Introduction
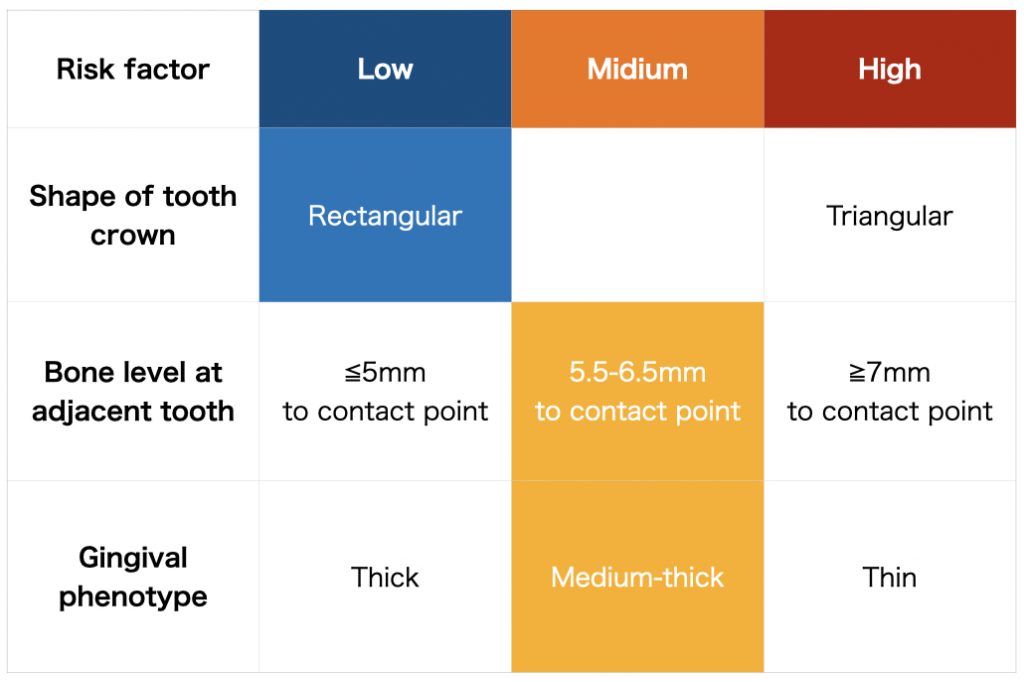
The lack of interproximal papilla in single-tooth implant restorations in the esthetic zone has a significant impact on the esthetic results. In particular, the presence of the gingival papilla is important in medium and high-smile cases. The ITI’s esthetic risk assessment (ERA) documented in the ITI Treatment Guide series was developed to assist clinicians in the diagnosis and planning of treatment in the esthetic zone and to identify clinical situations that could affect esthetic compromise. The ERA is easy to use and includes a comprehensive set of key clinical factors that contribute to treatment risk. In this article, the major risk factors related to the papilla in a single-tooth implant situation were excerpted from the ERA table (Fig.1).
