Abstract
Immediate occlusal or non-occlusal loading cases are often carried out using prefabricated temporary abutments onto which chairside or prefabricated provisional restorations are relined or directly cemented. An alternative technique can be applied using a titanium base abutment as both a temporary and definitive abutment. The present article presents the advantages of using a titanium base abutment as both a temporary and definitive abutment in an immediate non-occlusal loading case in terms of both biological preservation of tissues and clinical efficiency in reducing chairside time and treatment cost.
Introduction
Advances in surgical implant placement techniques and implant surface design have led to modifications to the initial protocols that required undisturbed healing for 3 to 6 months before prosthetic loading through the concept of immediate loading (Cosyn et al., 2019). This concept is defined as loading of implants at a maximum of one week after their placement as defined by the last three ITI Consensus Conferences in 2003, 2008, and 2013 (Chen et al., 2014), and can be either an occlusally loaded or non-occlusally loaded restoration (Wang et al., 2020), with high survival rates immediately post-extraction (98.8%) or in healed sites (99%) (Galluci et al., 2018; Atieh et al., 2010), considering that certain clinical guidelines have been met including but not limited to: appropriate bone quality and quantity, excellent primary stability or insertion torque, and adequate keratinized tissue (Chung et al., 2011;Wismeijer et al., 2018).
The immediate loading approach, whether occlusal or non-occlusal, stabilizes the gingival architecture and the existing bone with the added advantage of providing the patient with a temporary restoration at the surgical phase, thus reducing the overall treatment time (De Rouck et al. 2008). Immediate loading is usually done on metal, temporary abutments that are hand-tightened onto the implant. The provisional shell/tooth is relined onto the abutment with the intent of replicating the cervical emergence anatomy of the missing tooth and adjusting the provisional to clear functional contacts in centric and eccentric jaw movements (Chung et al., 2011).
It has been previously reported that a supracrestal tissue attachment is formed and matures to act as a barrier around implants within a period of 6 to 8 weeks (Vignoletti et al., 2009),while others report that the loss of peri-implant bone and soft tissue alterations, whether in immediate post-extraction cases or on healed sites, continue for up to one year (Kan et al., 2000; Lang et al., 2011). Thus, the choice of immediate temporary abutments and their effects on molding the peri-implant soft and hard tissues should be considered.
Prefabricated cylindrical temporary abutments, made of plastic or titanium, are used in immediate loading cases to retain the provisional restoration(s). However, not all implant systems offer these abutments in varying gingival heights and angulations. In addition, prefabricated temporary abutments do not allow for a full digital workflow as they are not incorporated into the libraries of digital designing softwares, thus increasing chair time and the total cost of the restorative protocol.
Titanium base (ti-base) abutments, were introduced as definitive abutments that allow for the precise fabrication of implant-supported prostheses in a shorter time, using a digital workflow through CAD/CAM systems (Tribst et al., 2019). Thus, these abutments are considered a strong link between the implant and the ceramic abutment/crown and provide a favorable esthetic outcome (Yilmaz et al., 2015). Ti-base abutments are known to offer several advantages, one of which is the extraoral cementation of the definitive prosthesis. However, little attention has been given to the possibility of using ti-bases as immediate, temporary implant abutments. This case report presents the use of a ti-base abutment, as both a temporary and definitive abutment in an immediate non-occlusal loading case, demonstrating its possible advantages in preserving peri-implant soft and hard tissues and its clinical efficiency in reducing chairside time and treatment cost.
