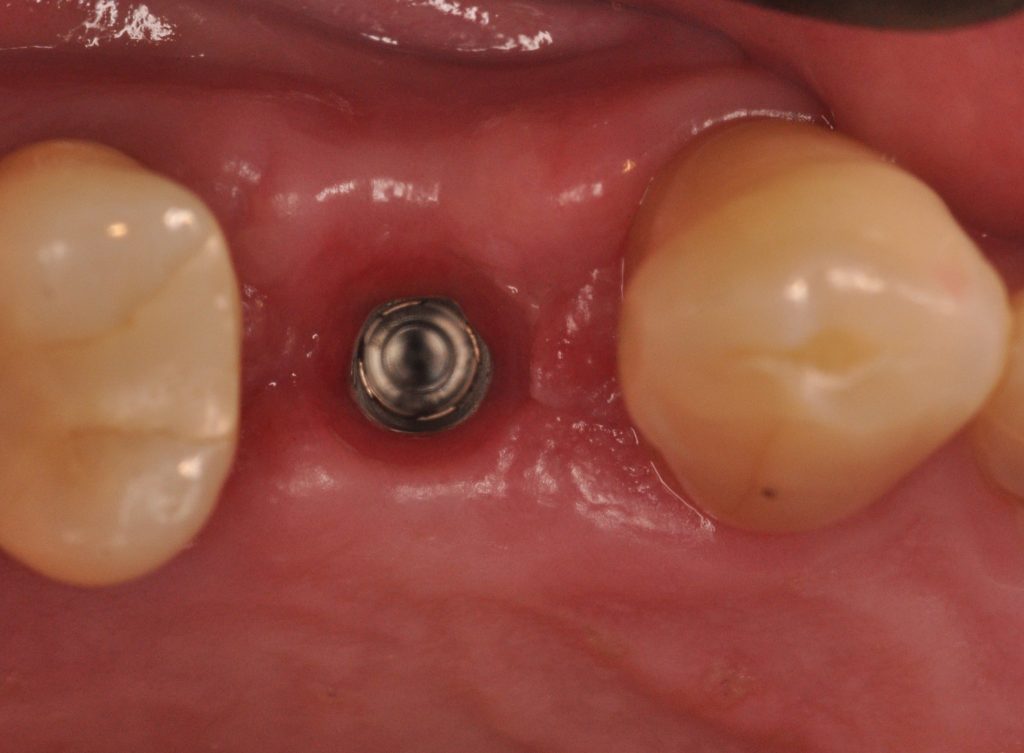
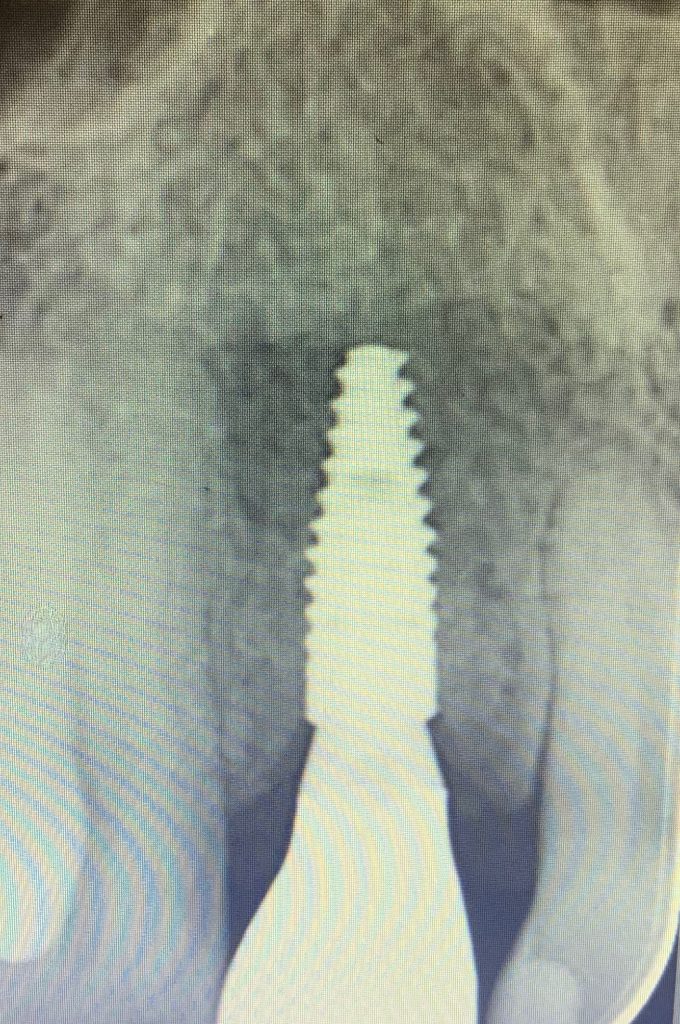
An example of an immediate implant placement is depicted in Fig. 3. The patient was referred by the endodontist for replacement of the maxillary second premolar (tooth 15) with a dental implant due to a fracture. The patient was healthy and a non-smoker. Clinical examination revealed that the surrounding teeth and soft tissue had no structural damage. A cone-beam tomography (CBCT) was acquired to evaluate buccal/palatal walls and proximity to the sinus. A risk assessment was performed pre- and intraoperatively, classifying this case as a low risk. A 4.1 Straumann BLT implant was placed, and primary stability was achieved. One must be prepared to abort implant placement if primary stability cannot be achieved.