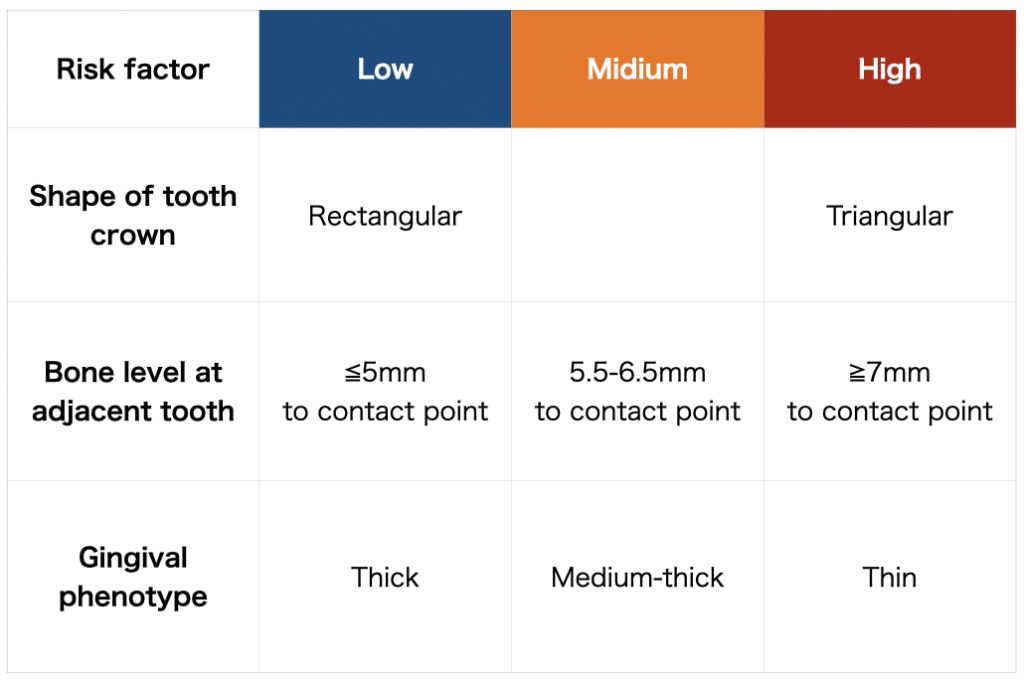
Three risk factors for interproximal papillae in single implant situations
Shape of tooth crown
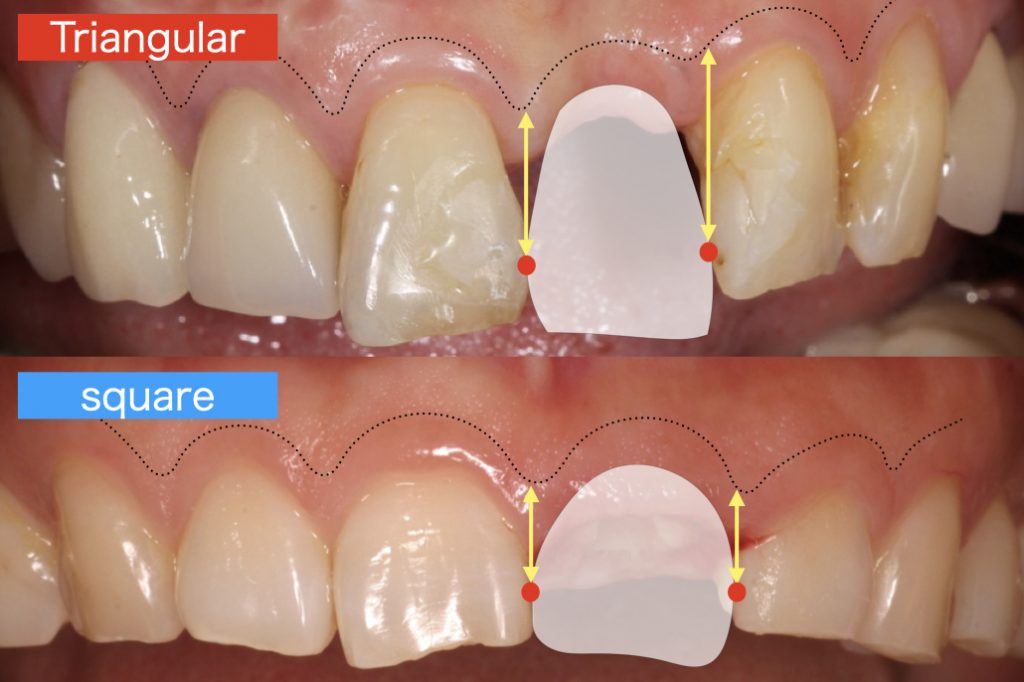
Crown morphology, classified as square or triangular, is one of the most important factors in the formation of an interproximal papilla. If the implant restoration is mismatched with an adjacent tooth, it will generally influence the appearance and final esthetic outcome. This situation can be further exacerbated when the implant restoration is located at the midline.
