Welcome to Singapore
We have enjoyed an amazing 3-day experience in the lion city. 3 days of lectures, discussion and learning, focused on evidence-based science and patient-centered care.
If you missed it, you can still get a personal flavor from the participants on this page where we posted live updates every day.
Digital Workflows
Gabriel Magrin reporting
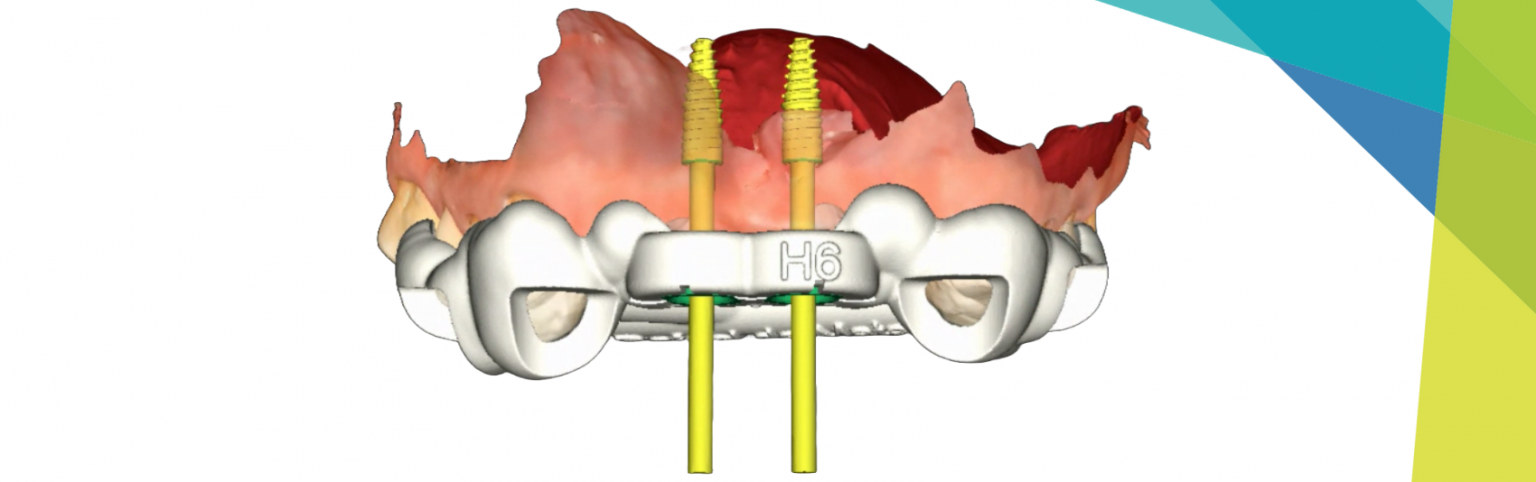
In daily clinical practice, several critical considerations emerge, particularly in digital dentistry applications. Cone-beam computed tomography (CBCT) acquisition and intra-oral scanning (IOS) encounter challenges such as patient movement, metallic artifacts, and mobile soft tissues, underscoring the importance of accurate data acquisition and segmentation. Understanding the intricacies of CBCT acquisition challenges such as patient movement and metallic artifacts may lead to improved strategies for minimizing errors and enhancing data accuracy. Implant placement precision through computer-assisted implant surgery (CAIS) demands meticulous planning and control over implant position. Additionally, material selection, particularly for full-arch restorations, presents challenges, with zirconia emerging as a gold standard but requiring further development to optimize esthetics and minimize complications. Moreover, human factors, including lack of planning and judgment errors, pose significant risks, emphasizing the dentist’s pivotal role in treatment outcomes. Integration of digital protocols should prioritize predictability and enhance communication with patients and peers, leveraging tools like the ITI SAC assessment and 3E check for comprehensive patient evaluation and treatment planning.
Things I can apply immediately
Several actionable insights emerge from the integration of digital dentistry technologies into daily clinical practice. Intra-oral scanning (IOS) offers advantages like eliminating traditional impressions but requires careful attention to mobile soft tissues and the resorbed edentulous mandible. Therefore, incorporating reverse scanning techniques for edentulous mandibles can significantly enhance prosthesis fit and can ease the scanning procedure.
