Introduction
Modern implant rehabilitation has become a computer-driven process, where CBCT imaging, surgical planning and prosthetic design software all allow the implementation of a digital workflow (Lerner et al. 2021). This workflow does not only help the practitioner execute the planned implant easily , but also increases the predictability and clinical success of osseointegration. It also aid in immediate loading protocols along the biological developments of fusing implant surfaces to grafted bone and peri-implant supporting structures (Adell et al. 1981; Albrektsson et al. 1986).
Nevertheless, at the end of this digital process, all the intended prosthetic design elements cannot account for the occlusal loads that occur during function on a newly installed, rigid, immobile, and unforgiving implant-supported prosthesis. Complication rates in implant prosthodontics exceed those of traditional tooth-supported restorations (Sailer et al. 2018), which necessitates following an occlusal scheme to combat destructive occlusal forces that often damage implant restorations.
Generally, applied occlusal forces are controlled through pulpal and periodontal ligament (PDL) mechanoreception and proprioception, and are somewhat neutralized by the periodontal structures (Madani et al. 2017; Dario 1995). Unlike natural teeth, the absorption of masticatory forces through osseoperception is reduced with implant-supported prostheses, due to the absence of a periodontal ligament (Madani et al. 2017; Dario 1995). While teeth can move apically within the socket about 50 to 100 µm, apical implant movement is limited to only 3 to 5 µm (Roque 2017). Hence, the occlusal material on an implant-supported crown bears the entire applied occlusal force, and can affect the structural integrity of both the abutment and implant body, as well.
Typically, an implant-supported prosthesis is delivered with an implant-protective occlusal scheme (IPO), developed with shim stock and very thin articulating paper. The implant occlusal surface is theoretically sub-occluded from the opposing occlusal surface by 25 µm, to prevent occlusal force overload during a normal strength mandibular closure into maximum intercuspation (Bozhkova 2016; Chaithanya et al. 2019; Luo et al. 2020).
Despite the widespread belief that an IPO provides adequate control over occlusal forces, occlusion related mechanical complications in implant-supported prosthesis remain common (Elemek et al. 2020; Papaspyridakos et al. 2020; Lerner et al. 2020; Sailer et al. 2018; Shen et al. 2018; Pjetursson et al. 2018; Drago 2016; Wittneben et al. 2014; Fischer et al. 2013; Pjetursson et al. 2012; Bozini et al. 2011; Jemt 2006), as long term survival studies indicate that mechanical complication rates in implant -supported prosthesis supersede those of natural teeth. (Elemek et al. 2020; Papaspyridakos et al. 2020; Lerner et al. 2020; Sailer et al. 2018; Shen et al. 2018; Pjetursson et al. 2018; Drago 2016; Wittneben et al. 2014; Fischer et al. 2013; Pjetursson et al. 2012; Bozini et al. 2011; Jemt 2006). Therefore, compared to tooth-supported prosthesis, implant rehabilitations require meticulously adapted occlusion because the implant-supported prosthesis lacks resiliency, elasticity, and forgiveness (Lerner 2020).