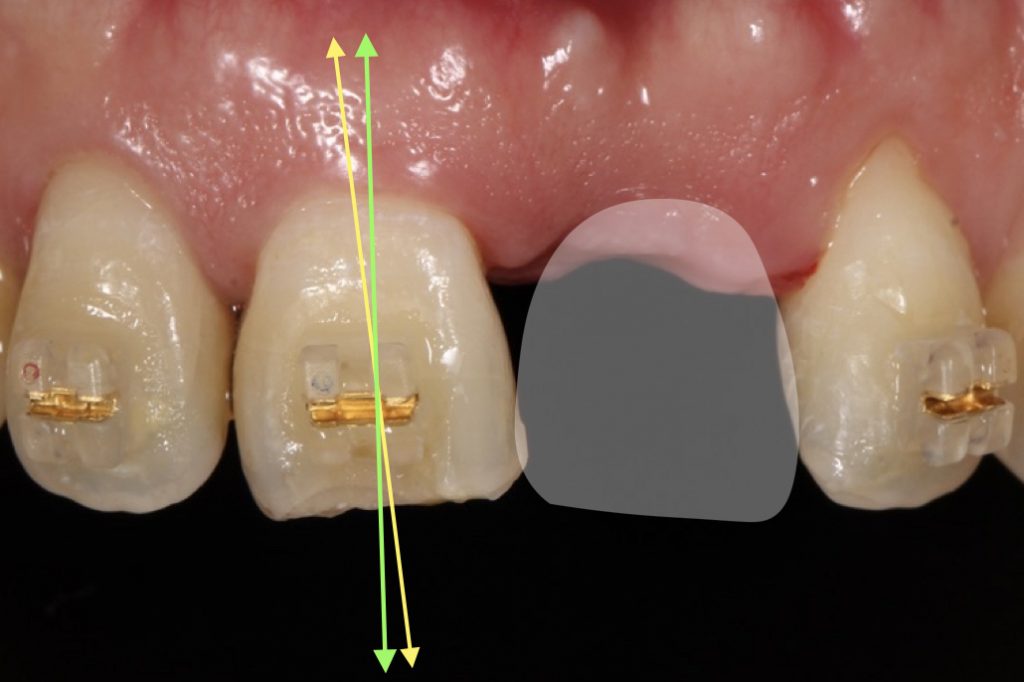
In the square tooth morphology, the black triangle is inconspicuous because the contact position is located on the apical aspect. However, in the triangular tooth morphology, the contact is located on the coronal aspect, therefore if the papilla is lost, the black triangle will be conspicuous. In addition, triangular tooth morphology will be more often associated with a thin phenotype (Fig. 2).
Bone level at adjacent tooth
The gingival papilla will decrease accordingly if there is alveolar bone loss around adjacent teeth which can be assessed by dental X-ray or CT images.
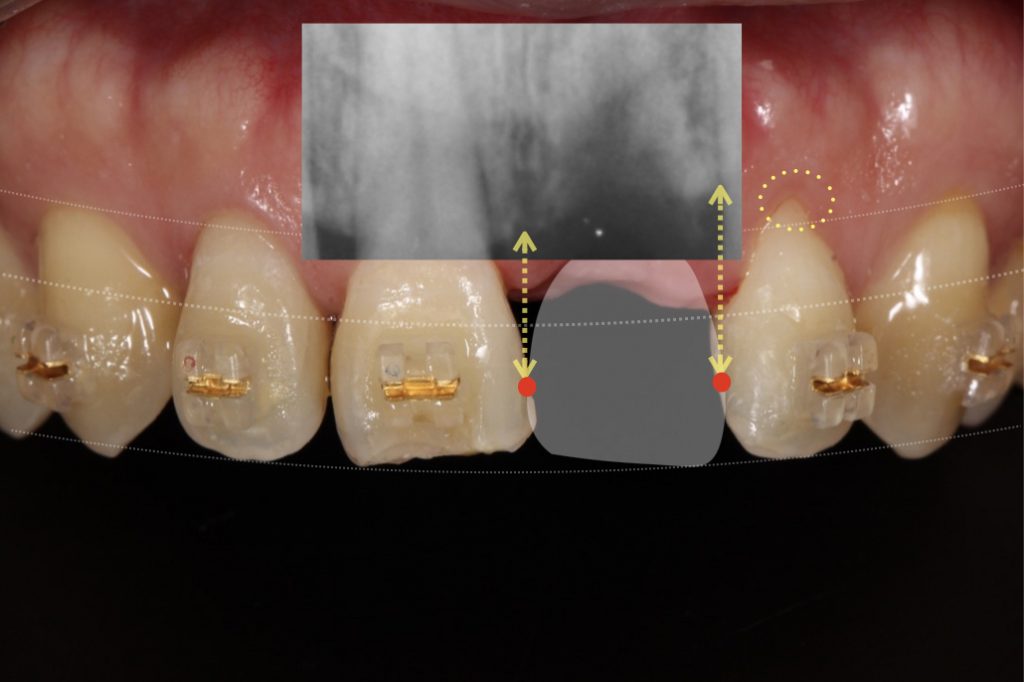
In terms of the papilla, the ideal distance from the interproximal bone crest on the adjacent tooth to the apical extent of the contact point should be within 5 mm. Black triangles are expected due to missing bone adjacent to a missing tooth (Fig. 3).