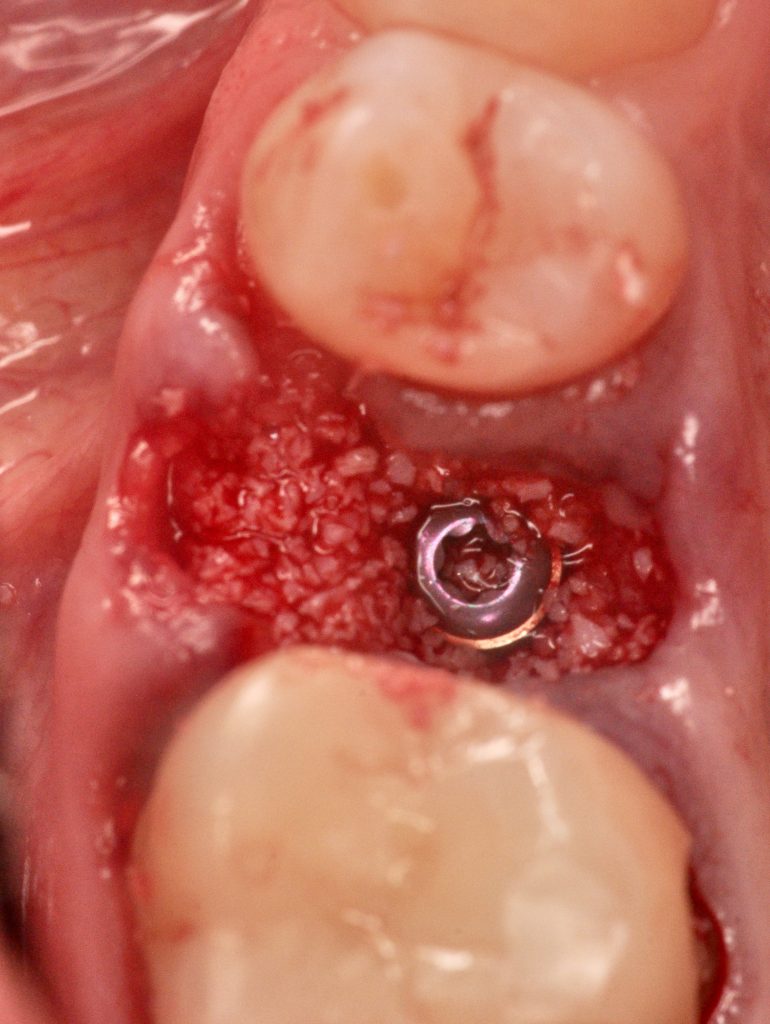

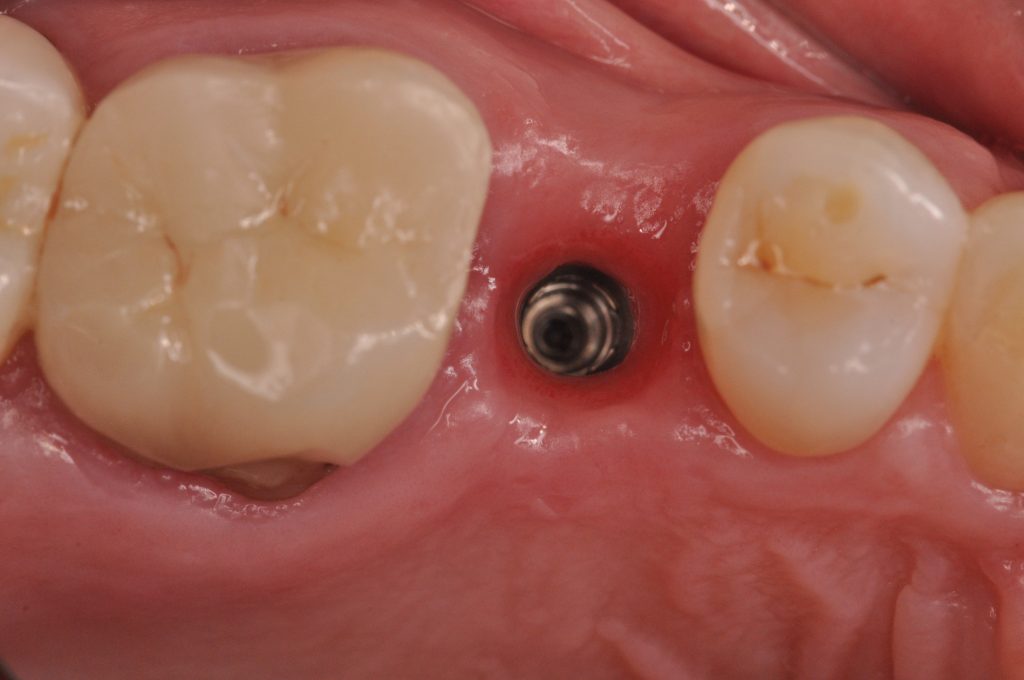

The other challenge of immediate implant placement is to achieve protection of the implant and biomaterials. In this case, a plasma rich in growth factors (PRGF) membrane was adapted and sutured. The other option would be to create a customized chair-side-made or lab-fabricated sealing socket abutment (SSA) (Finelle and Lee, 2017). Alternatively, the delivery of an immediate provisional restoration offers some advantages in the esthetic area. According to the latest systematic review, the reported survival rate of Type 1A implants in the maxillary esthetic zone was 99% (ranging from 97.8-99.5%) at 1 year and 95% (89.6-97.4%) at 5 years (Wittneben et al. 2023). Esthetic results remained stable at 1 year with an overall effect size in papilla height of -0.71 mm and midfacial recession of -0.15 mm. Evidence to support immediate loading at the posterior sites is scarce and might involve higher risks due to the higher masticatory loads (Gallucci et al. 2018). For immediate loading, the following criteria should be met: insertion torque >35 Ncm, no direct occlusal contact, no parafunction (Hamilton et al. 2023).
The use of a computer-guided surgical template is highly recommended to achieve an optimal restoratively driven 3D implant position, especially in the esthetic zone. Pilot drilling often has to start in the apical third of the palatal wall and the bur might slide away when touching the angled flat wall (Buser et al. 2017). A recent randomized clinical trial demonstrated a significantly higher angular deviation in the free-hand group compared to static guided surgery (6.09° vs 0.83°) during