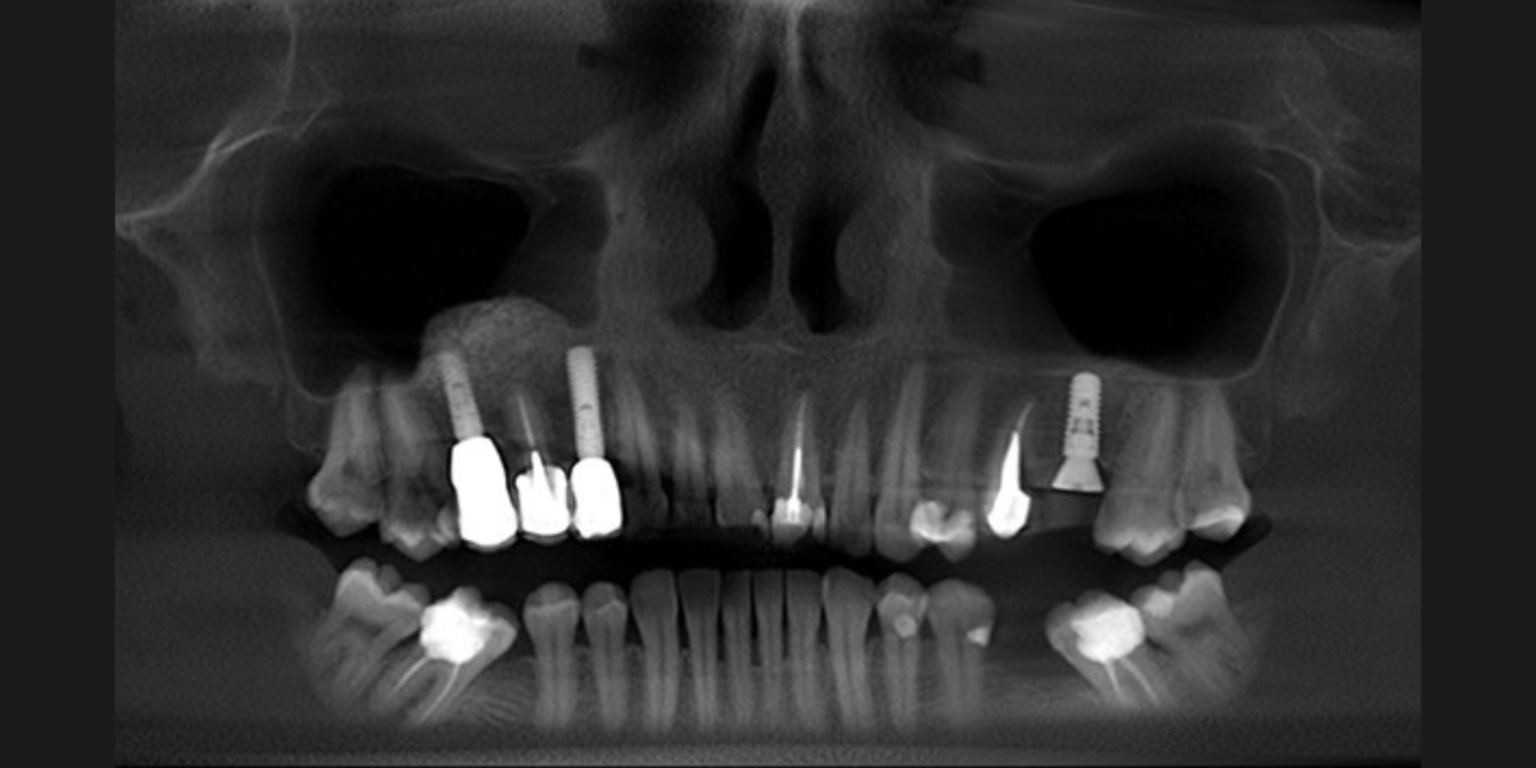
One of our biggest challenges in implant dentistry is managing patient expectations and providing long-term patient-centered solutions. Patients expect dental implants to look and function like teeth, but we know as implantologists that due to anatomical variance differences will always remain.
A dental implant lacks a periodontal ligament and is a functionally ankylosed tooth. This makes it susceptible to mechanical and technical complications particularly in individuals with heavy occlusal forces such as bruxists.
