Introduction
In the last three decades, there has been an improvement in oral health standards in industrialized countries and therefore a decrease in complete edentulism. However, partial edentulism has increased due to the aging population. Historically, partial edentulism was treated with fixed dental prostheses (FDPs) or partial removable dentures. Later, with the discovery of osseointegration, the use of titanium fixtures to support FDPs gained popularity, to the point where more than 10 million dental implants are now placed each year worldwide.
During the last two decades, due particularly to the increasing prevalence of peri-implant diseases (Romandini et al. 2021; Roccuzzo et al. 2022), the use of cantilever extensions as an alternative treatment option has been proposed to reduce the number of implants placed, to avoid bone augmentation procedures and to provide patients with sufficient functional units.
When focusing on the use of cantilever extensions on dental implants and the increased risk of failure, controversial results have been published in several systematic reviews. However, recent long-term data suggest this treatment option is reliable, underlining how the presence of a cantilever extension did not have a detrimental effect on the implant failure rate, despite its location.
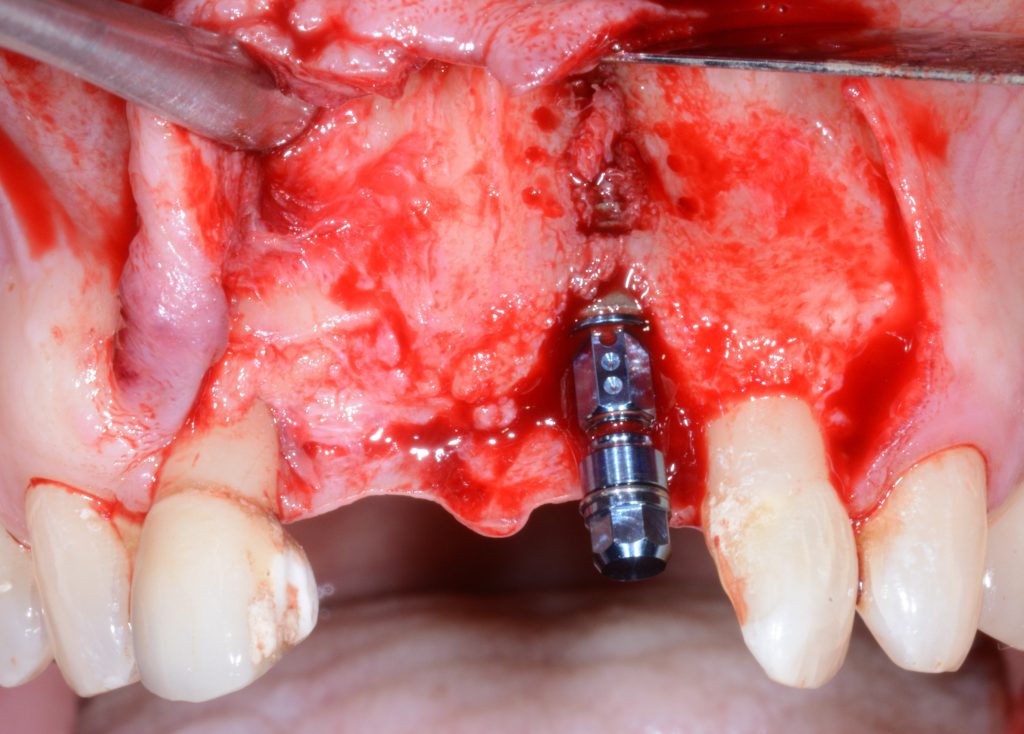
From a clinical perspective, the anatomical situation is a key factor that might encourage the application of implant-supported partial FDPs with cantilever extensions to prevent and reduce complications related to anatomical structures such as the mental nerve, incisive canal, and lingual concavity.
The use of a cantilever can be considered a minimally invasive option, especially if associated with short implants when the available bone is reduced or compromised. This approach makes it possible to prevent additional bone augmentation procedures.
Placement of a single implant with a cantilever in the esthetic zone is a suggested treatment when two teeth are missing in order to prevent interproximal papilla loss.
