Dental implant treatment has proven successful and predictable for many years in all indications when placed according to evidence-based guidelines (Buser et al. 2000). Replacement of teeth in the esthetic zone is complex and poses one of the biggest challenges in implant dentistry (Buser et al. 2004). Malpositioned implants, especially facially, lead to esthetic failure with a long clinical crown, mucosal recession and discoloration, and in extreme cases, exposure of the implant (Chen et al. 2015).
A tissue level (TL) implant is one of the earlier designs with several biological and mechanical advantages (Scacchi et al. 2000). Placing TL implants in the esthetic zone has been controversial and regarded as technique-sensitive since 3D implant placement is crucial to clinical success (Wallner et al. 2018) However, when correctly placed, the success of TL implants is predictable in obtaining an optimal long-term result (Derks et al. 2016, French et at. 2019). In a 9-year follow-up study by Derks and co-workers, TL implants showed the least risk for peri-implantitis compared to the other implants (bone level design) (Derks et al. 2016).
The tissue level implant design offers a number of advantages in the esthetic zone:
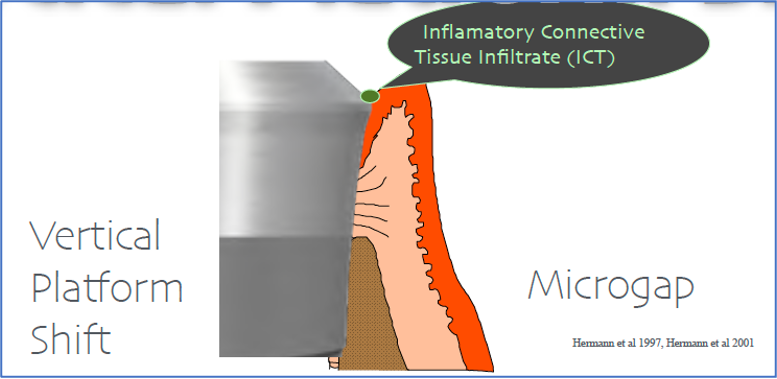
- The machined collar provides a vertical platform that shifts the implant-abutment interface coronally away from the level of bone (Fig. 1). In the bone level (BL) design implant, the horizontal platform shift minimizes marginal bone loss (Lazzara & Porter 2006). However, a recent study demonstrated that in BL implants, the abutment height of 2 mm preserved more marginal bone than an increased horizontal mismatch (Galindo‐Moreno et al. 2016). The vertical mismatch provided by TL implants in default offers a protective effect (Chen et al. 2019, Buser et al. 2012)
- Machined titanium, being an ideal material for mucointegration, creates an undisturbed supracrestal attachment and negates the influence of attachment/detachment of abutment during the prosthetic stages of treatment, and protects against unwanted marginal bone loss (Abrahamsson et al. 1997, Welander et al. 2008). Lately, the influence of this phenomenon has been emphasized with a novel “one abutment – one time” concept (Atieh at el. 2017), whilst it remains a default characteristic of the TL implant.
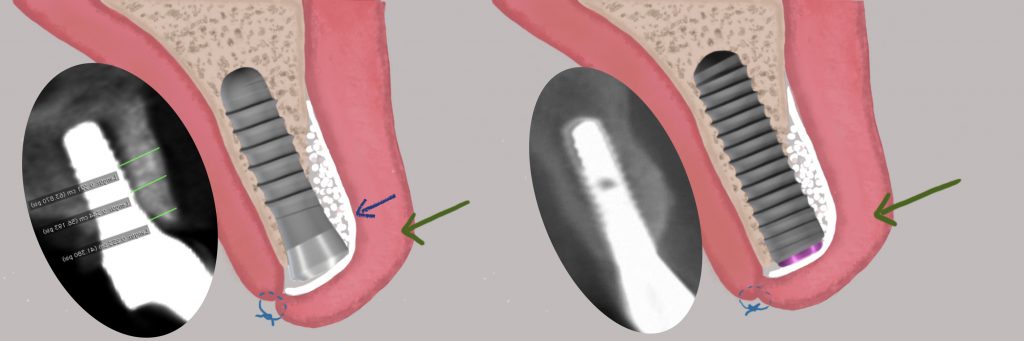
- The range of prosthetic diameters (regular/narrow) helps create an ideal emergence profile and angle (Esquivel et al. 2021) for different clinical situations in the esthetic zone (Fig.2). Different implant diameters and platforms have different emergence angles. This is particularly pertinent in atrophied alveolar ridges where a narrow diameter implant (3.3 mm) might be preferable. A TL 3.3-mm regular neck implant has an emergence angle of 18⁰, allowing for optimal smooth emergence for the crown. In contrast, a 3.3-mm BL implant has to be restored with an even narrower diameter abutment, resulting in over-contoured emergence for the crown (Fig. 2), and may increase the risk of peri-implantitis (Katafuchi et al. 2018, Yi et al. 2020).