immediate implant placement (Chandran et al. 2023). Results from an in-vitro study indicated that even when static computer-aided implant surgery (sCAIS) was used, the final implant position was significantly affected by the morphology of the alveolar ridge (Raabe et al. 2023, Dulla et al. 2023). Implants placed in healed alveolar ridges with sCAIS showed significantly lower mean deviation compared to implants placed in fresh extraction sockets with the greatest difference in angular deviation (1.86° vs 4.33°). The position deviations are initiated with the first implant osteotomy and persist throughout the drilling sequence (Raabe et al. 2023).
1.2 Type II – implant placement with soft tissue healing
One of the advantages of Type II placement is the soft tissue healing. A 7-fold increase in soft tissue volume has been observed (Chappuis et al. 2015), providing 3-5 mm of keratinized mucosa (Schropp et al. 2003).
Two-thirds of the alveolar ridge width reduction happens in the first 3 months following tooth extraction (Schropp et al. 2003). Therefore, the results from a systematic review which showed 13% less bone height reduction and 19.8% less width reduction favoring early implant placement, compared to Type IV implant placement, make Type II protocol very attractive. This approach has shown good esthetic outcomes and low risk for mucosal recession (Chen and Buser, 2014).
On the other hand, Type II implant placement may not be appropriate where primary implant stability is compromised due to the morphology of the socket or apical defect, often requiring extended simultaneous bone grafting procedures which add surgical complexity and demand a higher level of surgical skills.