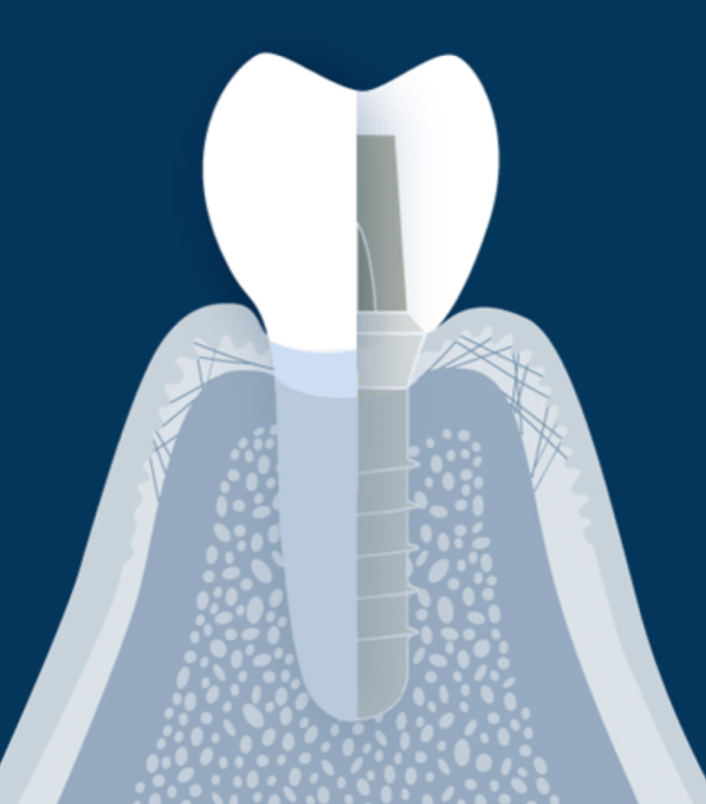
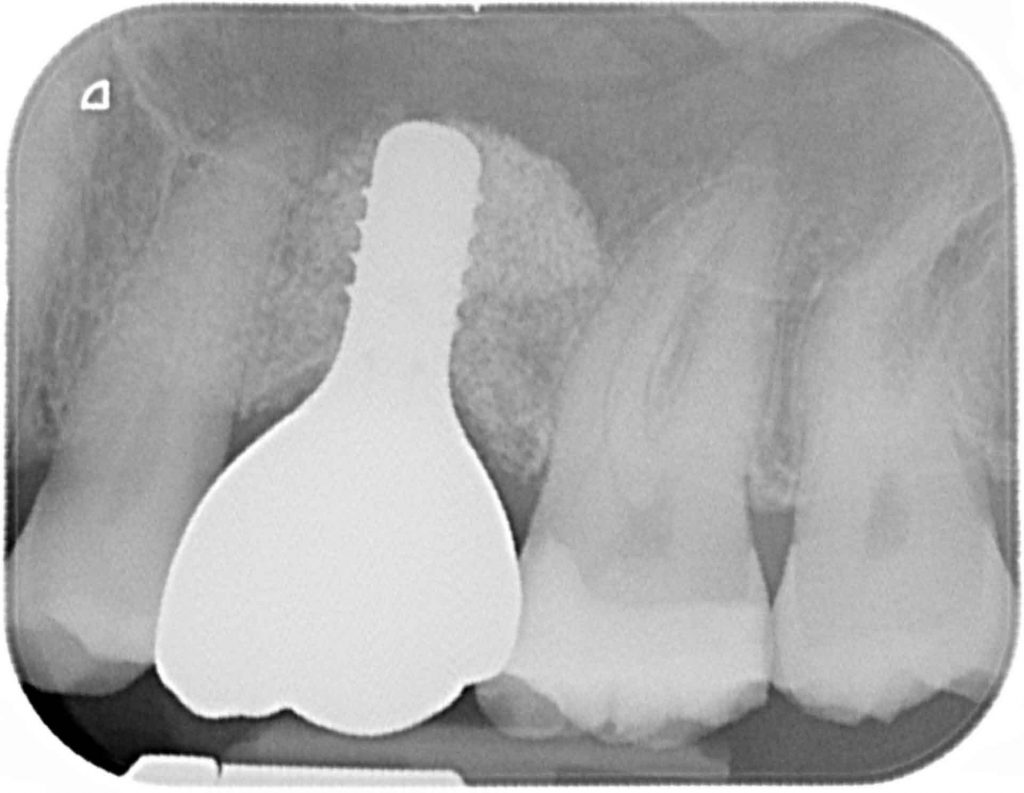
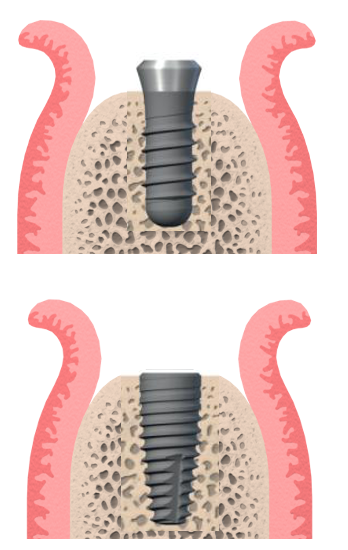
Due to the lack of root surface cementum and a periodontal fiber attachment, dental implants have an innate risk of direct bacterial attack on the underlying alveolar bone support. This means bacteria can elicit a very quick host immune response that can cause rapid and severe bone loss around an implant in a process called peri-implantitis. Implant design can help to mitigate this by moving the bacterial harboring regions – i.e., the connection between the implant fixture and the restorative interface away from the all-important crestal bone.