There are many known types of implant complications that result from increased occlusal overload (Adell et al. 1981; Albrektsson et al. 1986; Esposito et al. 1998; Balshi 1996), which can elevate peri-implant crevicular fluid levels, compromising peri-implant tissue health while leading to possible bone loss. The frequent mechanical complications include:
- Screw loosening
- Screw fracture
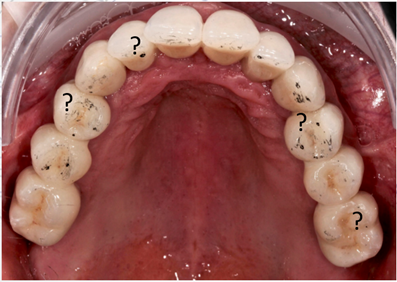
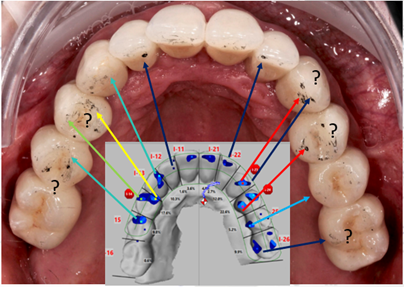
- Occlusal material failure (Fig. 1)
- Prosthesis substructure fracture (Fig. 2)
- Abutment fracture
- Peri-implant bone loss
- Difficult patient occlusal acceptance of the prosthetic occlusal contacts
- Occasionally, in severe cases, an implant body itself can fracture (Fig. 3)


A major contributor to a common occlusion-related mechanical complications is the clinical use of analog traditional occlusal indicators, such as articulating paper/foil/strips/horeshoes, shim stock “hold”, occlusal wax imprints, silicone imprints, and articulated casts (both stone and virtual) (Qadeer & Sarinnaphakorn 2020) . Studies have shown that articulating paper specifically, is incapable of measuring occlusal forces (Balshi 1996; Qadeer et al. 2012; Saad et al. 2008; Carey et al. 2007; Bozhkova 2020), leaving the clinician to adjust occlusion by “subjectively interpreting” the articulating paper marks. Unfortunately, this contact selection method is highly prone to error and fails to reliably control force levels (Basson et al. 2020; Sutter 2017; Kerstein & Radke 2013). Studies have shown that by relying on the visual detection of articulating paper marks, dentists select incorrect contacts 87-95% of the time (Basson et al. 2020; Sutter 2017; Kerstein & Radke 2013).
Utilizing digital occlusal indicators in implant-supported prosthesis
Adding computerized occlusal analysis (T-Scan 10 Novus, Tekscan, Inc., Norwood, MA, USA) when adjusting occlusion in cases definitive implant restorations or in cases of immediate loading, helps ensure a predictable targeting of problematic occlusal loads when adjusting occlusion (Lerner 2020). These problematic occlusal loads include premature contacts and excessive contact forces that can de-stabilize an implant restoration. Several digital occlusal tools exist that can aid in occlusal adjustments like Accura (Dmetec Co, Ltd, Seoul, South Korea) , Occlusense (Gmbh Bausch, Germany), and T-Scan , the latter being the most clinically tested device (Sutter 2019).
Many studies have been conducted on T-Scan (Qadeer et al. 2020) that have verified its accuracy in detecting occlusal problems (Koos et al. 2010), its force reproducibility (Harty et al. 2006; Koos et al. 2010; da Silva Martins et al. 2014; Kerstein & Radke, 2022), its time quantification (Koos et al. 2012), and its clinical effectiveness in many areas of patient occlusal care (Qadeer et. al. 2020). Many digital occlusion T-Scan protocols exist in Prosthodontics, Dental Implants, the Digital Workflow, TMD, Posturology, Orthodontics, Periodontics, Occlusal Diagnosis, Aesthetic Dentistry, Tooth Hypersensitivity, Mandibular Orthosis, Occlusal Adjustments, and Patient Education (Kerstein 2020).
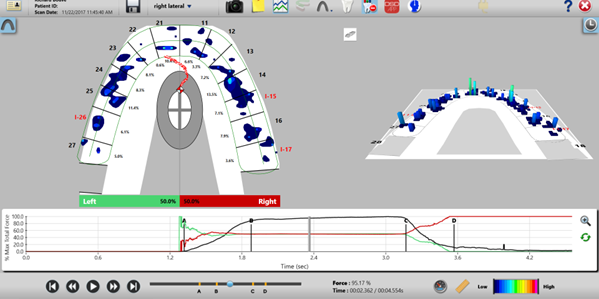
Digital occlusal indicators like T-Scan dynamically records and displays the occlusion time (OT), disclusion time (DT), the relative force % distribution, the intensity of 256 relative occlusal forces and their duration, and the timing order of all occlusal contacts, as they each occur inter-occlusally during functional mandibular movements (Kerstein 2020).Such indicators bring objective data to the process of occlusally adjusting an implant restoration, whether the case is full-arch implant supported prosthesis, a removable overdenture, a segmental implant restoration, or a single unit (Aradya et al. 2022; Mangano et al. 2021; Kuder et al. 2017; Ma et al. 2016; Cotruţă et al. 2015). Regardless of the clinician’s desired occlusal scheme (Implant Protected; Anterior Guided, or Balanced), the digital indicator can guide the contacts selected for corrective adjustment where the case installation outcomes are quantifiably improved compared to those obtained with subjectively interpreted, non-digital occlusal indicators (Fig. 5) (Qadeer et al. 2020; Andrus et al. 2019).