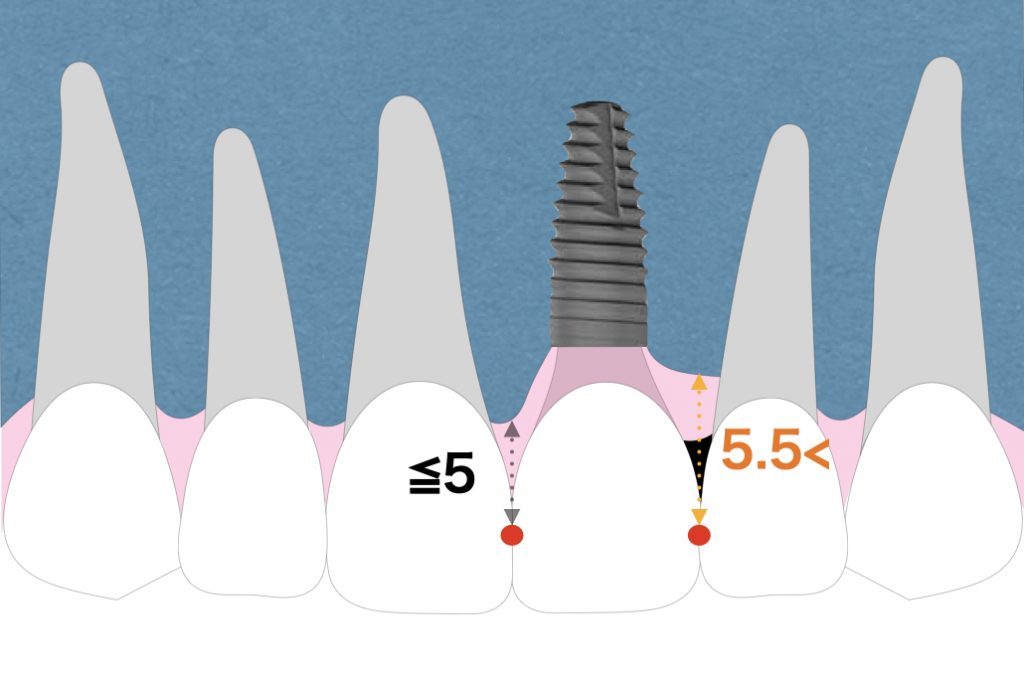
When the papilla at the adjacent tooth is retracted due to bone loss, it is difficult to be reconstructed by partial vertical bone augmentation. A connective tissue graft onto the tooth defect or morphological modification of adjacent teeth is necessary to make the black triangle less noticeable.
Gingival phenotype
If the gingival phenotype is thin, gingival recessions are likely to occur. As a simple diagnostic method, if, after insertion into the pocket, a color-code probe is visible, the patient is assessedas being a thin phenotype. Otherwise, the patient is assessed as a thick phenotype (Fig. 4).