During the patient selection and treatment planning processes, it is crucial to identify and evaluate the presence of parafunctional habits that may cause biological or technical complications, such as implant loss, peri-implantitis, screw loosening, chipping of veneering material or abutment fracture (Blanes et al. 2007; Hämmerle et al. 2018). As reported by Schmid et al. (Schmid et al. 2020), loss of retention in cement-retained reconstructions occurred in 34.6% of cases in a sample of 60 implants; a possible reason given for this was the presence of premature contacts on the cantilever extension. Consequently, the authors suggested that the static and dynamic contacts should be corrected during occlusal function as part of the maintenance care program.
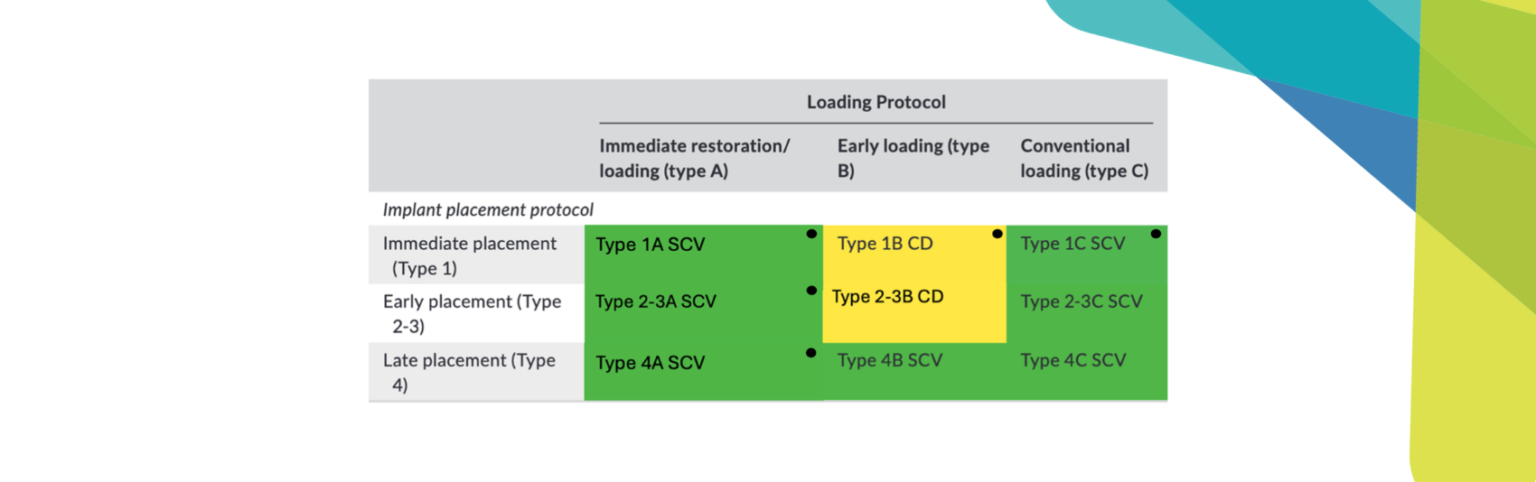
Surgical and prosthetic factors
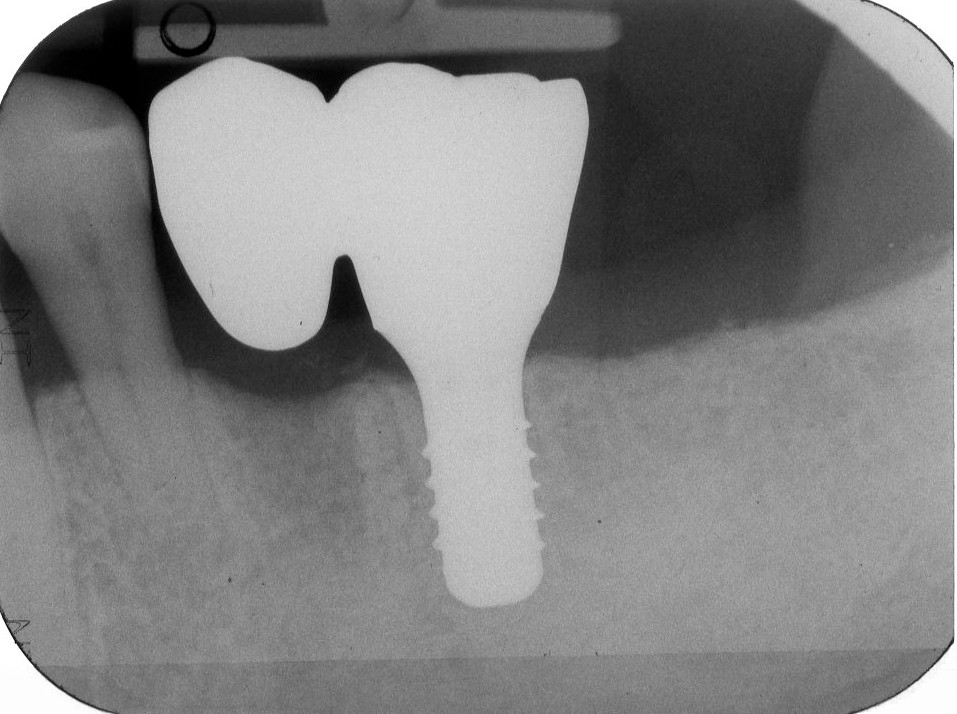
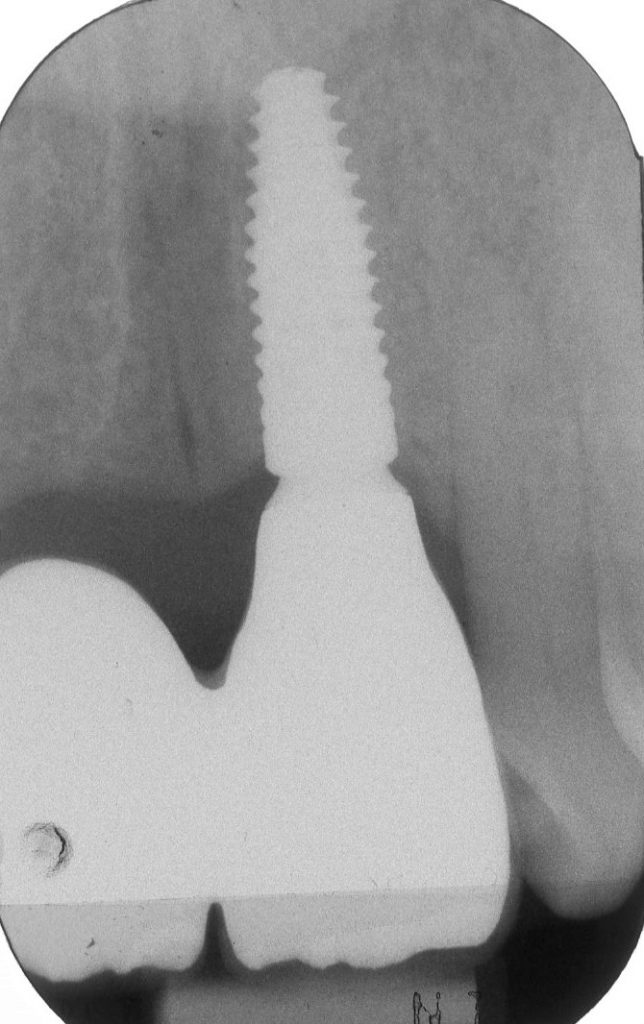
Prior to implant placement, several implant-related factors need to be considered, such as implant type (bone- vs tissue-level), length, diameter, and prosthetic connection. More specifically, whenever an extension is planned, it is crucial to bear in mind that the use of a cantilever, from a mechanical point of view, might appear to be an unfavorable condition primarily due to the stress placed on the implant connection segment and on the marginal area of the implant (Romanos et al. 2012). Implant design and geometry may influence the survival rate of cantilever units.
Implant diameter has been negatively associated with an increased risk of implant fracture which, although a rare occurrence, has been reported in some studies (Schmid et al. 2020; Palmer et al. 2012). Hälg et al. (2008) reported two cases of implant fracture after 2.5 and 3.8 years of loading, while Schmid et al. (2020) reported one case of implant loss after 11.3 years of loading. These lost implants were all Ø 3.3 mm in diameter (Schmid et al. 2020; Hälg et al. 2008).
With respect to short implants, this can be deemed a reliable treatment option when the posterior region might present limited bone conditions for implant placement and when anatomical structures, such as the maxillary sinus or inferior alveolar nerve, need to be preserved (Hälg et al. 2008). From a clinical point of view, standard-length implants are recommended to increase stability and limit the risk of implant loss.