How digital occlusal indicators work?
Functional occlusal data sets are recorded intraorally with an ultra-thin, Mylar-encased 100-um thick electronic printed circuit sensor, shaped in the form of a dental arch (Novus HD sensor, Tekscan Inc. S. Norwood, MA, USA) (Figs 6 – 7) that is placed between the patient’s teeth, as they occlude into maximum intercuspation or make lateral excursive movements. The HD sensor sits in the Novus recording handpiece that connects to a computer workstation via a USB interface, and transmits a stream of digital occlusal contact information to the software for presentation to the dentist on the T-Scan 10 desktop.
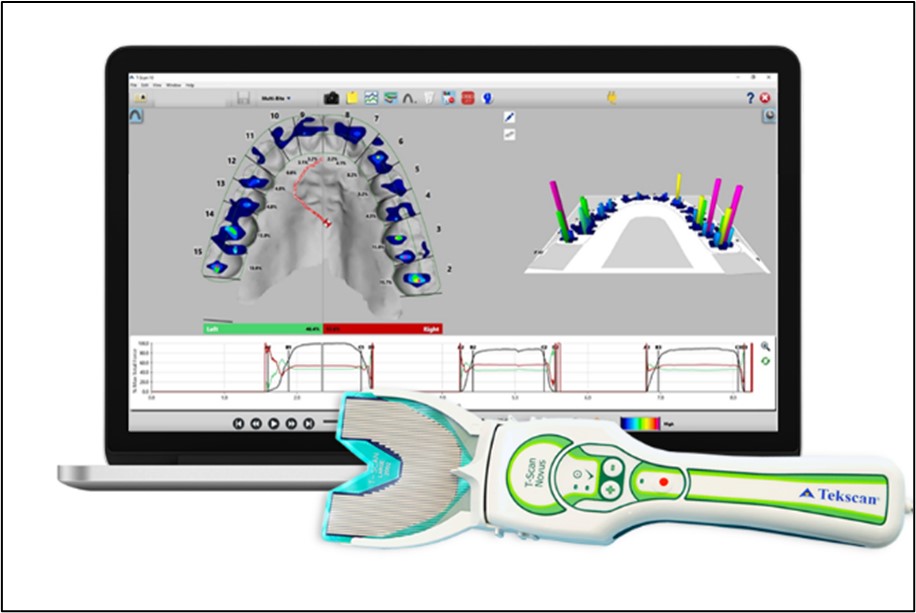

When a patient occludes upon an HD sensor, the opposing teeth make approximating contact that compresses together the upper and lower sensor surfaces, which results in a change in the electrical resistance in each of the compressed 1-mm2 force measurers (the sensors contain between 1500-2200 force measurers). These resistance changes are then measured by the T-Scan’s hardware electronics as a change in digital output voltage (DO). When the contact force applied is higher, it produces larger resistance changes, and lower occlusal contact force produces lesser resistance changes. A map in the T-Scan 10 software receives a stream of changing sensel digital output voltage values (from the recording handpiece) and organizes them in the same orientation the sensels have within the sensor matrix. These contact-induced voltage changes are presented to the implantologist in a multi-colored, 2- and 3-dimensional dynamic video playback graphical display (Fig. 8a) (Kerstein 2020).