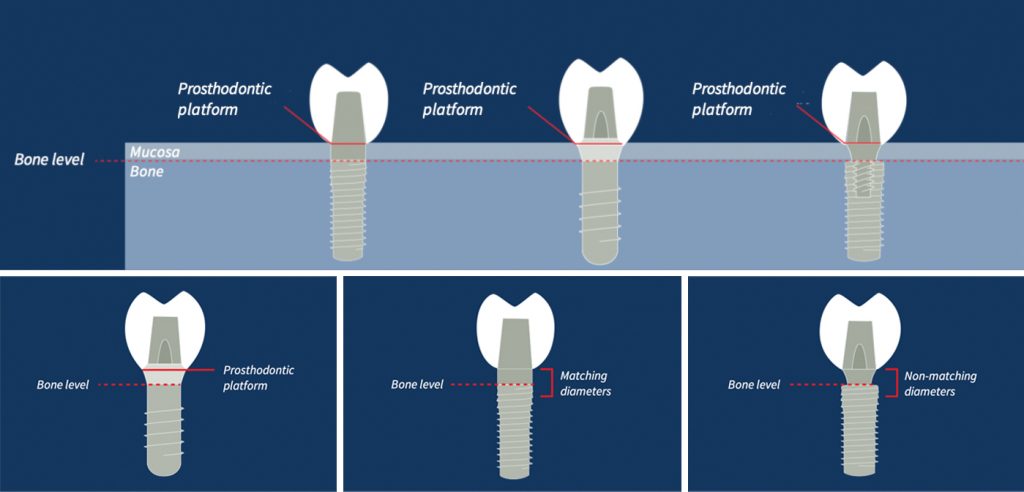
Hence, implant restorative design to prevent these biological risks can help to maintain alveolar bone and the supporting structures for as long as possible. This has been the principle behind the long-term success of the soft tissue level implant. The tight connective tissue cuff around the implant fixture head is critical to success.
The concept of biologic width
Gingival biotype and biologic width have been described in the literature at length. Biologic width was very clearly described by Gargiulo et al. (1995) and shows the constituents to soft tissue anatomy. The epithelium and connective tissue form a physiological seal coronal to the bone. The connective tissue is fairly consistent, but the epithelium can vary in thickness – similarly with gingival biotype.
Thick gingival biotypes tend to be more biologically resistant to bacterial invasion than thinner biotypes and have a reduced risk of gingival recession.