Case report
Pretreatment evaluation
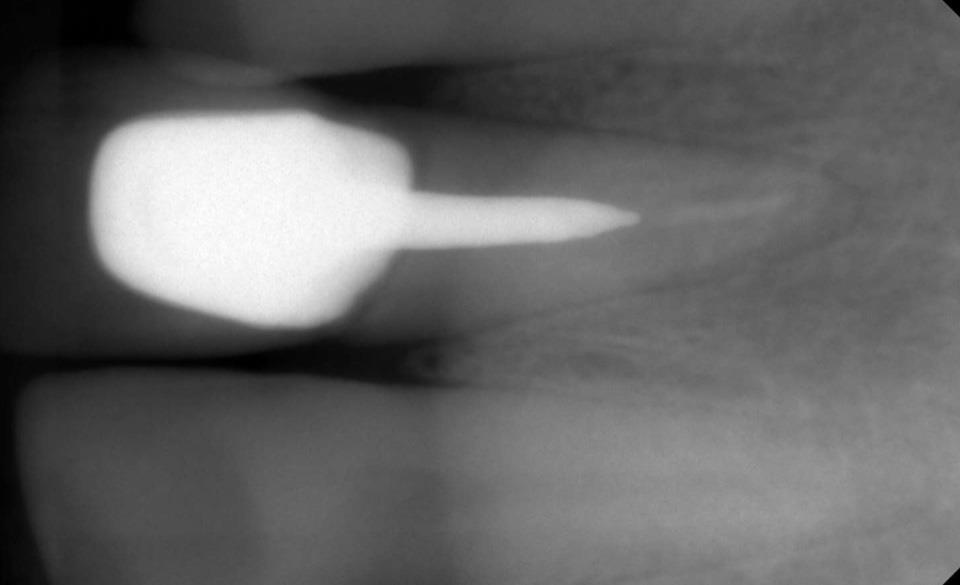
A 45-year-old healthy, non-smoker male presented to a private dental clinic to replace his upper right central incisor. The patient had a clear medical history with no active dental disease and no contra-indications to implant therapy. The patient expressed his frustration with the post and core crown repeatedly falling off which required frequent visits to another dental clinic for recementation of the prosthesis. An intraoral clinical examination (Fig. 2) revealed signs of parafunctional habits with incisal tooth wear extending into the dentin and multiple enamel cracks. The underlying tooth structure revealed limited remaining tooth structure for a crown ferrule. The gingival biotype was classified as thick using the probe transparency test. A periapical radiograph (X-Pod; myray, Imola, Italy) (Fig. 1) revealed inadequate bony support of the root and an unfavorable crown-to-root ratio with an overall poor prognosis if a re-endodontic treatment, surgical crown lengthening, and fabrication of a replacement post and core crown were to be performed. The case was classified as advanced, according to the ITI SAC Assessment Tool, and the tooth was indicated for extraction and immediate implant placement.

