Soft tissue management is a crucial aspect of any bone augmentation procedure, since wound dehiscence is detrimental to new bone formation. Looking at the data in the literature, this is not so rare, indeed an incidence of dehiscence around 12-20% has been recently reported for vertical bone augmentation with guided bone regeneration (GBR) or autogenous bone block (ABB) (Urban et al. 2019).
It has been reported that suture tension is the most important factor in determining primary wound healing. A 5g tension seems to be the limit, below this tension-value wound healing will be uneventful, while over this tension-value the risk of complications grows quite rapidly (Burkhardt & Lang 2010). It means that, in the case of a correctly passivated flap, the tension at suture level will be lower than 5g, while in an incorrectly passivated flap the suture will hold a greater tension force. What is curious is that in every study theoretically correct soft tissue management is reported and described but, nevertheless, wound dehiscences are reported as well. Why does this happen? Is there something we are missing?
Probably, yes! Usually in the literature, a passive flap is one that reaches a specific target point after a periosteum releasing incision, for example the occlusal plane of neighboring teeth. But this evaluation considers the length of the flap, not the force applied to the surgical tweezers to bring and maintain the flap to that target point. This means that an elongated flap is not necessarily a passive flap. This mismatch between length evaluation and wound tension is probably at the base of the high risk of complications in wound healing.
How can we avoid complications or at least limit them to a very few cases? How can we control wound tension? A strategy is needed that is based on three aspects: (i) flap design; (ii) flap elongation and (iii) wound sealing. All three points work in the same direction towards obtaining low-level tension wound closure.
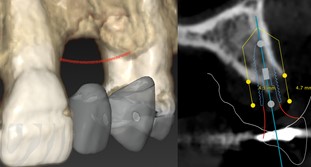
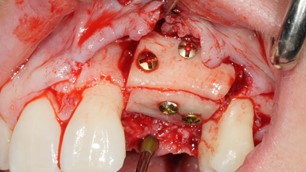
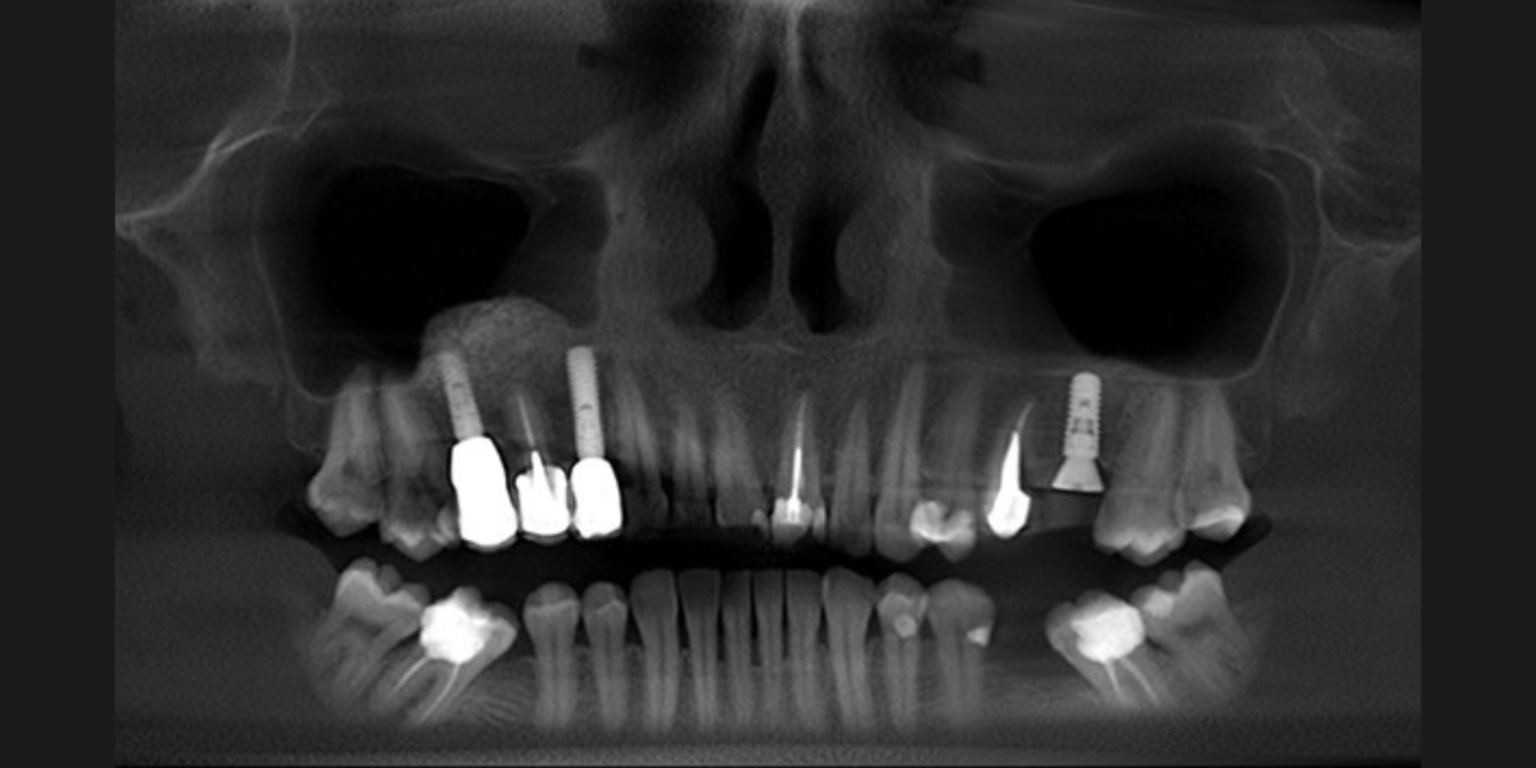