- For optimal bone regeneration, the “tulip” shape of the collar provides a kind of reservoir for the particulate bone graft and protects it from collapsing (Fig. 3). This is likely to prevent displacement of the particulate graft after flap closure, which has been shown to displace the graft thickness at the coronal portion of the implant by around 40% (Chiapasco et al. 2014). Besides, the long-term peri-implant bone stability of grafted sites with autogenous grafts is better with TL implants (Chiapasco et al. 2014).
- TL implants offer better biomechanical stability in a one-implant cantilever scenario, avoiding esthetic issues with two adjacent implants (Becker 2004). In the esthetic zone, with limited mesiodistal space for two implants, one-implant cantilevers perform with the same survival and technical complication rates but with better marginal bone levels and papilla fill (Roccuzzo et al. 2020).
TL implant disadvantages in the esthetic zone:
- The width of the peri-implant saucer (after physiological bone remodeling) is greater in TL (1 mm) compared to BL (0.6 mm) (Buser et al 2013). However, the clinical relevance of the 0.4-mm difference is questionable.
- Limited interproximal space might limit its application, especially when placing two adjacent implants. This should be considered in the planning process to maintain a minimum of 3 mm inter-implant distance.
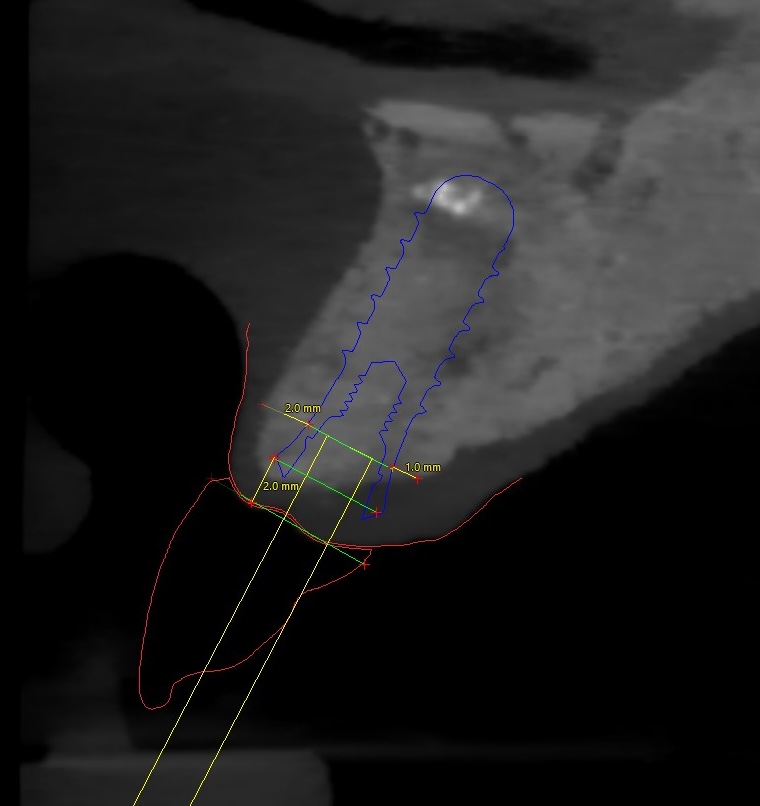
- It is often argued that the 3-dimensional optimal placement of the TL implant is more critical than with the BL implant. A facially malpositioned TL implant could result in more extreme esthetic failure, with exposure of the machined implant collar. However, such a statement trivializes the importance of the same rules of engagement for the BL implant too. In order to preserve at least 1 mm bone at the crest, the implant should be approximately 2 mm palatally from the adjacent teeth (Shahdad et al. 2023). With regard to the implant depth, whilst the TL implant should be placed 2 mm from the proposed mucosal zenith, the BL implant also needs to be placed 3-4 mm apically for an optimal esthetic outcome (Buser et al. 2004).