Presurgical phase
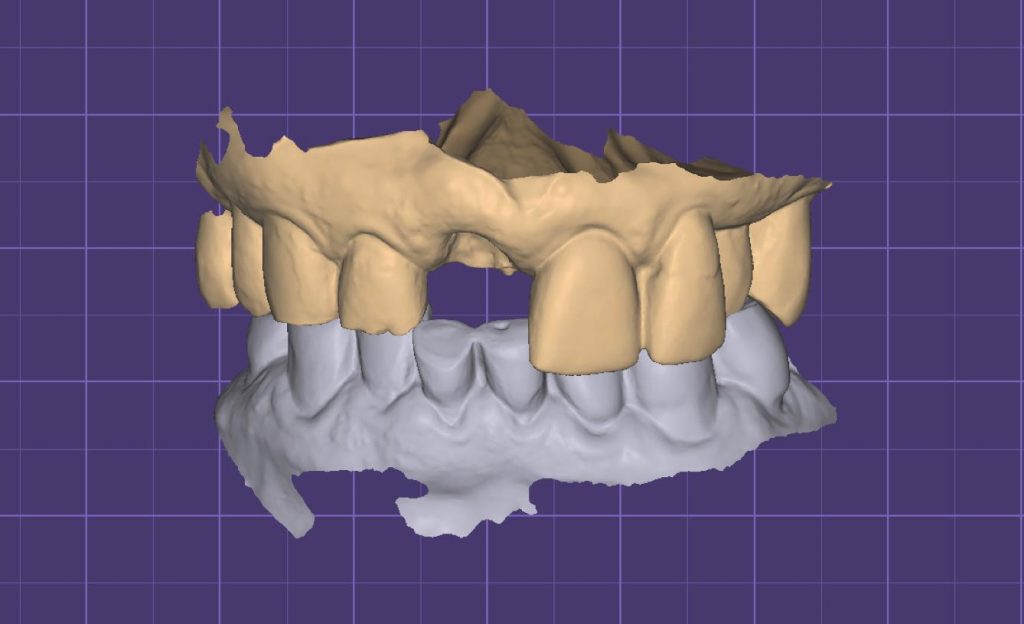
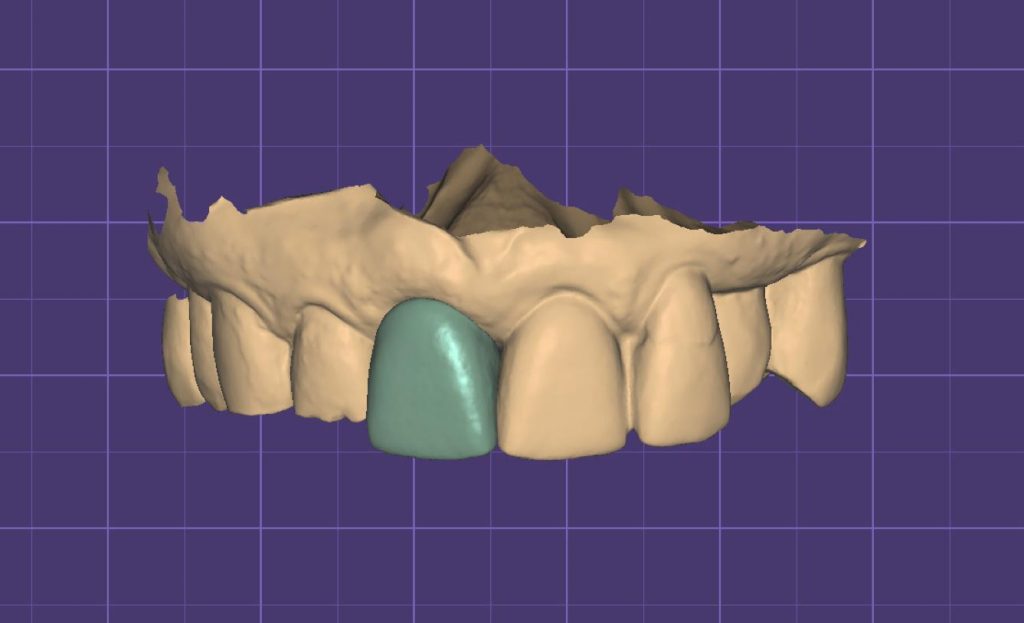
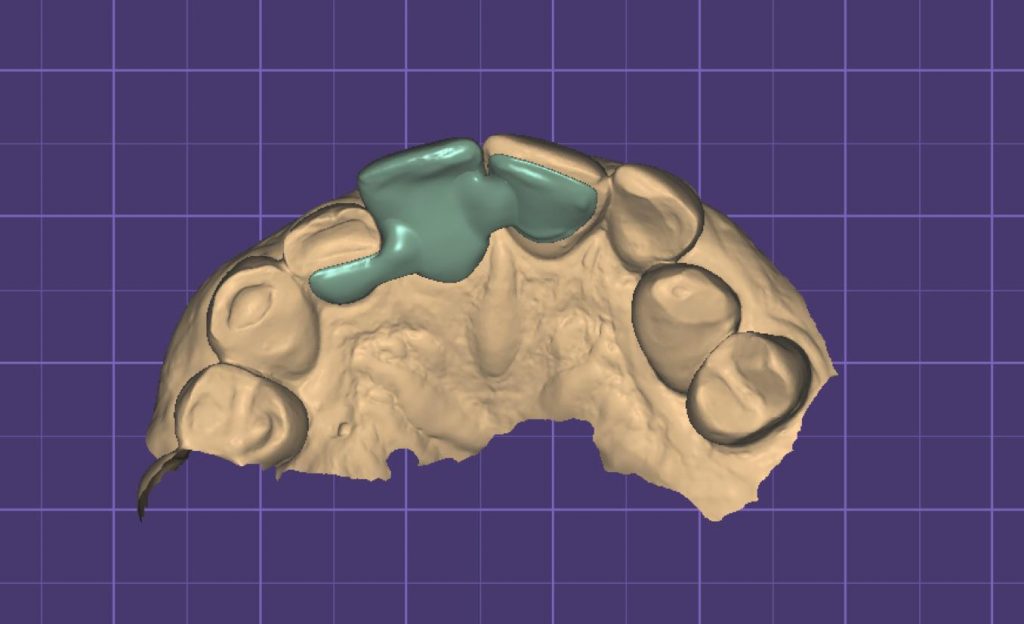
A preoperative intraoral scan was registered with an intraoral scanner (TRIOS® 3, 3shape), and the upper and lower arch scans registered in occlusion (Fig. 4a) were imported into the design software (DentalCAD 3.0 Galway; Exocad). To create a polymethylmethacrylate (PMMA) temporary shell (TempShell), the missing tooth was designed by mirroring the adjacent central incisor (Fig. 4b) and adding wings supported on adjacent teeth (Fig. 4c) to guide its labio-palatal positioning intraorally during relining (Fig. 5). The Standard Tessellation Language (STL) file of the final design was then exported to a milling machine (Planmeca PlanMill® 40 S; PLANMECA) for fabrication, and thereafter stained with acrylic resin (Minute Stains; Taub dental, New Jersey, United States) to mimic the contralateral tooth. The Tempshell was tried intraorally to verify its esthetic anatomy and shade and assess its proper seating on adjacent teeth (Fig. 6).