- Flap design is crucial since a mid-crest incision may not be the perfect choice in any case. We should think about the flap position at the end of the surgery before performing the incision. Indeed, wound closure should be based on horizontal mattress sutures, which evert and couple the internal face of both flaps. To perform this correctly, the suture layer flaps should be longer than the achieved bone level (residual bone plus bone graft) by at least 4 mm. In the lower jaw, where both flaps can be elongated by specific management, the incision can be performed in the middle of the residual crest (Fig. 1). On the opposite side, in the upper jaw the palatal flap cannot be improved in terms of length because of its histological nature that is based on dense connective tissue. This means that the palatal flap may not be long enough to be everted and coupled with the vestibular flap, particularly in the presence of a vertical defect. A vestibular shifted incision may overcome this problem by increasing the length of the palatal flap at the beginning of the surgery. Considering the palatal margin of the residual crest as the palatal flap base, the incision should be situated 4 mm buccally in the case of a horizontal defect, while 4 mm plus the vertical defect dimension in the case of a vertical deficiency (Fig. 2). In the latter scenario, the incision is progressively shifted to the buccal side based on the defect anatomy (De Stavola et al 2021). In this way a free area of 4 mm will be available for the correct horizontal mattress suture application.
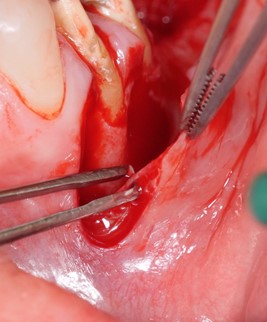
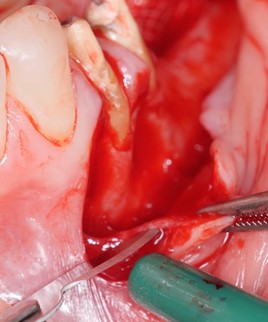
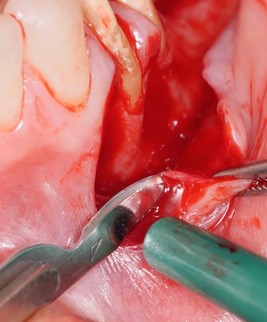
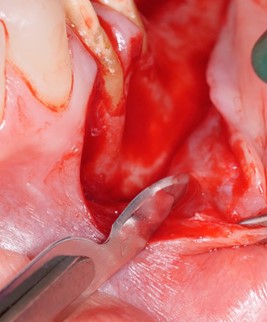
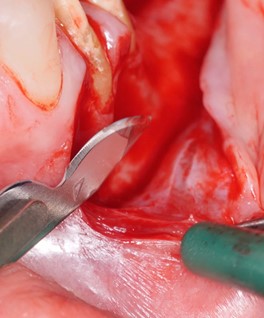
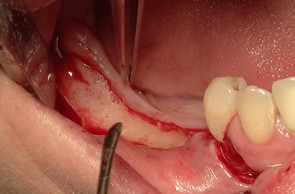
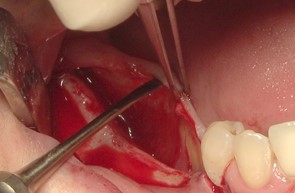
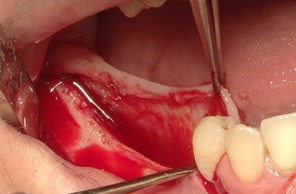
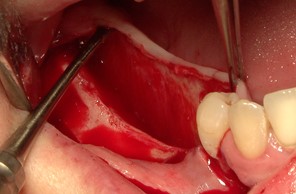
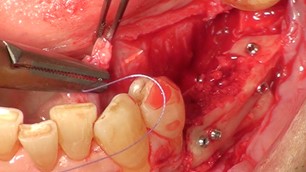
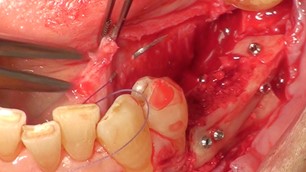
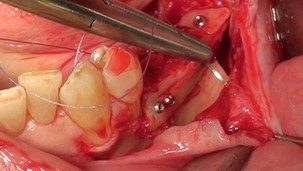
- Flap elongation is another important step for wound-tension control. Vestibular flaps (maxilla and mandible) are managed firstly by interrupting the periosteum and secondly by separating the flap tissue from the elastic and muscle fibers. The starting point for the periosteum incision is the fornix base and not the muco-gingival junction, but below. Working at this level, the flap thickness is not affected and the flap can be bisected from the deeper muscle fibers. In the first step, the blade