Type II case selection criteria:
- Extended (>50%) buccal or palatal bone defect (Tonetti et al. 2019)
This approach might be particularly useful if > 50% of the socket wall is missing and hard-tissue preservation can only be performed using guided bone regeneration with flap elevation (Jung et al. 2018). In the presence of large defects, it may sometimes be difficult or impossible to achieve primary tension-free wound closure, due to the lack of soft tissue at the time of tooth extraction. At the same time, significant coronal advancement of the flap by periosteal release might cause displacement of the mucogingival line compromising the esthetic outcome (Benic and Hammerle, 2014). In such cases, spontaneous socket healing can be allowed for 4-8 weeks to facilitate soft tissue healing and volume increase, followed by a staged bone augmentation procedure or implant placement with simultaneous hard and soft tissue grafting (Benic and Hammerle, 2014).
- Presence of acute infection – This approach allows pathology associated with the extracted tooth to resolve prior to implant placement.
- Insufficient bone volume for an immediate implant placement
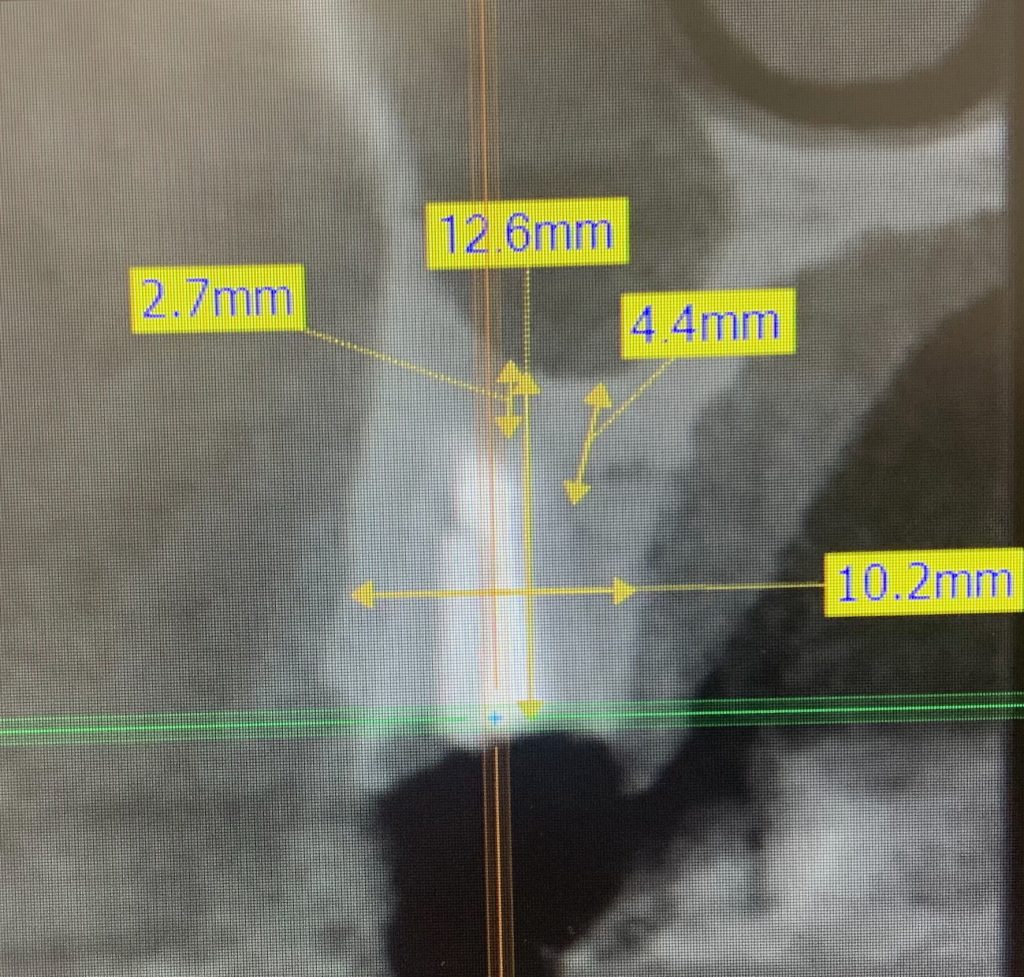
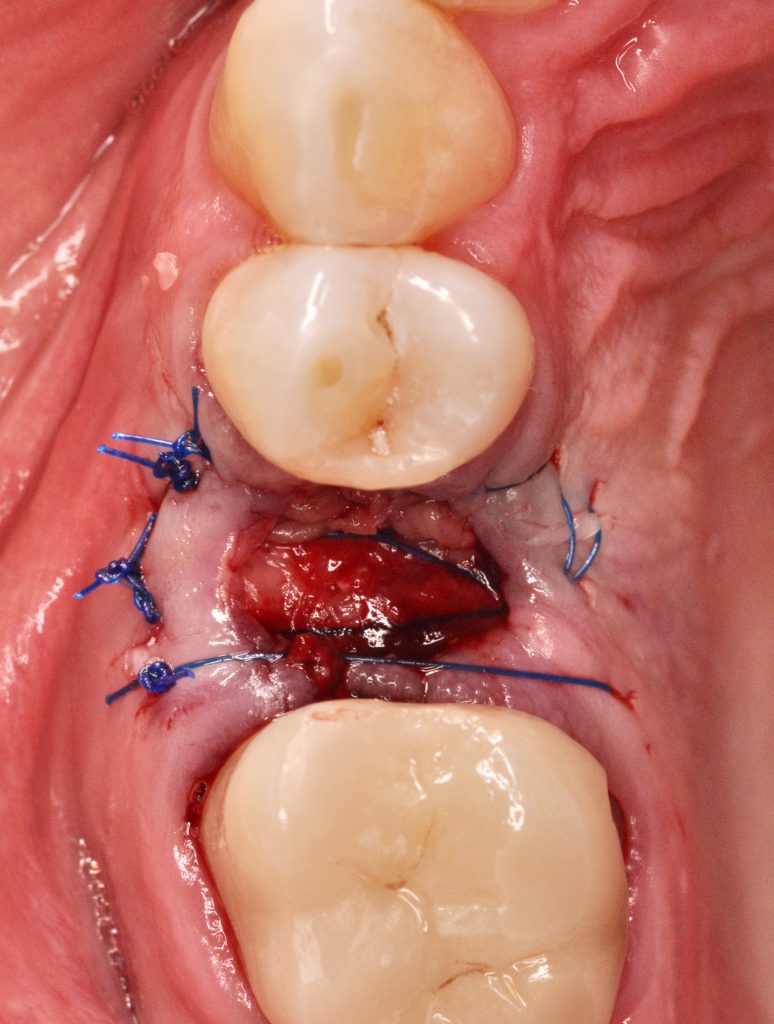
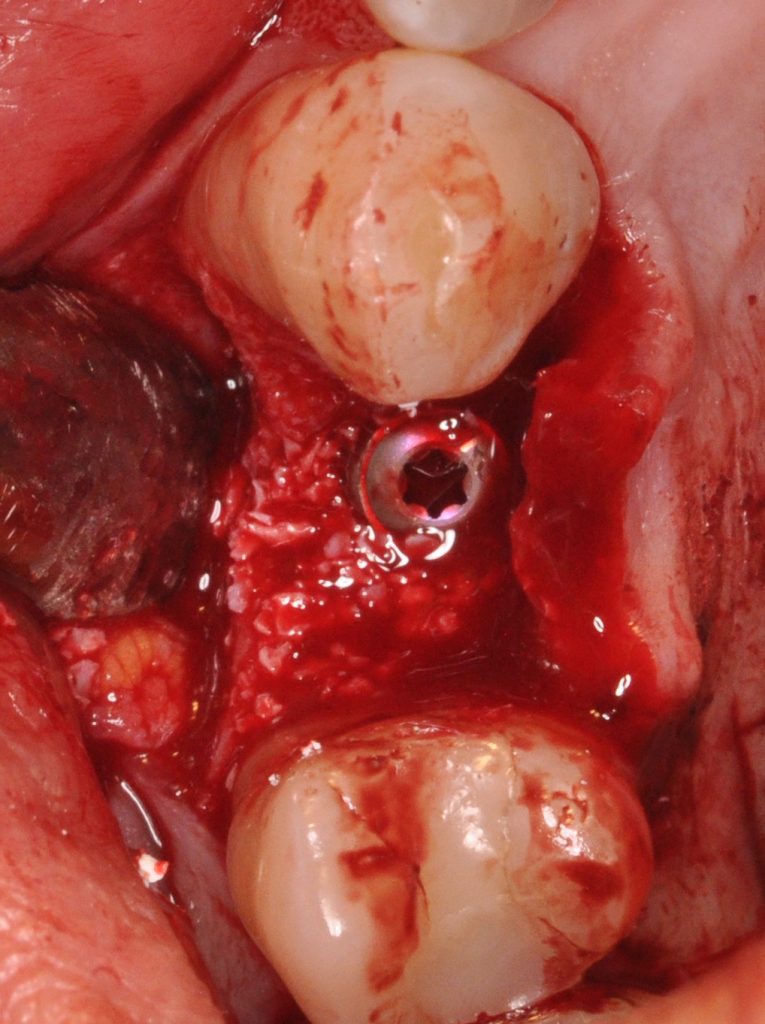
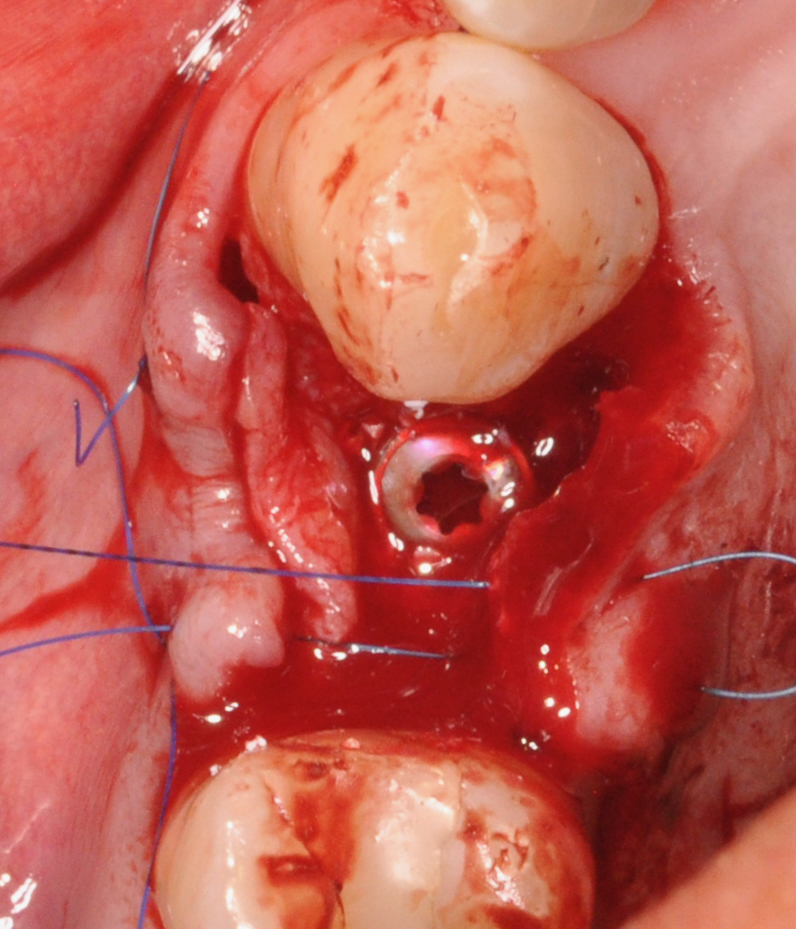
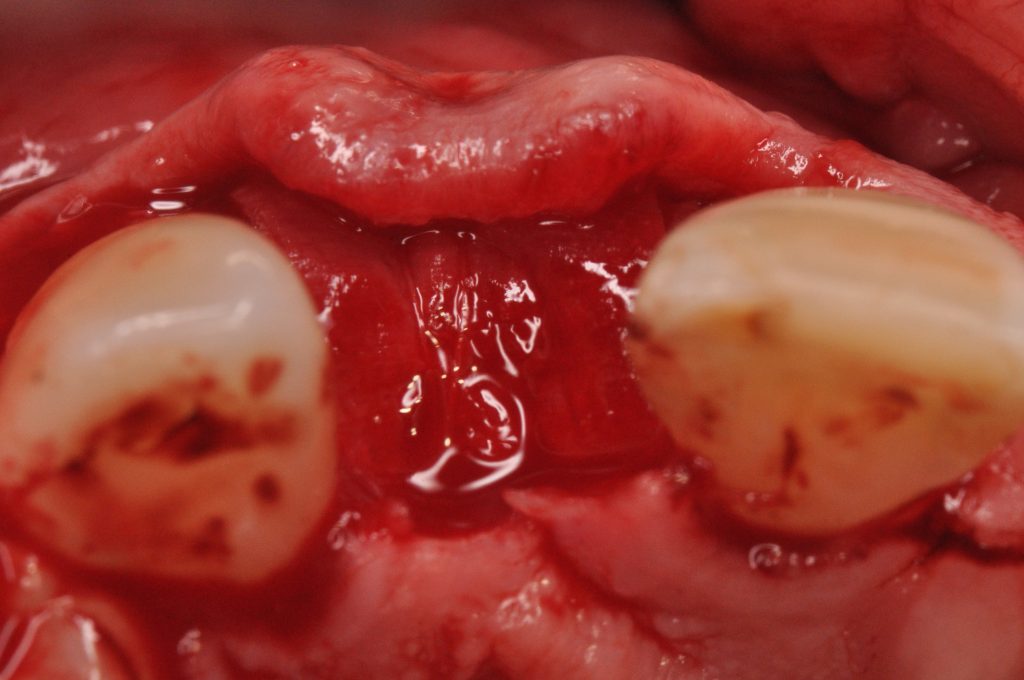
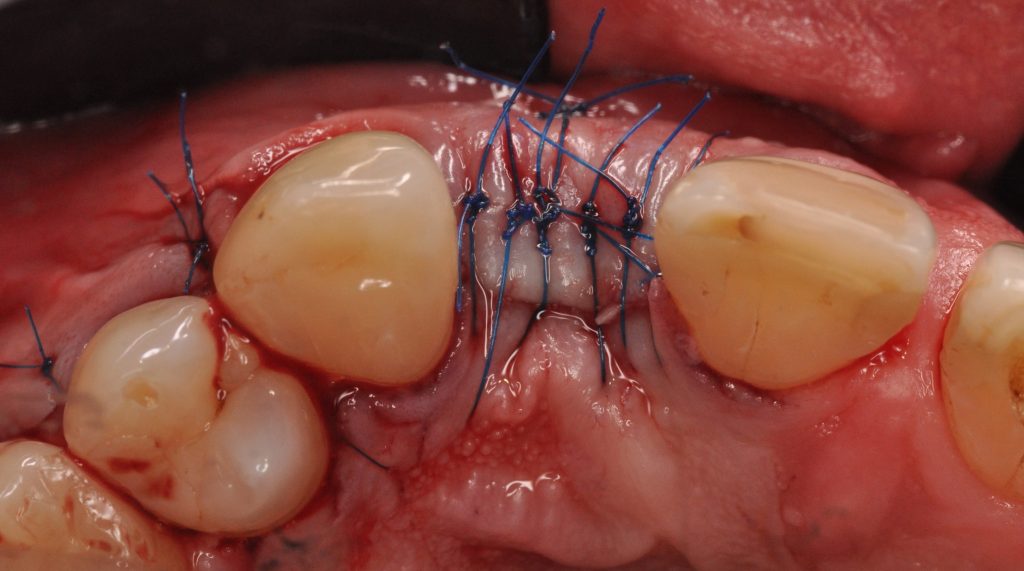
The clinical case (Fig. 4) demonstrates Type II implant placement with simultaneous contour augmentation and soft tissue modification using a connective tissue graft (CTG). Radiographic examination demonstrated insufficient residual bone height to the sinus floor for an immediate implant placement.


Type III – implant placement with partial bone healing
Although rarely used (1-3% cases), this approach provides the benefit of partial bone healing and prolonged healing allows resolution of extended periapical pathology (Buser et al. 2017, Morton et al. 2014). If it is anticipated that implant stability will not be achieved with a Type I or Type II approach, Type III implant placement may be considered. Another advantage is also complete healing of soft tissues at the time of implant placement.