Surgical protocol
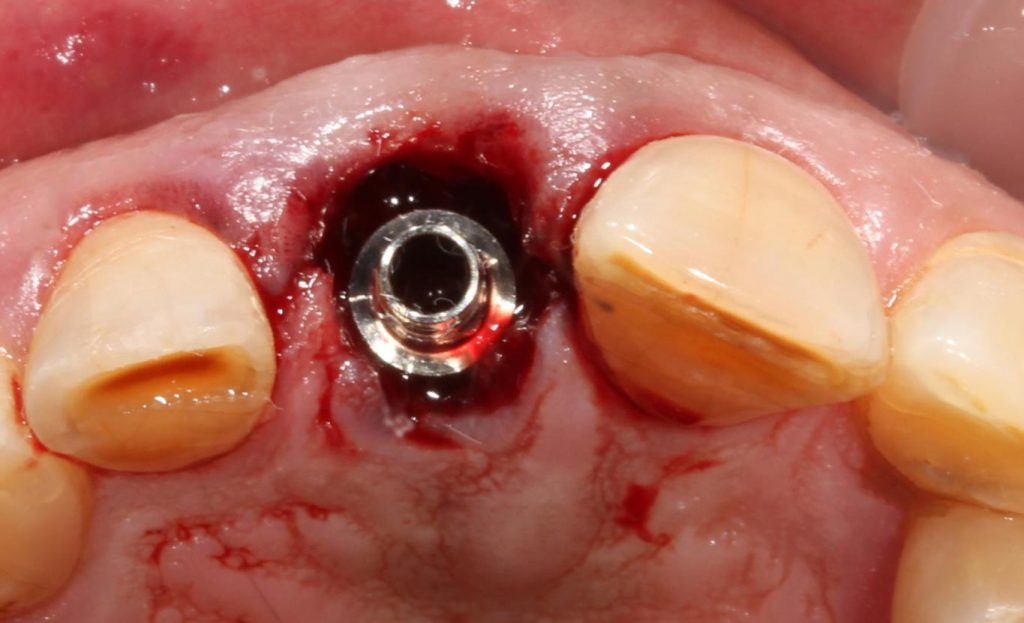
The patient was first asked to rinse with chlorhexidine solution (0.12%) for 1 min. Then local maxillary infiltration and a palatal injection were performed with articaine 4% with 1:200,000 epinephrine (Septanest; Septodont). Atraumatic, flapless tooth extraction was performed by separating the supracrestal gingival fibers with an anterior periotome (Anterior Periotome No.2; Hu Friedy). Thereafter, the tooth was extracted using forceps (Upper Anterior, Apical, Atlas; Hu Friedy) with minimal damage to the hard or soft tissue to preserve the integrity of the surrounding bony structure and gingival architecture. After extraction, the alveolar socket was generously irrigated with normal saline solution and curretaged (Lucas Surgical Curette, CL 86, Hu Friedy) to remove any granulation tissue. The presence of adequate surrounding bone was confirmed using the implant depth gauge (Straumann®). A bone-level implant (RB TorcFit BLX∅ 3.75 mm, length 12 mm; Institut Straumann®) was immediately inserted according to the manufacturer’s recommendations without opening a flap where it was placed approximately 1mm below the buccal bone plate and 4 mm below the gingival margin. Although it