Computer-assisted implant surgery (CAIS), whether static or dynamic, demands thorough training but promises improved prosthetic outcomes and patient safety. Ensuring low tolerance between drills and surgical guides during CAIS is of ultimate importance to achieve a precise implant placement. Stop sleeves and other methods should be used to maintain the control over the vertical position of implants and to avoid mismatches between the planned and performed position of implants. Moreover, leveraging digital planning tools, such as a combination of implant placement and teeth-positioning digital files, and assessment protocols such as the ITI SAC assessment and 3E-check enhance treatment predictability and build trust between dentists and patients. Integrating these strategies into daily clinical practice can optimize treatment outcomes and patient satisfaction.
Ideas I would like to find out more about
I would like to delve deeper into intra-oral scanning (IOS) techniques, particularly in addressing challenges like the edentulous mandible, where the mobile soft tissues and the lack of solid landmarks can pose difficulties during image acquisition. Valuable insights into achieving perfectly fitting prostheses were provided during the session, especially in complex cases such as full-arch rehabilitations. As an alternative to edentulous mandible traditional scanning, we can implement a reverse scan body concept. It is an extra-oral technology, not affected by intra-oral factors. The prosthesis fit with reverse scanning can be 100%, while the conventional IOS is about one third.
Additionally, investigating the potential of artificial intelligence (AI) in aiding computer-assisted implant surgery (CAIS) could provide valuable insights for improving surgical precision and patient outcomes. The discussion around CAIS highlighted the potential of dynamic CAIS with AI integration to improve surgical precision and patient safety. Exploring this technology further could revolutionize implant dentistry by providing real-time visualization and guidance during surgery.
How well did the clinical and patient videos work together?
The integration of clinical and patient videos was effective in providing a good understanding of digital workflows for implant dentistry. The clinical case video provided a detailed overview of the treatment process, including challenges faced and strategies employed, such as the construction of guides for precise implant placement and the use of check splints to ensure passive fit of the prosthesis. This visual demonstration offered valuable insights into the practical application of digital techniques in a real-life scenario, aiding in knowledge acquisition for dental professionals. Additionally, the patient report video offered firsthand accounts of the treatment experience, providing valuable perspectives on aspects such as pain management, procedural complexity, and overall satisfaction. The combination of these videos facilitated a comprehensive understanding of digital dentistry practices, emphasizing the importance of meticulous planning, precise execution, and patient-centered care.
3 things I am taking away from the session and why it is important to me
- The emphasis on accurate data acquisition and segmentation during CBCT acquisition and intra-oral scanning is crucial. These steps lay the foundation for precise treatment planning and execution, minimizing errors and enhancing clinical outcomes.
- Computer-assisted implant surgery is an important factor towardsreducing errors and improving the success of implant treatment in current dental practice.
- It is essential to recognize potential mistakes during the whole process and leverage digital protocols to enhance communication, decision-making, and implant treatment in order to deliver high-quality treatment and build trust with patients. These insights underscore the continuous learning and adaptation required to stay at the forefront of digital dentistry and provide optimal care to patients.
Management of Peri-implantitis
Teresa Chanting Sun reporting
The speakers in my session made it clear that as clinicians we should not look at peri-implantitis as a complication but as a disease. And in that context, we need to explore and identify its etiology and then control the build-up of biofilm. As always, the proper diagnosis and treatment plan are the first step, where the prosthesis design plays an important role, before deciding on which non-surgical and/or surgical procedures to follow.
If there was one key message it was that, in the long-term, prevention is always better than cure as peri-implantitis treatments are not always predictable.
Looking to the future, ideas were floated for a transmucosal design of implant that would promote soft-tissue attachment rather than simply having a sealing effect as well as bacteriostatic surfaces to the implants.
3 things I’m taking away from this session
- When treating patients, start conservatively with non-surgical treatment and then escalate to surgical treatment if necessary but without forgetting that even surgery does not always have a predictable outcome. Make sure to carry out a comprehensive risk assessment.