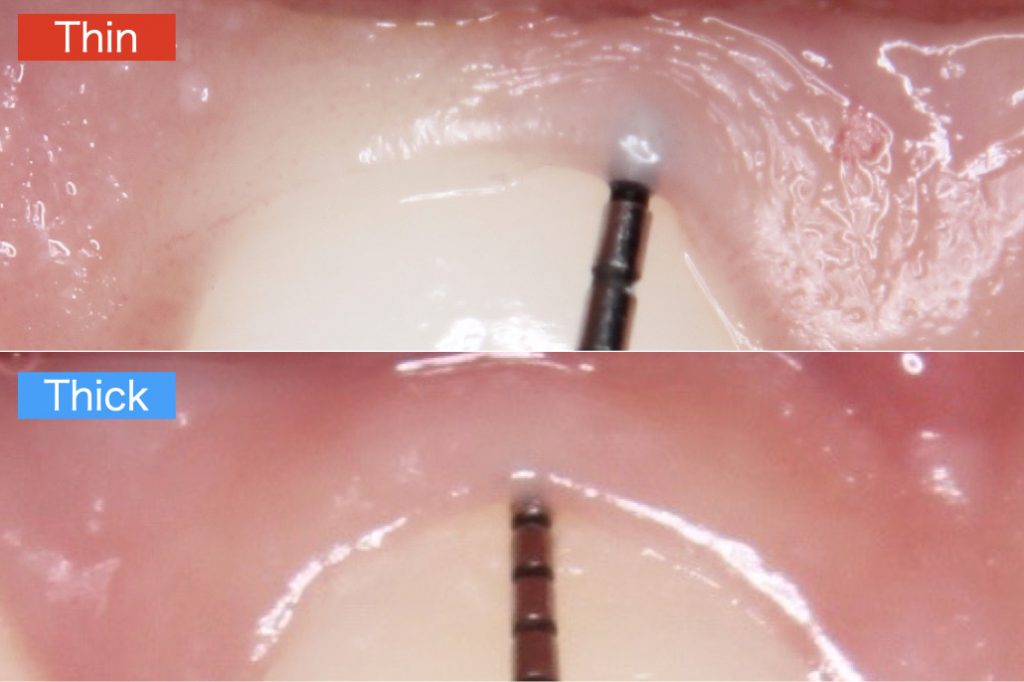
Sufficient soft tissue thickness should be created on the labial side when attempting to reconstruct the gingival papilla. For soft-tissue augmentation, autologous tissue has to be considered as the treatment of choice resulting in an increase in soft-tissue thickness at implant sites, even though some soft-tissue shrinkage has to be expected.
How to evaluate and manage interproximal papillae
Immediate implant placement is known to be effective as a means of avoiding invasion of the gingival papilla adjacent to the implant and maintaining the papillae. However, immediate implant placement is only indicated in carefully selected situations due to the loss of alveolar bone and soft tissue associated with root fracture or infection of non-restorable teeth. Therefore, this section introduces methods for managing the papillae except for immediate implant placement.
The photo shows a patient who lost the anterior tooth due to trauma (Fig. 5, Fig. 6). The risk of the loss of the gingival papilla was evaluated using three risk factors, and the following evaluation results were obtained (Fig. 8).
Shape of tooth crown
The central incisor was determined to be of a rectangular shape and was inclined medially. A black triangle is expected to form in the medial and distal sites due to the coronal position of the contact point (Fig. 5). Direct bonding on the medial of the upper right central incisor or orthodontic treatment can make the black triangle less noticeable as the contact point will be apical. In this case, orthodontic treatment was planned to improve the tooth axis.
Bone level at adjacent tooth
The X-ray shows a slight bone loss on the distal side of the missing tooth. Therefore, the distance between the alveolar bone and the contact point is longer than normal (Fig. 6).
Gingival phenotype
Oftentimes a square crown morphology is associated with a thick phenotype. However, this patient was diagnosed as a thin phenotype because the color of the probe was perceptible when the probe was inserted into the pocket (Fig. 7).