was placed with the free-hand technique, it was directed in accordance with the ideal prosthetically driven position, later confirmed by the angulation of the ti-base abutment screwed onto the implant fixture. Primary stability was confirmed at an insertion torque of 50N and an implant stability quotient (ISQ) value of 70 (Osstell; W&H company).
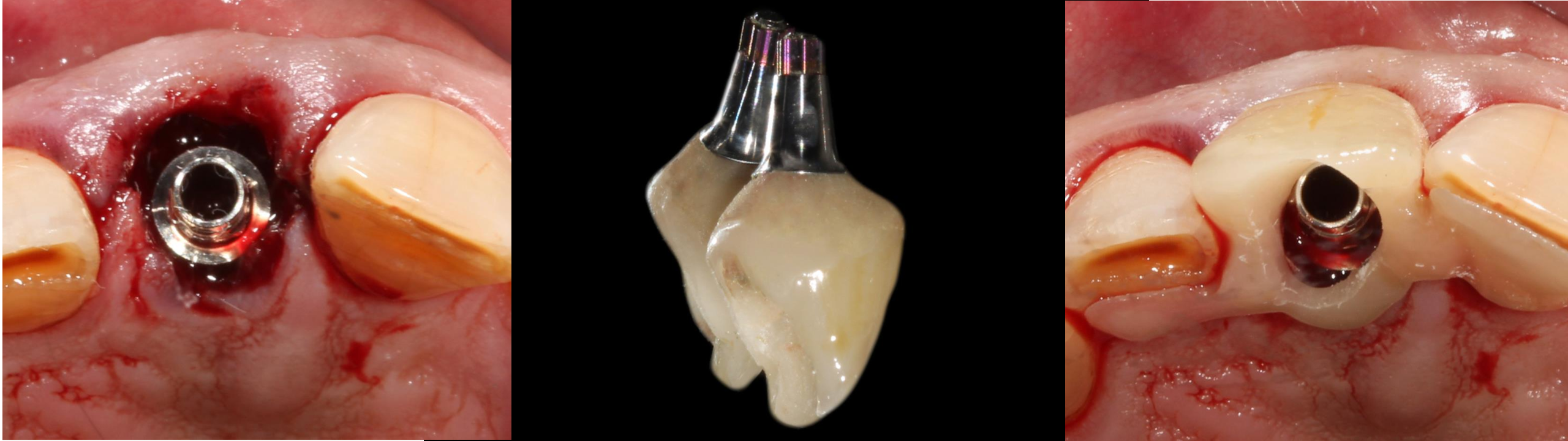
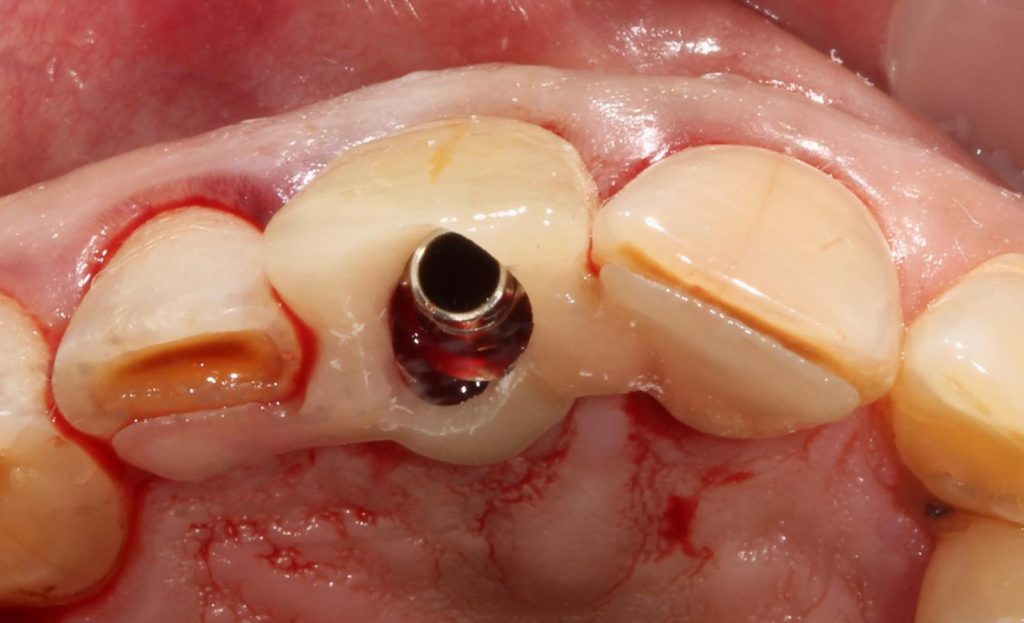
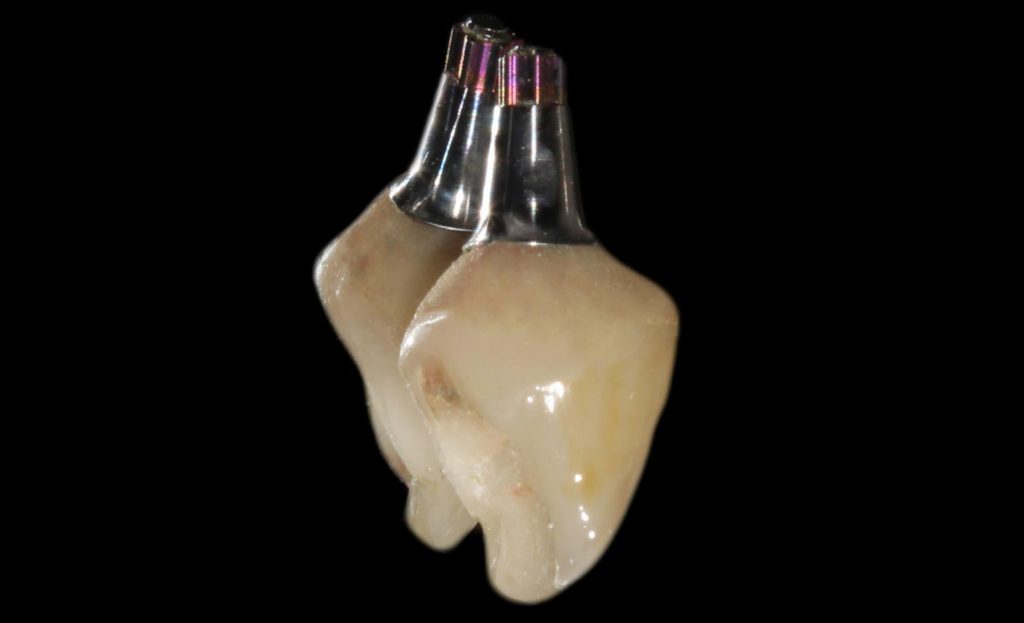
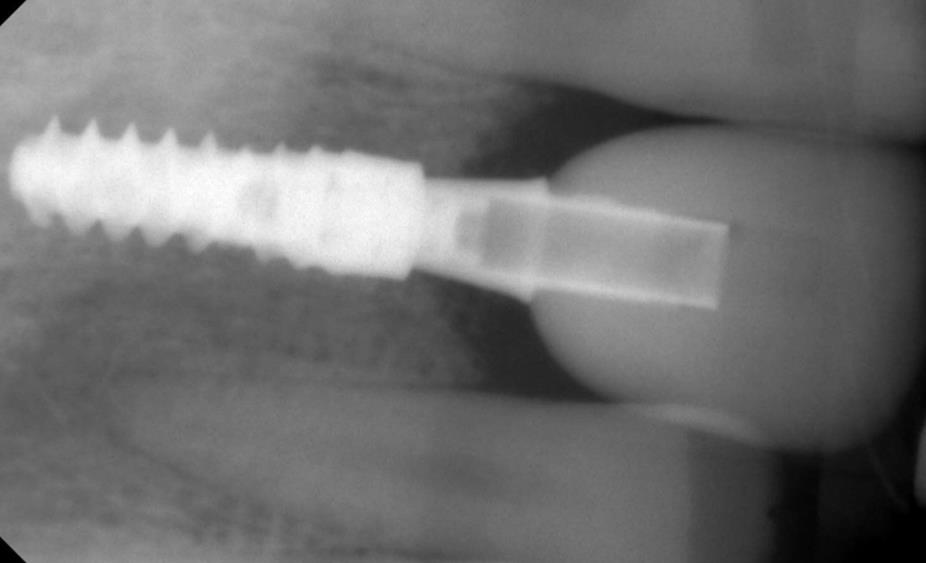
The titanium base abutment (Variobase® for Crown, GH 3.5 mm, AH 5.5 mm, Institut Straumann®) was hand-tightened onto the implant (Fig. 7) followed by the try-in of the TempShell to ensure optimum fitting before relining (Fig. 8). To capture the subgingival contour of the soft tissues and create an emergence profile, the TempShell was loaded with self-cured acrylic resin (ALIKE™; GC America) and the mechanically locked TempShell over the Variobase® was removed as a single unit. The relined restoration was then disinfected and placed onto a laboratory analog (RB/WB Implant lab analog – L 12 mm, TAN, Institut Straumann®) on which the final contouring of the emergence profile was established with resin (Fig. 9). The wings of the TempShell were then removed and the temporary was finished and polished with pumice. The provisional restoration was replaced onto the implant and assessed clinically to confirm esthetics and contour, and occlusion was adjusted accordingly. A flat-contoured healing abutment was then placed, and a xenograft bone graft material (Bio-Oss®; Geistlich Pharma AG) was packed in the gap between the implant and the buccal wall of the extraction socket. A collagen matrix (RCF Resorbable Collagen FOAM, ACE Surgical Supply Co., Inc.) was adapted over the bone graft to support it. The healing abutment was then unscrewed, and the provisional restoration was tightened onto the implant at 35N (Fig. 10). The screw hole was plugged with Teflon and flowable composite resin (Tetric N- Flow; Ivoclar Vivadent). Follow-up visits were performed after 1 week and 1 month. At 4 months, a periapical radiograph was taken to verify satisfactory healing. The provisional restoration was removed for the first time, and the peri-implant soft tissues revealed no signs of redness, swelling, or bleeding along with a well-established gingival sulcus. ISQ value was 85 (Papaspyridakos et al., 2014), ensuring desirable osseointegration of the implant with the surrounding bone.

Restorative protocol
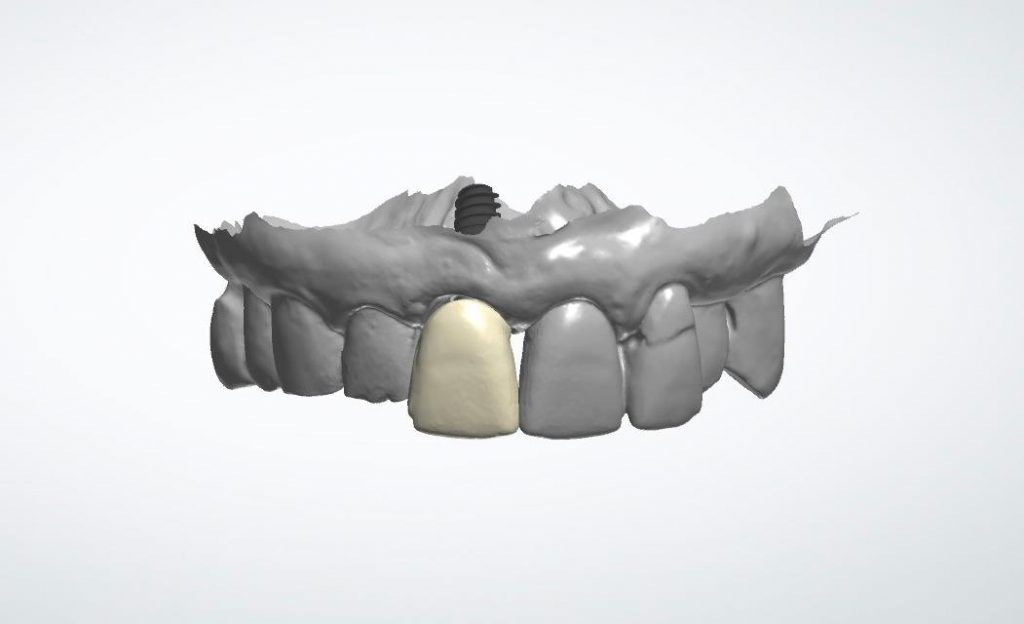
To register an emergence profile scan, the screw-retained temporary prosthesis was removed, and the soft tissue profile was scanned immediately along with the complete upper arch. The soft tissue profile was locked in the scan using the locking tool, and an implant-level scan body (CARES® Mono Scanbody, PEEK/TAN, Institut Straumann®) was tightened to transfer the implant position (Fig. 11). A virtual Variobase® of the same gingival and abutment height of the temporary was selected over which a zirconia crown was digitally designed to meet the functional requirements of the patient’s parafunctional habits (Figs 12 – 13) and minimize unfavorable occlusal loading. The STL file of the design was then sent to a milling machine (CORiTEC 250i; imes-icore) to produce a monolithic zirconia crown (IPS e.max® ZirCAD® MT; Ivoclar Vivadent), color infiltrated in its pre-sintered phase. Setting aside the temporary Variobase® to be used on another patient, a new Variobase® abutment, with the same gingival and abutment height as that of the temporary, was sandblasted with 50 µm AL2O3 at 50 psi. A methacryloxydecyl dihydrogen phosphate (MDP) containing primer (Monobond plus; Ivoclar vivadent) was applied to the fitting surface of the zirconia crown and the Variobase® for 60 seconds. A self-curing resin cement (Multilink Hybrid Abutment; Ivoclar Vivadent) was manually mixed and loaded onto the fitting surface of the zirconia crown and the Variobase® abutment. Excess cement was removed at the margin using a microbrush before setting the resin cement, and the margin was polished using medium and fine zirconia polishing wheels (Dialite® ZR, Brasseler). The temporary restoration was unscrewed, and the new Variobase® abutment with the cemented definitive crown was then screwed onto the implant at 35 N and the screw hole was sealed with Teflon and composite resin (Fig. 14). Occlusion was then assessed and adjusted in centric and excursive movements. A periapical radiograph was then taken to verify the proper seating of the restoration (Fig. 15).





Follow-up
After 4 months, the patient was recalled for a follow-up evaluation. A periapical radiograph revealed a stable level of crestal bone, exceeding the level of the implant-abutment interface. The interproximal soft tissue (i.e., papillae) was also clinically stable, with no signs of bleeding on probing. A 4-year follow-up clinical examination demonstrated stable levels of soft and hard tissue, further confirmed using a periapical radiograph (Fig. 16).

Discussion
This report proposed utilizing a titanium base abutment as both a temporary and definitive abutment for immediate non-occlusal loading. An advantage of using a ti-base abutment as a temporary abutment is reflected in its design. Compared to prefabricated temporary abutments, these abutments are manufactured with varying gingival heights. The availability of various gingival heights of ti-base abutments allows their seating post-extraction and immediate implant placement without necessitating the removal of proximal crestal bone by a rongeur forceps or bone profiling burs, which would risk further loss of marginal bone during the healing phase. It has been well-established by Tarnow et al. that the presence of interproximal papillae inversely depends on the distance from the base of the contact area to the crest of the bone (Tarnow et al. 1992). Likewise, Salama et al revealed that this association is present in peri-implant tissues (Salama et al. 1998).
Another important design feature of a ti-base abutment is its “platform switching” configuration where it is narrower than the implant diameter. In immediate loading cases, where bone grafts are placed between the fixture surface and the inner wall of the extraction socket, regeneration of bone begins with active bone resorption and formation. It is then followed by osteoconduction and a process known as “creeping substitution” in which all of the graft is replaced with host tissue (Rodríguez et al., 2012). This bone creeping substitution along with the “platform switching” can exceed the implant abutment-interface, limit the loss of crestal bone, and guide the orientation of the mechanically retained periodontal fibers (Tarnow et al. 1992).
The stability of peri-implant health is also affected by the repeated dis/reconnections of the abutment during restorative protocols (Wang et al., 2016). Minimizing disturbances to the healing phase may avoid damaging the connective tissue which would cause the migration of the epithelial attachment with consequent loss of bone, even with an established biological width. The “one abutment one-time” concept is an approach that successfully preserves peri-implant tissues using definitive abutments placed immediately after implant insertion with no intention to remove them at later stages (Tallarico et al. 2018; Koutouzis et al. 2017; Praça et al., 2020; Degidi et al., 2014; Koutouzis et al., 2013). One disadvantage associated with this approach requires the clinician to predict the definitive level of soft tissue and prosthetic finish line at the surgical stage, whereas, when using ti-base abutments for temporization, the clinician is still able to fabricate the final prosthesis according to the healed soft tissue. Nevertheless, while the proposed concept still necessitates the removal of the abutment at the implant position registration phase, the temporary and definitive abutments remain identical, which reduces the risk of altering the peri-implant tissues. In a recent case report, the concept of “socket sealing abutments” was applied using digitally customized titanium bases that preserve peri-implant tissues at grafted sites (Finelle et al., 2017).This technique was suggested in cases of immediate implant placement where implant loading is not advocated (Finelle et al., 2021; Lilet et al., 2022). However, these attempts still do not meet the clinical efficiency and chairside time-saving advantages of prefabricated provisionals prepared extra-orally onto ti-bases and thereafter immediately loading the implants with a full anatomical prosthesis.
Since titanium bases were initially designed to be compatible with CAD/CAM technology (Al-Thobity et al., 2021), a fully guided surgical protocol followed by a fully digital prosthetic workflow permits clinicians to design and mill accurately fitting PMMA provisional protheses that do not require chairside relining and are cemented extra-orally onto the abutment. Furthermore, a fully digital workflow also preserves peri-implant soft tissues as the clinician no longer uses a conventional impression technique in which an impression coping, sometimes of a diameter wider than that of the healing abutment, is used. Accordingly, the initial supracrestal tissue attachment established during the healing phase is well-maintained, and the emergence profile created by the immediate provisional restoration is only registered with an intraoral scanner.
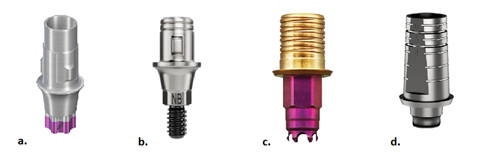
Similar to other commercially available ti-base abutments, the Variobase® is designed with “cams”, i.e. positive modifications or horizontal retention sleeves, to increase the cementable surface area and provide a locking anti-rotational feature for retaining the definitive ceramic superstructure. Other ti-base abutments are designed with negative modifications or retention grooves to retain restorations as demonstrated in figure 17. Such features have proven to adequately retain monolithic material including zirconia, lithium disilicate, and PMMA (Lilet et al., 2022). In this case report, the four Variobase® “cams” provided an adequate retentive role of the provisional crown, excluding the need to recement the relined provisional using temporary cement. Another prosthetic advantage is the possibility of correcting implant angulation. Recently, ti-base abutments with the concept of an angled screw channel have been introduced to correct buccally or labially angled implants, with an angulation correction ranging between 0 and 30 degrees to the implant’s long axis (Anitua et al., 2020). The widely open screw channel within the ti-base abutment is designed to be accessed at an angle, allowing the prosthetic screw to be tightened using specifically designed angled screwdrivers. For example, in anterior areas where implants may be positioned too far labially due to the lack of buccal bone, using a temporary abutment would result in an aesthetically unpleasant provisional restoration where the screw hole cannot be relocated lingually.
Nevertheless, a limitation associated with the proposed protocol is the unavailability of varying gingival and abutment heights of non-engaging ti-base abutments, which may limit their use in cases of immediate bridge temporization. In such cases, multi-unit screw-retained abutments which offer various gingival heights are used instead with their cylindrical temporary coping to fabricate an immediate provisional bridge.
Conclusion
The use of ti-base abutments as a temporary and definitive abutment in immediate loading cases provides several advantages that include preserving peri-implant tissues, undergoing a full-digital workflow, and reducing chairside time. Nevertheless, the outcomes need to be further investigated in well-designed controlled clinical trials that assess quantitative and qualitative clinical factors when using ti-base abutments. Manufacturers should also introducetitanium base design enhancements, such as providing a wider variety of gingival and abutment heights, to extend their application into immediate loading protocols.