- Never forget that patients are mostly not really aware of the implications of peri-implant disease on their health and life. The patient videos underlined how important patient education is to get them on board with realistic expectations and a full understanding of the treatment process. They also need to be instructed on how to maintain their post-treatment oral health optimally.
- Overall, it’s all about prevention, prevention, prevention!
Immediacy
Yukihiro Takeda reporting
Immediacy was the main focus here with the overall aim of improving quality of life for patients by shortening treatment time with the predictable results. The speakers underlined that careful selection of the right treatment approach for each case is imperative. It’s all about good preparation and planning that starts with the implant supracrestal complex with the abutment and crown.
Things I can apply immediately
Using the esthetic risk (ERA) and SAC assessments to ensure that my patients are getting the right treatment.
Collecting all the necessary digital data right from the start using the intraoral scanner and CBCT to build up a comprehensive picture of the situation
The patient videos
I found the patient videos very helpful as clincians (me, included) have a tendency to look at diseases and symptoms without necessarily always seeing the patient behind them. The videos were a reminder that we need to educate patients to get their buy-in and help them set realistic expectations.
3 things I’m taking away from the session
- The battle over placement concepts is over and we now have predictable treatment protocols that simply need to be applied correctly.
- Having a sound understanding of our skills, knowledge and limitations is necessary so we can deliver the best possible treatment
- When planning start with the crown and abutment before moving on to the implant design and positioning. Irena Sailer says: Bone sets the tone, tissue is the issue, but pros is the boss!
GBR/Bone Augmentation
Rafael Lazarin reporting
In terms of bone regeneration, the speakers in the first session all agreed that for the long-term success of any type of rehabilitation two fundamental factors are crucial: an understanding of the biology of each bone defect along with the associated biological requirements as well as selection of the appropriate case. They reiterated that not all problems can be resolved by extensive grafting or esthetically pleasing surgeries but that complications can and do arise.
The role of medication was discussed, specifically of antibiotics and regenerative procedures. Patients on antiresorptives were flagged as at high risk for complications along with smokers. For these groups, based on site/patient-specific situations, alternative treatment should be considered with narrow diameter, zygomatic, subperiosteal implants and short implants as good alternatives to avoid GBR procedures or minimize their invasiveness.
I found that the patient videos added a new dimension showing how the lives of patients change following treatment. This triggered discussion among the panel where different techniques and approaches were discussed, but similar opinions on the principles to be followed were put forward.
Ideas I would like to find out more about
While listening to this session’s speakers, several things occurred to me. I would like to know more about the association between bone defect morphology and implant installation moments, see direct comparisons between GBR procedures and treatment alternatives, and generally get more detailson complications (and how to resolve them, of course). And lastly, further details on future trends and the real impact of antibiotics on regenerative procedures would also be great.
3 things I’m taking away from the session:
You need to have knowledge and understanding of biology in order to perform proper case selection, which is the first key point to achieving success.
Be cautious with the selection of clindamycin in regenerative procedures, preferably opting for other alternatives for patients who are allergic to penicillin. Since we must adopt a rational approach to the use of antibiotics, knowing which ones to use to obtain the real benefit of the medication is essential for case management/resolution.
Be aware of your limitations. Refer, seek assistance, or explore alternative treatments when large regenerative procedures are necessary.
Soft Tissue Management
Lucrezia Paternò Holtzman reporting
This session focused on the diagnosis and etiology of peri-implant soft tissue dehiscence (PSTD) defects, as well as on the importance of soft tissue to both esthetics and function. The speakers asserted that, depending on the clinical scenario, both autologous grafts and soft tissue alternatives can be considered. And the final lecture gave us a peek into the future perspectives on the diagnostic techniques for soft tissue dehiscence defects along with possible new developments in the field of bioengineering.
There are some ideas from the session that I will be able to apply immediately. For example, the knowledge that soft tissue grafting around implants is crucial for good esthetics. And also, that the quality and quantity of soft tissue are paramount to maintain peri-implant health.