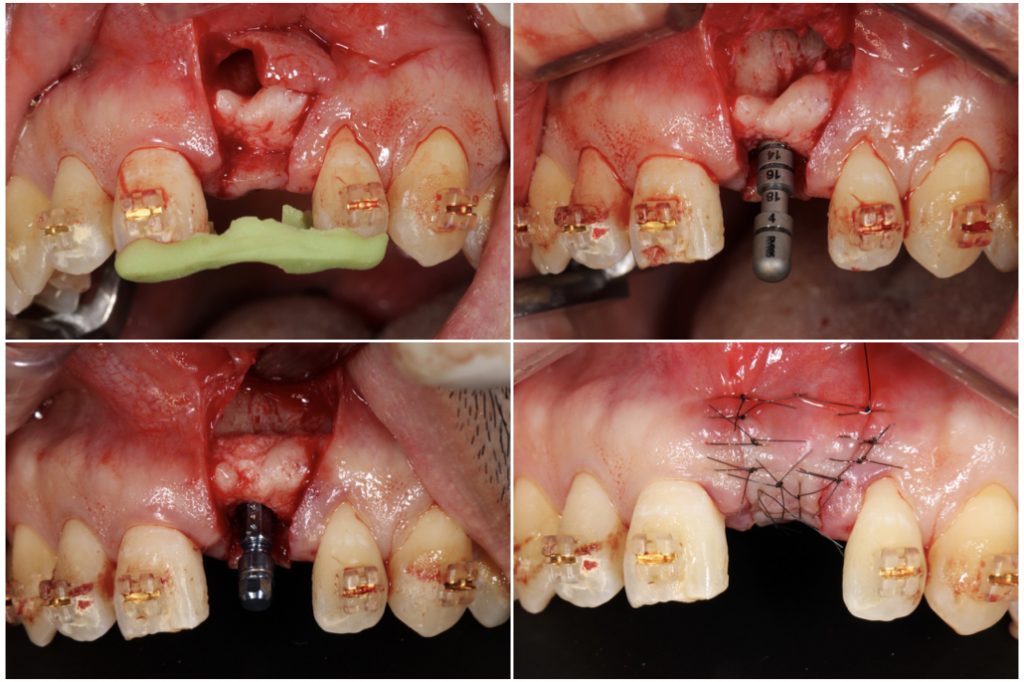
Therefore, the risk for the gingival papilla was intermediate in this case. A connective tissue graft was used in order to change the gingival phenotype from thin to thick.The incision was made avoiding the papillae of the adjacent teeth. A bone-level implant was placed with the platform positioned at a depth of 3 mm from the ideal cervical line (Fig. 9).
A provisional restoration was placed 3 months postoperatively. Connective tissue grafting was performed to reconstruct the papillae and to prevent gingival recession. A vertical incision was placed in the vestibule, remote from the treatment area. Through this incision, a subperiosteal tunnel was created, extending toward the vestibular depth as well as the ridge crest. Then connective tissue was inserted from the incision. This surgical procedure is minimally invasive and superior in terms of blood supply to the graft because it doesn’t need an open flap procedure. Sutures at the papillae were fixed with composite to the crown for traction of the flap (Fig. 10).

Eighteen months after loading. A zirconia‐based screw‐retained prosthesis was applied to the implant. The gingival papillae were stable (Fig. 11).

Conclusion
In this article, three risk factors related to interproximal papillae around a single implant were excerpted from ERA in the ITI Treatment Guide using a case report.
Of the 3 risk factors, tooth morphology can be modified to some extent by direct bonding, orthodontic treatment, and prosthetic procedures. In addition, phenotypes can also be partially improved by a connective tissue graft. However, loss of the gingival papillae associated with bone loss in adjacent teeth is difficult to recover and requires special attention.
The evaluation of 3 risk factors simplifies the risk assessment for the preservation of the papillae in a single implant situation. It is necessary to fully explain the expected outcome of the treatment if the risk is high and to find a compromise between the dentist and the patient. Using this table during consultation can be a valuable tool for achieving esthetic implant outcomes in the dental practice, however, more importantly, it spares dentists from having to deal with unexpected esthetic complications.