The main disadvantage of this approach is that varying degrees of resorption are usually observed, limiting the available bone volume at time of implant placement (Schropp et al. 2003, Araujo et al. 2005).
The survival rates for Type II and III placement ranged between 96.3% and 100% using the conventional loading protocol with a follow-up of 2.5 to 8 years and success rate of 100% (Gallucci et al. 2018). Immediate (prosthesis delivery within 1 week) and early (between 1 week and 2 months) loading protocols were reported to be insufficiently documented (Gallucci et al. 2018).[TF1] Only one study demonstrated a positive outcome of Type II-III placement with early loading in a medium-term follow-up (Belser et al.2009) and no studies were identified to report on early placement with immediate loading (Gallucci et al. 2018).
Type IV – implant placement in a fully healed ridge
Late implant placement is not usually recommended due to the risk of extensive resorption of the ridge post-extraction, which is a major disadvantage (Morton et al. 2014). Schropp and his co-workers demonstrated that two-thirds of the bony reduction in the horizontal dimension happens in the first 3 months (Schropp et al. 2003). The expected average alveolar ridge reduction following spontaneous healing is 3.8 mm in width and around 1.24 – 1.67 mm in height (Tan et al. 2012). These findings correspond to around 29-63% of horizontal bone loss and 11-22% of vertical reduction. Therefore, if the implant placement is not indicated or possible within 2 months, alveolar ridge preservation is indicated according to the current literature (Avila-Ortiz et al. 2019).
Type IV case selection criteria:
- Young patients
Implant placement should be postponed until jaw growth has ceased because implants don’t follow the eruption of natural dentition. Therefore, implant placement in a growing jaw could result in occlusal and gingival discrepancies (Testori et al. 2018).