will involve just the periosteum layer, which is a dense tissue of approximately 1-mm thickness (Fig. 3). In the second step of the flap elongation, the blade will work parallel to the flap surface starting from the coronal rim of the interrupted periosteum. The lingual flap should be managed differently due to its anatomical characteristics. Three areas need to be recognized by the surgeon: a) the distal area behind the retromolar path, b) the mylohyoid muscle in the second and third molar area, and c) the periosteum zone in the first and premolar area as well as in the frontal zone. The steps which surgeons should follow are these (Fig. 4): tunneling in the distal area behind the retromolar path, stretching the flap in the coronal direction in the muscle area, and interrupting the periosteum with a dissector in the periosteum area (Tinti & Parma-Benfenati 1998).
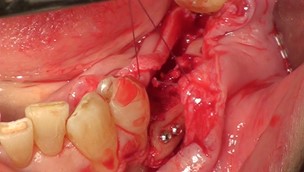
- Finally, wound closure through suture application, where the role of the suture is to seal the wound and not to hold the flap coronally. To obtain this low-tension wound closure, a breaking force suture should be applied involving just the coronal periosteum layer of both flaps, in the lower jaw, and only the vestibular coronal periosteum in the upper jaw (Fig. 5). These sutures will allow marginal flap tension to be released without impacting vascular flap support. Indeed, a reduction of almost 90% of the residual flap tension in expected (De Stavola & Tunkel 2014). Once the flaps are retained in the end-surgery position through the breaking force suture, the horizontal mattress sutures can be applied to seal the wound by coupling the inner faces of both flaps. Marginal adaptation of the wound will be performed by a single simple stitch line. Schematically, breaking force sutures are applied 6-7 mm apically from the flap rims, at 4 mm horizontal mattress sutures seal the wound at depth and single stitches adapt the wound margin at 2 mm from the flap rims.
In the majority of cases, the protocol presented here will allow optimal control over the wound tension, with a positive prospect of primary wound healing. Different approaches in this particular clinical scenario may be applied by other forms of flap management such as the tunnel flap, where no crestal incision over the grafted area is performed.