Ideas I would like to find out more about
During the afternoon a number of things came up about which I’d like to know more. For example, how ultrasonography can be used to diagnose PSTD and monitor the healing and perfusion of grafting procedures. And additionally, how to optimize soft tissue healing using bioengineering.
3 things I’m taking away from the session:
Correct implant positioning is of key importance to prevent PSTDs and esthetic deficiencies in the soft tissues
PSTDs have different prognosis and treatment approaches depending on the defect classification
Due to the high volume of incorrect implant positioning we are likely to encounter PSTDs more and more frequently in our clinics in the future. We should know about them and their treatment!
Day 3: The culmination of four years of hard work
Our last day in the lion city was filled with patient stories and impressive presentations all around peri-implantitis and digital workflows. But at least as much was going on in the social and exhibition area as it was time to say goodbye to old friends and new acquaintances. The announcement at the end of the day of the winners of the Young ITI World Series and Poster Presentations, the André Schroeder Research Prize and ITI Academy Video awards represented the red cherry on the top of a record-breaking 2024 edition of the ITI World Symposium. See you in 2027 in Milan, Italy!
Some more impressions
Out and about at the ITI World Symposium



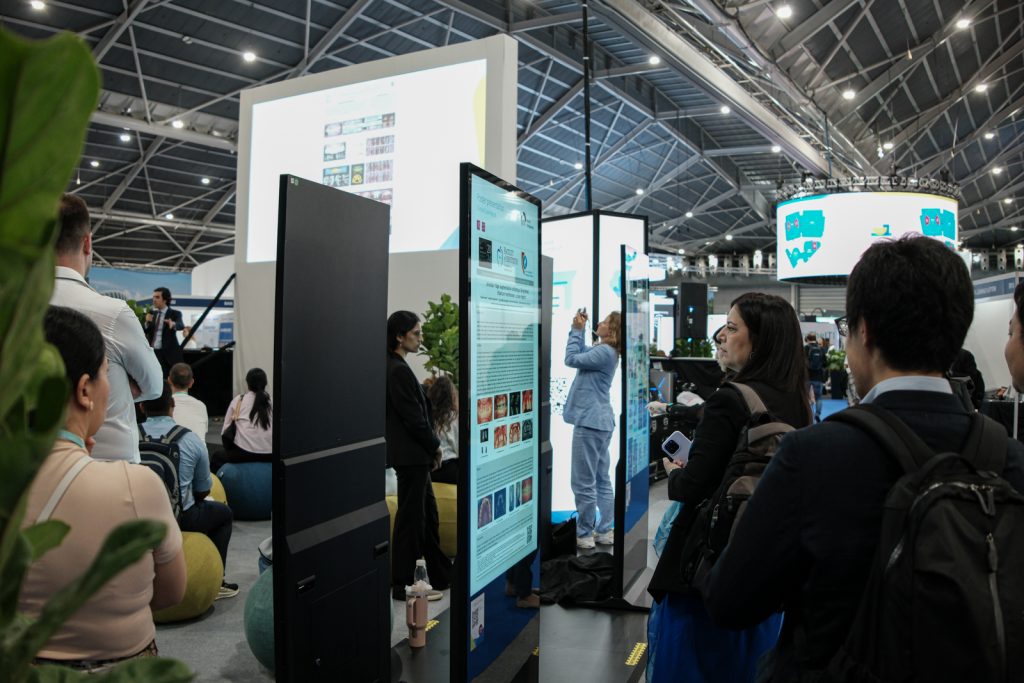






































Day 2: Backstage, on stage, at the heart of the action
Every face tells the same story – the ITI World Symposium is truly in full swing.
More impressions
Day 2 is on and we are in the zone!










Day 1 – Off to a breathtaking start
The 7-year wait since the last on-site ITI World Symposium has finally come to an end. The 2024 edition in Singapore kicked off today with an exciting opening ceremony including a vibrant dragon dance for the 5,700 delegates.
Couldn’t make it to the world’s largest implant dentistry event in 2024? Here is our video recap of the first day.
First impressions
Can’t wait, it’s gonna be great!