- Periodontally unstable patients requiring extensive treatment
Elimination of periodontal lesions, establishment of a high standard of infection control and regular maintenance care in periodontally compromised patients improve the long-term success of therapy (Roccuzzo et al. 2022).
- Anticipated delay in implant treatment
Alveolar ridge preservation might be considered if patients wish to delay implant placement to the unforeseeable future, due to personal circumstances or medical reasons, to reduce alveolar ridge resorption.
Survival rates reported for Type IV implant placement ranged between 97.7% to 98.3% with up to 2.5 years follow-up depending on the loading protocol (Gallucci et al. 2018). Type IV implant placement with early or conventional loading is a scientifically and clinically validated protocol, which yield higher success rates of 82.4-100% for early loading and of 88-100% for conventional loading compared to those for immediate loading (72.2-100%).
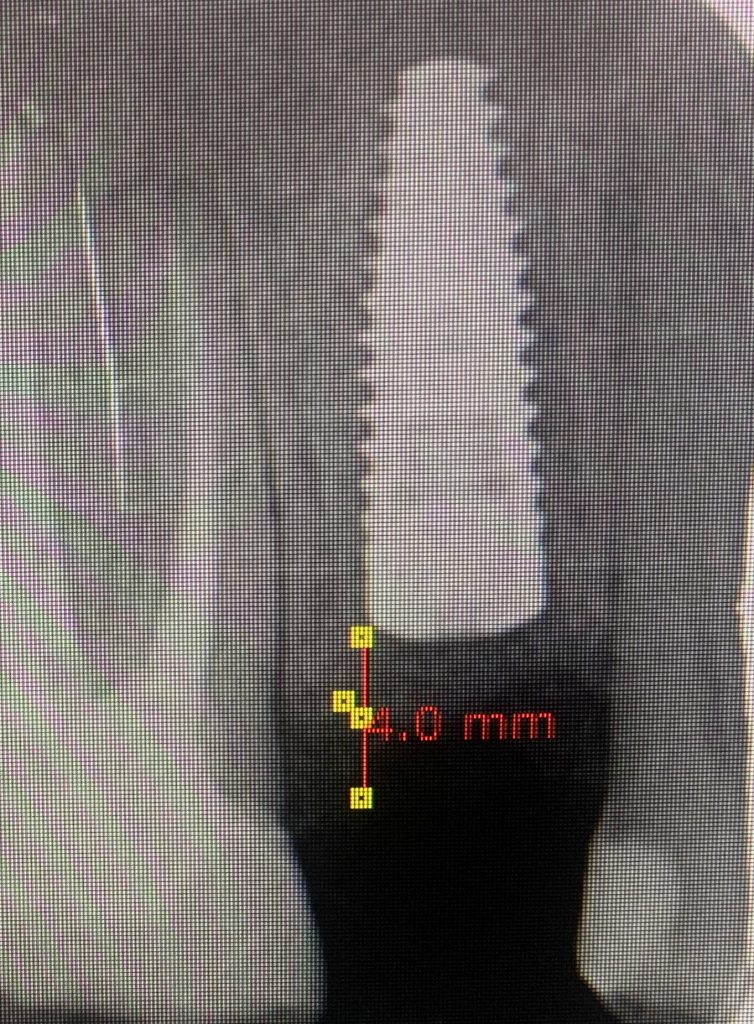
The clinical case in figure 5 illustrates Type IV implant placement. The patient lost the UR2 over 10 years ago. In the preoperative clinical and radiographic assessment, a buccal concavity due to horizontal bone loss can be seen.





Conclusions
Four different treatment options are available for clinicians today based on the timing of implant placement. Satisfactory results at post-extraction sites can be achieved with all types of implant placement, however, meticulous case selection is crucial. Immediate implant placement can be the treatment of choice in patients with ideal anatomical conditions (i.e. thick intact buccal bone) but it is technique-sensitive and requires an experienced team. Type II implant placement can be considered in sites with a thin or damaged facial wall. It allows soft tissue healing, however this approach frequently requires an open flap procedure and contour augmentation. Type III is rarely applied due to the associated bone resorption and is mostly used for sites with an extended periapical lesion. Type IV placement is usually reserved for situations of absolute necessity due to specific patient- or site-related reasons. If Type IV implant placement is anticipated during tooth extraction, alveolar ridge preservation is strongly recommended. Regardless of the approach, careful planning and case selection are key for long-term success.