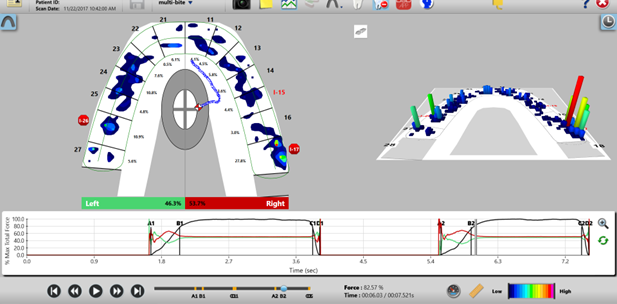
The digital indicator system detects whether an occlusal force on one set of contacting opposing teeth or implants is greater, equal to, or less than the occlusal forces occurring on other contacting teeth throughout the dental arches. This aids the implantologist in diagnosing excessively high occlusal force concentrations, while simultaneously diagnosing where there is little, moderate, low, or no occlusal force present in other areas of the same occlusion (Kerstein 2020). Determining where excessive relative forces are concentrated on implant prostheses can accurately diagnose their location for precisely targeted computer-guided time-based and force-based occlusal adjustments.
An example of this computer-guided closure into MIP force control that develops improved occlusal force balance in a patient with 3 isolated single implants crowns can be seen in Figures 8a and b. The maxillary 2nd molar implant #I-17 is holding excessive and intense contact forces (32.7% of the entire occlusion), which set off an overloaded implant warning (red stop sign), while also causing the patient significant bite discomfort since this crown was initially placed 2 years prior. Excess occlusal force was also detected on implant #I-26, setting off another overloaded implant warning. By using the T-Scan technology to target these 2 overloaded implant crowns with computer-guided occlusal adjustments, widespread, low force occlusal balance was established that did not raise any implant warnings (Fig. 8b). Then, following closure and balance corrections, excursive lateral and protrusive movements were optimized.
Limitations of digital occlusal indicators
Digital occlusal indicators can increase chair time when performing computer-guided occlusal treatment, because it requires the clinician to meet high-telorance occlusal metrics to measurably establish a low-force and balanced outcome (Fig. 8b). Also, digital sensors do not mark the occlusal contacts which means that an articulating paper is still needed, but only to “mark” contacts. Its appearance is not “judged subjectively” for perceived force content because the digital indicator data targets the specific contacts for adjustment. Another limitation is that these indicators do not measure absolute force in engineering units (Kerstein 2020). Finally, there is a definite learning curve required of clinicians (involving didactic amd clinical training), to develop the chairside skills required for optimal computer-guided diagnostic and treatment effectiveness (Afrashtehfar & Qadeer, 2016).
Advantages of digital occlusal indicators
a. Clinician related advantages
There are many clinical advantages for the clinician when using this technolgy compared to using traditional occlusal indicators (Qadeer, 2020) including:
- Quantifiable time-sequencing and force-mapping guides diagnosis and treatment
- Precise, targeted occlusal adjustments made based on objective, metric data
- Increased accuracy and clinical results when performing occlusal adjustments
- Cost savings related to fewer material and prosthesis failures
b. Patient related advantages
There are also a number of patient advantages to T-Scan, as well (Qadeer 2020) that also include:
- A visual aid that offers comprehensive insight and understanding to the patient’s occlusal status
- Minimally invasive treatment is rendered because occlusal measurements replace the compromised subjective paper mark method
- Improved prosthesis occlusal outcomes with less overload sequelae
- Reduced number of follow-up adjustment appointments needed for occlusal adaptation
Conclusion
The deleterious consequences of choosing the wrong contact to adjust occlusion are potentially many, because undetected high force contacts are left in place and eventually cause cyclic overload of an implant prosthesis, while healthy undetected low-force contacts may be inadvertently adjusted away. Contact selection subjectivity certainly plays a definitive role in the high rates of occlusal and implant material complications that occur with dental implant restorations. This is the main reason installing implant prostheses with the objective force and timing metrics of the digital occlusal indicator technology like T-Scan helps aid in both long-term implant component material survival and peri-implant biomechanical health.
Disclosure
Dr. Robert Kerstein is a Clinical Consultant for Tekscan Inc., Norwood MA, USA. He receives no compensation for sales of any Tekscan products