Important factors to consider when planning optimal placement of tissue level implants:
Preoperative planning:
- The “Esthetic Risk Assessment” tool is highly recommended as it allows the clinician to review patient- and implant-related parameters to ensure long-term success (Buser et al. 2019).
- The prosthetically driven implant position should be dictated by a diagnostic wax-up (conventional or digital). This is critical since the restorative zenith will determine the apico-coronal position of the implant. TL implants must be placed 2 mm away from the proposed zenith (Buser et al. 2004) (Fig. 4).
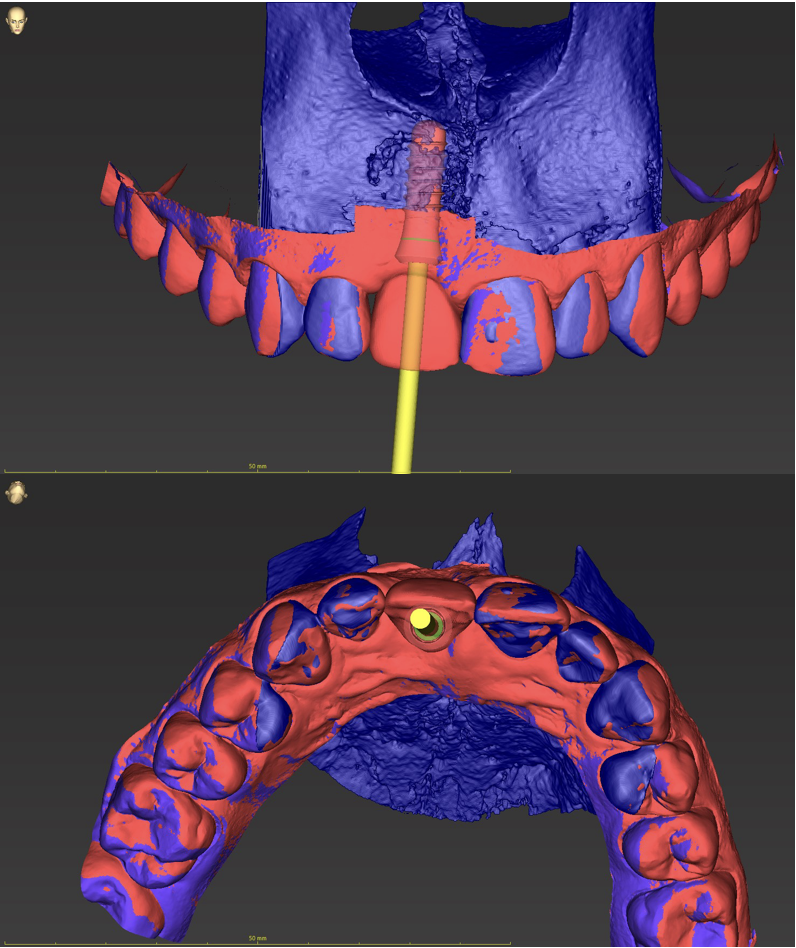
- A digital diagnostic wax-up should be merged with the patient’s CBCT using virtual implant planning software to facilitate optimal implant planning.
- It is advisable to use a cone beam computed tomography (CBCT) for optimal planning. Implant planning software (e.g. coDiagnostiX, Simplant) allows superimposition of the surface scans (.stl files) of the pre-operative situation and the diagnostic wax-up. This ensures the most optimal prosthetically-driven implant planning and fabrication of a surgical guide (Fig. 5). Even the choice of abutment can be made at this stage to consider any prosthetic complications.
The ITI has developed a clinical evaluation tool for determining the surgical or prosthetic difficulty and classified the categories as Straightforward, Advanced and Complex (SAC). Esthetic zone cases are classed as either Advanced or Complex and clinicians need to be aware of many risk factors (Dawson et al. 2022). Only 10% of cases have been reported with facial bone crest thickness of >1mm (Braut et al. 2011). Therefore, GBR for facial-bone-contour augmentation should be carried out in the anterior esthetic zone beforehand or simultaneously to ensure long-term success and stability (Fig. 4) (Buser et al. 2013).
As an ITI Scholar at Queen Mary University of London under the mentorship of Prof. Shakeel Shahdad, I’ve had the opportunity to evaluate numerous patients who have been successfully restored with tissue-level implants in the esthetic zone. I’ve come to realize that meticulous treatment planning, optimal implant positioning, and simultaneous GBR are paramount for successful outcomes when placing implants in such a critical area – irrespective of whether we choose tissue or bone-level implants.