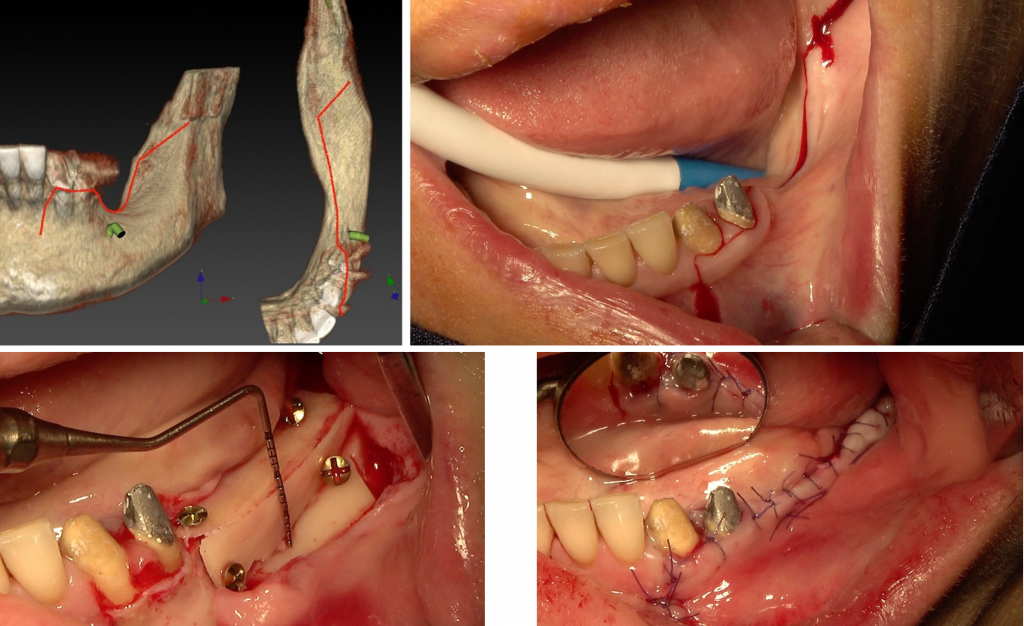
Fig. 1: In the lower jaw, an incision in the middle of the residual crest is optimal since both flaps can be elongated coronally. Note the distal releasing incision over the external oblique ridge in the direction of the ramus to avoid any damage to the lingual nerve and allow a perfect view and access to the possible donor site area. In the mesial area an incision in the buccal third of the anatomical papilla is performed to keep the papilla intact.
Fig. 2: Vertical defect in the maxilla, with a planned bone augmentation close to 5 mm. The palatal flap should be long enough to compensate the vertical graft (5 mm) and to allow a correct wound seal (4 mm). The necessary length of the palatal flap is 9 mm, starting from the palatal base of the defect, in the deepest defect area, 9 mm are evaluated with a periodontal probe. The crestal incision is shifted to reach that point. While closed to the mesial and distal bony peaks the incision line runs along the vestibular third of the crest. The blade should be 90° to the bone to avoid a beveled incision. Once the palatal flap is elevated, the flap length will be 9 mm. Once the bone graft has been placed, the flap will cover the graft of 4 mm to provide an adequate seal to the wound.
Fig. 3: The vestibular flap is elongated by interrupting the periosteum layer, which is a relatively thin layer compared to the overall thickness of the flap. The starting point is the base of the flap at the fornix bottom. The blade will stay at a superficial level to reduce the vascular damage. A safe distance from the mental foramina of at least 6 mm should be considered. A flap dissection is then performed to separate the flap from the deeper muscle fibers.
Fig. 4: The lingual flap is elongated without the use of a blade. Distal to the retromolar area, a tunnel is performed full thickness; in the molar area the flap is stretched coronally; in the premolar area the elevator tip works at 90° against the flap and is moved mesially and distally until the thin periosteum is interrupted.
Fig. 5: Before wound sealing is performed by applying horizontal mattress sutures and single stitches, one or two breaking force sutures are placed. The suture involves just the inner periosteum face of both flaps and is placed at least 6 mm from the flap rim. The flap vascular support is not affected. Both flaps move coronally towards each other stabilize in a coronal position. The horizontal mattress sutures will work to seal the wound only and not to hold the flaps in the coronal position.
Related article:
Related content: