Introduction
Dental implants have become a common and reliable method for replacing missing teeth, improving chewing function, and enhancing oral health-related quality of life (Buser, Sennerby and De Bruyn 2017, Duong, Roccuzzo et al. 2022, Roccuzzo, Imber et al. 2022). However, in addition to the functional benefits, there has been increasing attention to the esthetic and biological aspects of the peri-implant soft tissue seal and understanding the biology of the soft tissues surrounding dental implants is of great clinical importance (Sculean, Gruber and Bosshardt 2014, Schwarz and Ramanauskaite 2022).
Peri-implant mucosa vs. gingiva
Distinctions between peri-implant soft tissues and gingiva are evident histologically and histomorphometrically. There are several reasons to differentiate between mucosa around implants and gingiva around teeth:
- Parodontal fibers insert into tooth cementum, while peri-implant connective tissue fibers run parallel to the implant/abutment surface (Berglundh, Lindhe et al. 1991, Listgarten, Lang et al. 1991).
- Peri-implant connective tissue (CT) has fewer fibroblasts and a higher proportion of collagen fibers (similar to scar tissue) (Berglundh, Lindhe et al. 1991, Moon, Berglundh et al. 1999).
- Gingiva around natural teeth has a higher vascular content than peri-implant soft tissue (Berglundh, Lindhe et al. 1994).
Non-elastic collagen fibers in underlying CT seem responsible for the presence of keratinized tissue (gingiva or mucosa). Whereby elastic fibers are a common finding in CT below a non-keratinized epithelium. Around natural teeth, even after complete surgical removal, a narrow band of gingiva is reestablished due to the presence of non-elastic fibers in the periodontal space (Karring, Østergaard and Löe 1971). In contrast, implants can be surrounded by either keratinized mucosa (KM) or movable alveolar mucosa. Studies suggest gingival CT can induce keratinized epithelium formation (Karring, Lang and Löe 1975). Despite keratinization of peri-implant mucosa, it may not be attached to underlying peri-implant bone, especially if the transition between keratinized and non-keratinized mucosa lies coronal to the bone.
The peri-implant phenotype
The peri-implant phenotype encompasses the observable characteristics of the tissues surrounding osseointegrated implants and includes both soft tissue and osseous components (Avila-Ortiz, Gonzalez-Martin et al. 2020). Soft tissue aspects include keratinized tissue (KT) width, mucosal thickness, and supracrestal tissue height. KT width refers to the distance of the soft tissue margin to the mucogingival junction and can affect peri-implant health and esthetics. Mucosal thickness, the horizontal dimension of soft tissue, affects esthetic outcomes and may require surgical intervention for augmentation. Supracrestal tissue height, the vertical dimension of soft tissue, influences bone remodeling and is essential for predictable implant therapy outcomes (Avila-Ortiz, Gonzalez-Martin et al. 2020).
Keratinized mucosa around implants
The importance of keratinized tissue (KT) surrounding dental implants has been debated for decades. While some studies suggest that soft tissue quality has little impact on implant survival, others emphasize the potential benefits of adequate KT for plaque control and peri-implant health. Recent meta-analyses (Wu, Qu et al. 2015, Ramanauskaite, Schwarz and Sader 2022) have highlighted significant associations between lack of KT and increased plaque accumulation, inflammation, and attachment loss. Moreover, the absence of KT may lead to discomfort during brushing, impacting patients’ ability to maintain proper oral hygiene (Kungsadalpipob, Supanimitkul et al. 2020). Inflammatory responses around implants without KT are more pronounced than those around teeth. Consequently, maintaining a CT similar to that around teeth is desirable for implant sites, ensuring a biological seal and long-term peri-implant health. Understanding the specificity of soft tissue characteristics and responses around implants compared to teeth is essential for optimizing treatment outcomes and maintaining peri-implant health.
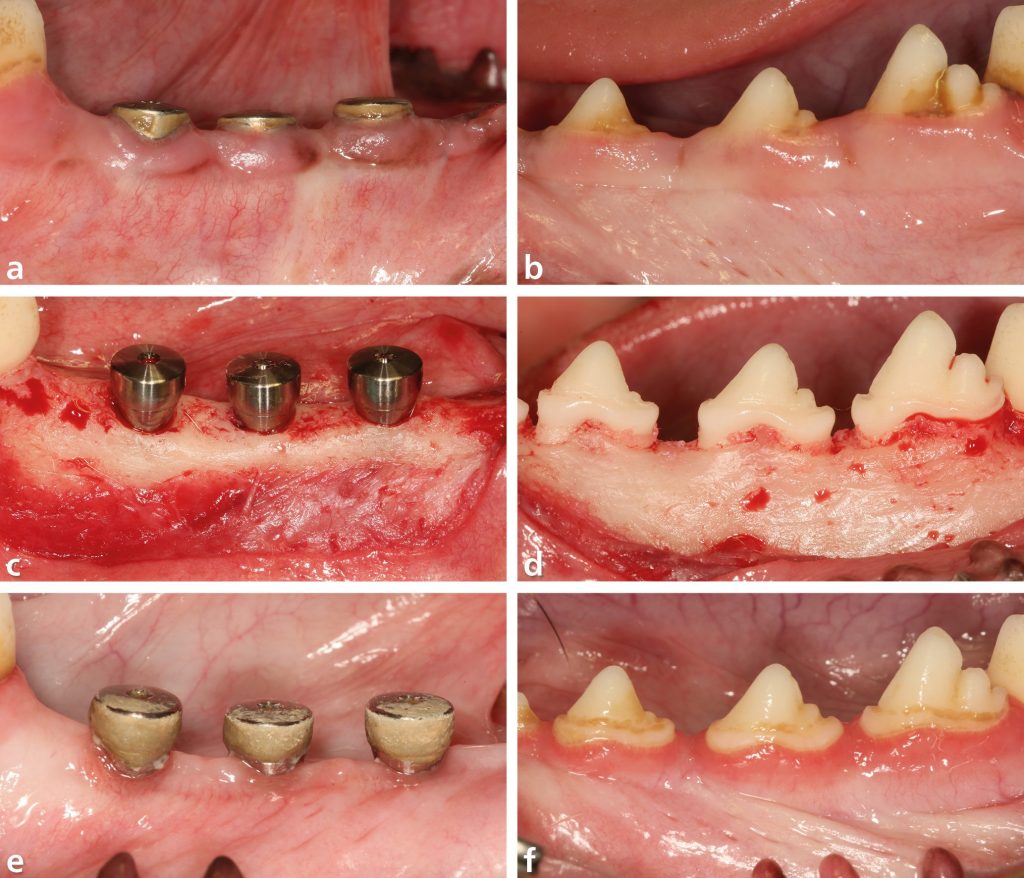
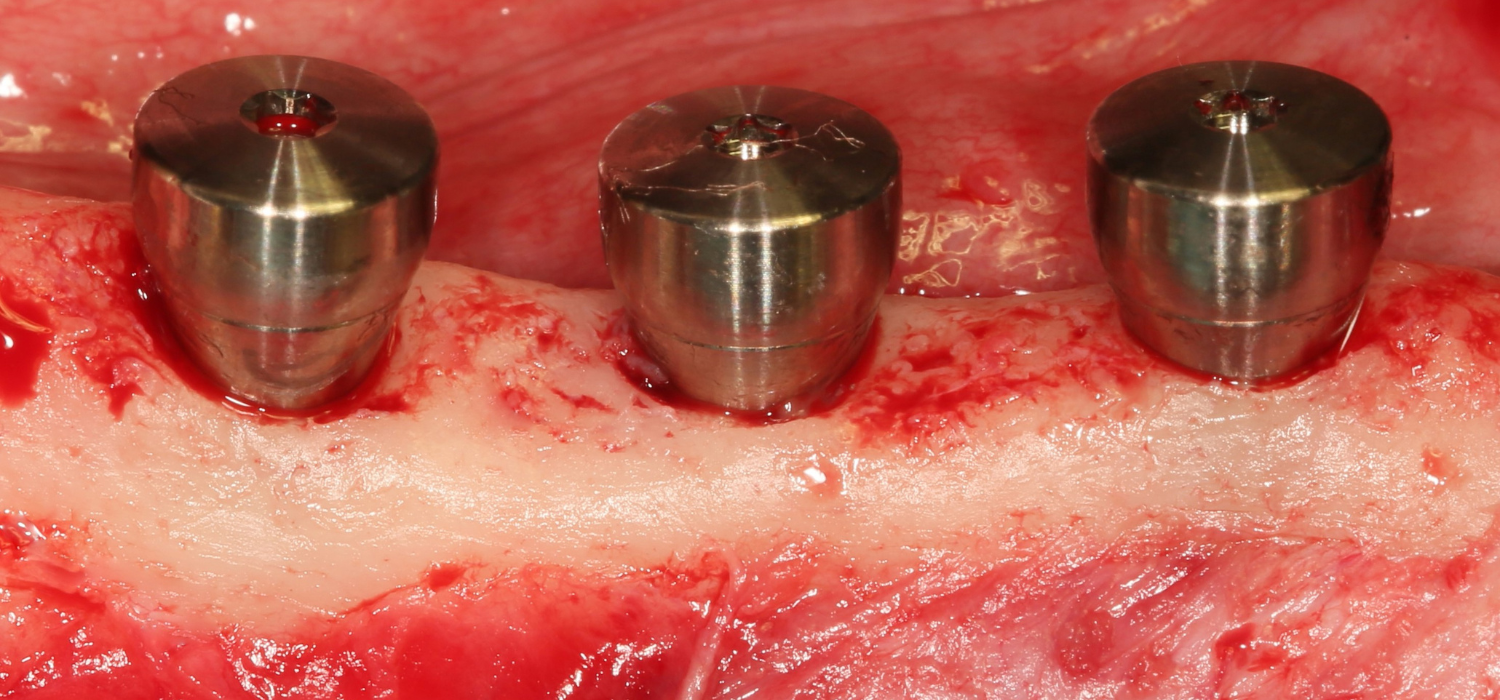
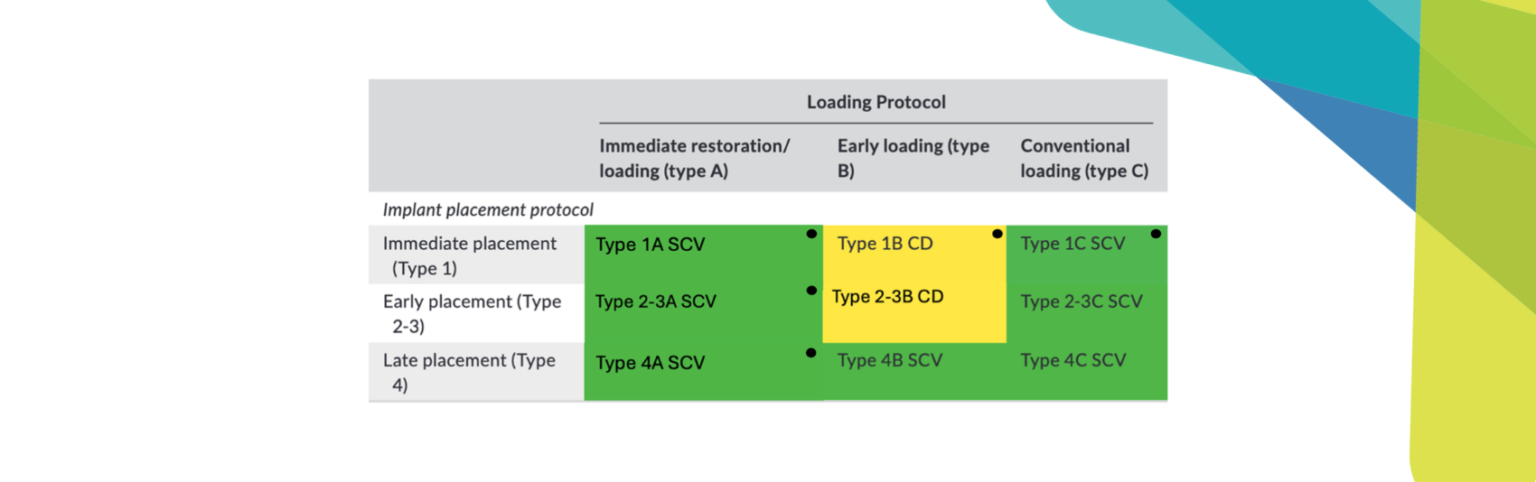
Recently, the findings of a preclinical-animal study of Imber and co-workers (Imber, Roccuzzo et al. 2023) provide valuable insights into the biological processes involved in soft tissue regeneration around dental implants compared to natural teeth. After osseointegration, the entire keratinized tissue (KT) was removed on dental implants (Figs. 1a, 1c) and on contralateral teeth (Figs.1b, 1d), and the tissues were allowed to heal for three months (Figs. 1e, 1f). At tooth sites, spontaneous regeneration of the dento-gingival unit was evident, characterized by the formation of masticatory mucosa (Figs. 2e, 2f, 2g, 2h). Keratinization was observed on both buccal and lingual aspects, with the presence of CT and absence of elastic fibers below the keratinized epithelium (Fig. 3b). In contrast, implant sites exhibited characteristics of alveolar mucosa, with the absence of KT (Figs. 2a, 2b, 2c, 2d). Elastic fibers were abundant in the CT near and far from the mucosal margin, indicating differences in tissue composition compared to tooth sites (Fig. 3a). Overall, histological analysis confirmed differences in tissue characteristics between tooth and implant sites, highlighting the influence of adjacent masticatory mucosa on soft tissue regeneration. Histomorphometric analysis further quantified differences in tissue dimensions between tooth and implant sites. The height of the KT was significantly higher at teeth compared to implants, with no KT detected at any implant site. Similarly, the height of the junctional epithelium and CT was greater at teeth, resulting in a larger supracrestal tissue height compared to implants. Vertical soft tissue loss (gingival recession or soft tissue dehiscence) was more pronounced at implant sites, indicating a more significant challenge to the soft tissue barrier. The results emphasize the importance of maintaining health around implants to prevent complications such as peri-implantitis and soft tissue dehiscence. Consequently, clinical procedures should aim to preserve keratinized tissue or enhance keratinized tissue with grafting procedures to support soft tissue health and minimize complications associated with implant therapy.
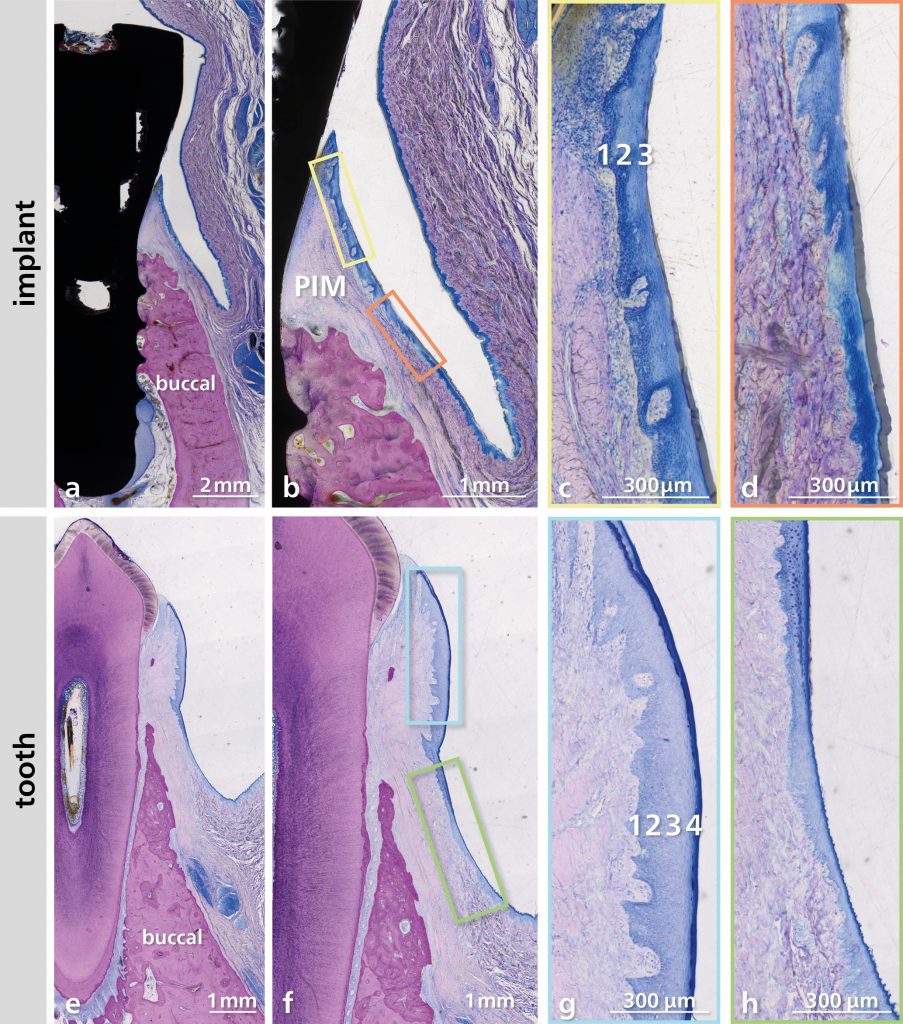
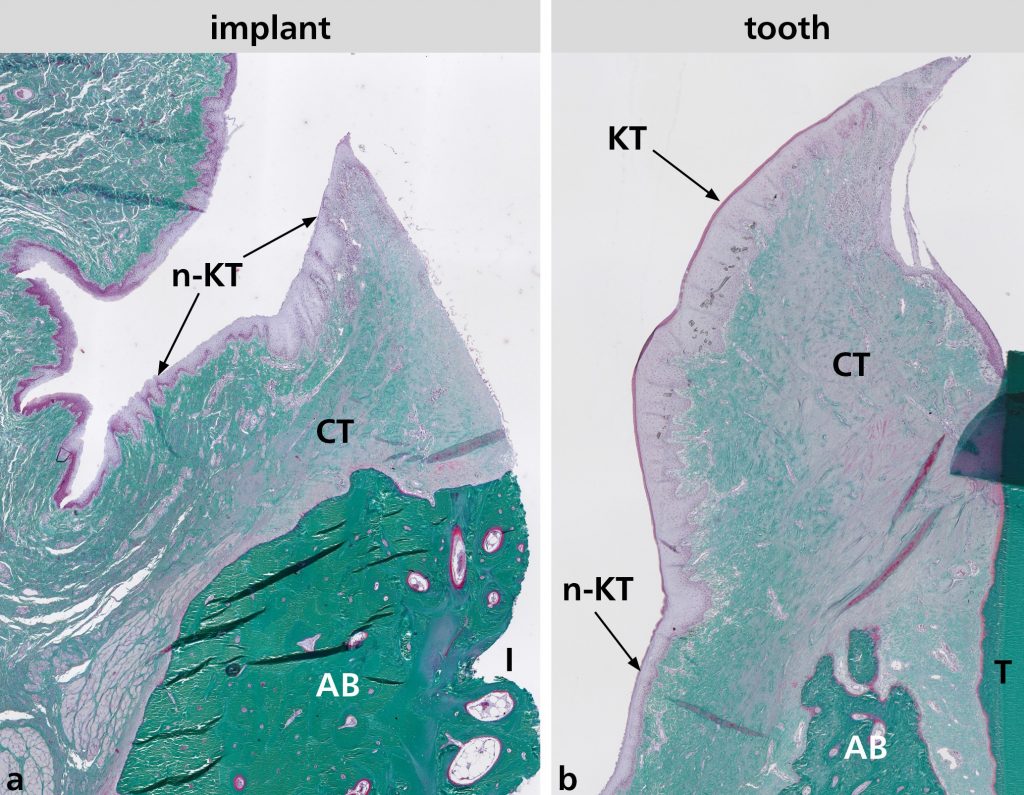
and near the gingival margin at tooth site (b). AB, alveolar bone; CT, connective tissue; I, Implant; KT, keratinized tissue; n-KT, non-keratinized tissue; T, tooth. Staining: resorcin-fuchsin and Goldner.
Soft tissue grafting
Soft tissue grafting procedures around dental implants encompass a variety of surgical techniques tailored to meet specific patient needs and clinical challenges. The selection of the appropriate surgical approach depends on factors such as the extent of soft tissue deficiency, the desired outcome, and the clinician’s expertise. Common surgical techniques for soft tissue augmentation include vestibuloplasty, tunneling techniques, coronally advanced flaps, and guided bone regeneration (GBR) with simultaneous soft tissue grafting. Optimal times for augmentation include before or after implant placement and at healing abutment connection (Mancini, Simeone et al. 2023). Factors like operator experience, implant position, and patient expectations are crucial for successful outcomes and complication prevention (Mancini, Simeone et al. 2023). Several types of soft tissue grafts are used in implant dentistry, including autogenous grafts, allografts, xenografts, and alloplastic materials (Thoma, Buranawat et al. 2014, Cairo, Barbato et al. 2019). Allografts, xenografts, and alloplastic materials provide alternatives to autogenous grafts with reduced morbidity and surgical complexity. Nevertheless, autogenous grafts, harvested from the patient’s own tissues, remain the gold standard due to their excellent biocompatibility, minimal risk of immunogenicity, and superior tissue integration (Thoma, Buranawat et al. 2014, Cairo, Barbato et al. 2019). Common autogenous grafts used for soft tissue augmentation around implants include connective tissue grafts (CTG) and free gingival grafts (FGG) harvested from the palate or tuberosity region.
In clinical practice, careful monitoring of peri-implant soft tissue conditions is paramount. Consideration of FGG to augment KT width or CTG to enhance the thickness of the soft tissues around implants may be warranted in cases where soft tissue manipulation during implant placement is challenging or when enhancing patient oral hygiene is essential. Through a comprehensive understanding of grafting principles, meticulous surgical execution, and ongoing research and innovation, clinicians can effectively manage peri-implant soft tissue challenges and ensure the success of implant therapy for their patients.
Conclusion
Understanding the characteristics of peri-implant soft tissues, their importance for implant success, and the various procedures available for managing soft tissue deficiencies are crucial for optimizing treatment outcomes and maintaining peri-implant health.