With respect to the restorative materials that may be employed for prosthetic rehabilitation of implant-supported FDPs with cantilever extensions, metal-ceramic restorations based on precious alloy-ceramic restorations are supported by the most evidence in the posterior zone. Very recently, improvements in CAD/CAM technology for prosthetic design and fabrication showed that zirconia has favorable clinical outcomes and excellent biological and technical properties. From a biological, technical and esthetic point of view, zirconia’s properties and behavior are extremely well suited to patients’ needs and use in the peri-implant tissues. The main reported limitations are chipping of veneering materials and fracture of the crown or connection. However, at the present time, evidence on the possible applications of zirconia restorations on cantilever units is still scarce.
One of the main concerns related to the use of cantilever extensions is the high risk for technical and mechanical complications such as screw-loosening or implant abutment fracture, fracture of veneering ceramics, decementation, and chipping.
At the present time, most of the available evidence is on cantilevers in posterior sites, while only three clinical studies documented this treatment modality with positive results in the mid-term in esthetic areas. Wu et al. (2013) used metal-ceramic with precious alloys and reported one case of screw loosening and no other complications. Roccuzzo et al. (2020) studied metal-ceramic restorations and reported no biological or prosthetic complications. Similar results were reported by Van Nimwegen et al. (2017) with all-ceramic restorations at a 5-year follow-up. Nevertheless, further clinical studies are needed to assess the reliability of cantilevers in the esthetic zone.



Clinical performance
Implant survival rate is defined as the presence of a previously placed dental implant in the oral cavity at the follow-up examination with or without complications linked to the implant placement or prosthetic phase.
Cantilever units do not seem to affect the survival rate of implants loaded with this type of rehabilitation. In a retrospective study of 46 implants with a 5-year follow-up, Hälg et al. (2008) reported a survival rate of 95.7% for implants with cantilever units compared to single implant crowns with 96.9%. Similar data were reported by Romeo et al. (2009) with a sample of 116 implants after 8.2 years of follow-up: the survival rate with cantilever units was 80.0%, and with single implant crowns it was 90.5%. Schmid et al. (2021), after a follow-up period of at least 10 years, reported a survival rate of 100% in a group of 25 implants where 48% were classified as healthy and 52% displayed peri-implant mucositis.
Survival rate needs to be considered as a descriptive parameter that can define the situation; however, it is important to underline that the survival rate alone is not sufficient. Success is defined as the condition where the implants are in situ without any kind of biological or technical complications over the entire follow-up period.
The prosthesis survival rate has been defined as the presence of the restoration in the same position and in the same original extension over a specific follow-up period without it needing to be remanufactured when complications occur.
With cantilever units, the prosthesis survival rate was shown to be lower than with single-unit crowns. Hälg et al. reported a prosthesis survival rate of 88.9% for the cantilever group and 96.3% for the control group (Hälg et al. 2008). In several systematic reviews, technical complications were the most common issue affecting cantilever units, and chipping, screw loosening or abutment fracture were the most reported complications.
One of the major concerns among clinicians is the potential detrimental effect of cantilever extensions on peri-implant marginal bone levels. Indeed, marginal bone loss is the primary outcome and the most common parameter reported in cantilever studies; it is used to evaluate the possible presence of overloading and/or biological complications related to the implant. According to a recent systematic review, the presence of a cantilever does not negatively affect peri-implant marginal bone levels; indeed, the use of these types of prosthetic rehabilitation can cause more technical than biological complications.
Conclusions
Cantilever extensions can be considered a reliable therapeutic option in both the anterior and posterior regions. They offer the advantages of minimal invasiveness, reduced treatment time and costs. This treatment modality might be suggested for non-compliant patients in whom the number of implants placed needs to be kept to a minimum, or patients with economic issues. From a clinical perspective, the use of a cantilever might facilitate treatment of patients with insufficient bone or help to avoid contact with vital anatomical structures. However, the prosthetic maintenance requirements, technical complications that have been reported in the literature, the need to determine a favourable extension of the cantilever and the difficulties posed by the type of tooth to be replaced must all be kept in mind.