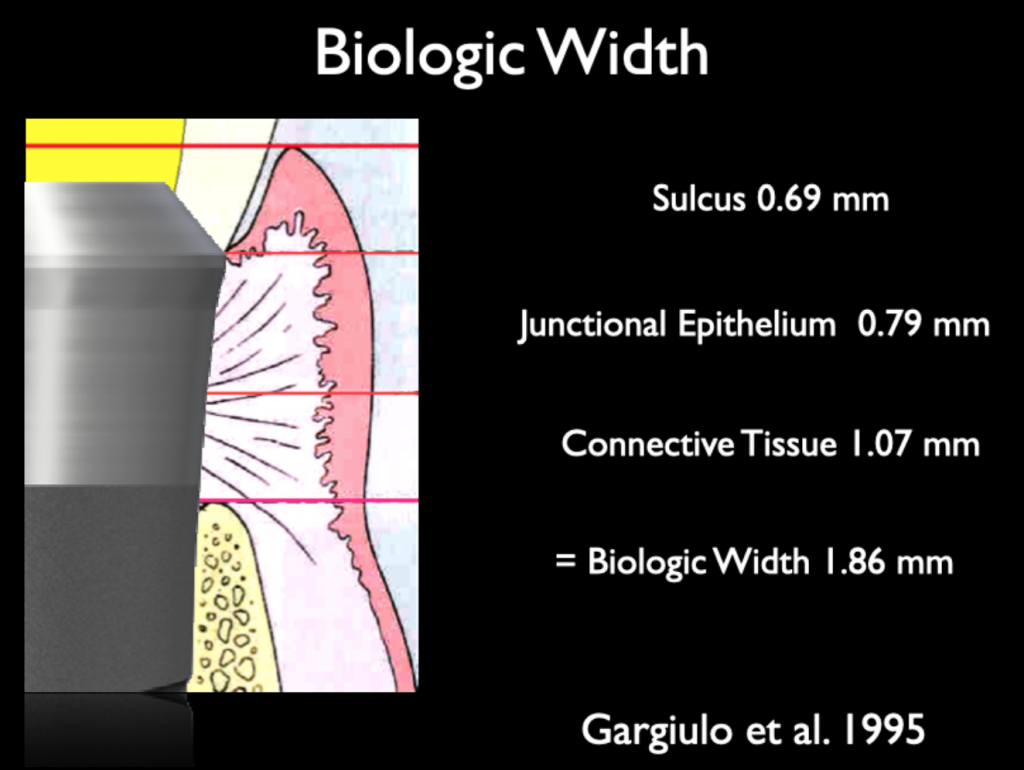
If we can understand the biological width ratios and their importance to implant dentistry, it means we can protect our patients’ restorations from significant bacterial attack over many years. This is the fundamental principle to the long-term success of the Straumann tissue level implant.
Clinical restorative importance
Tissue level implants are difficult to place initially – there is much less “restorative” flexibility from having a supra-crestal restorative interface. However, the long-term benefits of this connection far outweigh the learning curve difficulties. Once the implant is in situ, the impression technique is relatively straightforward with minimal management of the soft tissue required, which makes it an excellent choice for the young or inexperienced clinician in the non-esthetic zone.
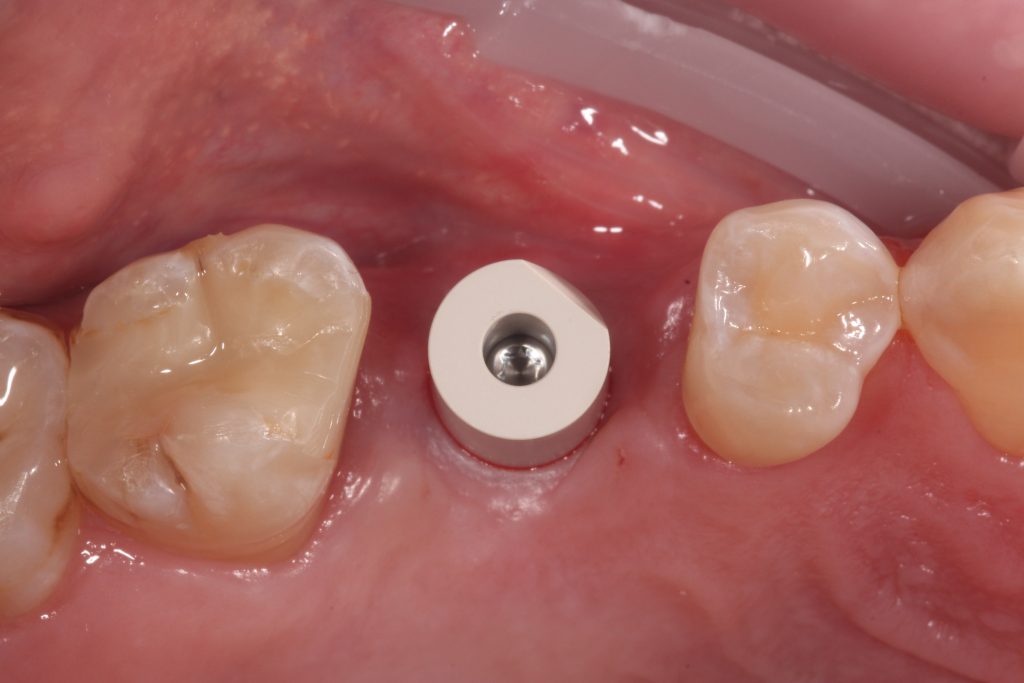
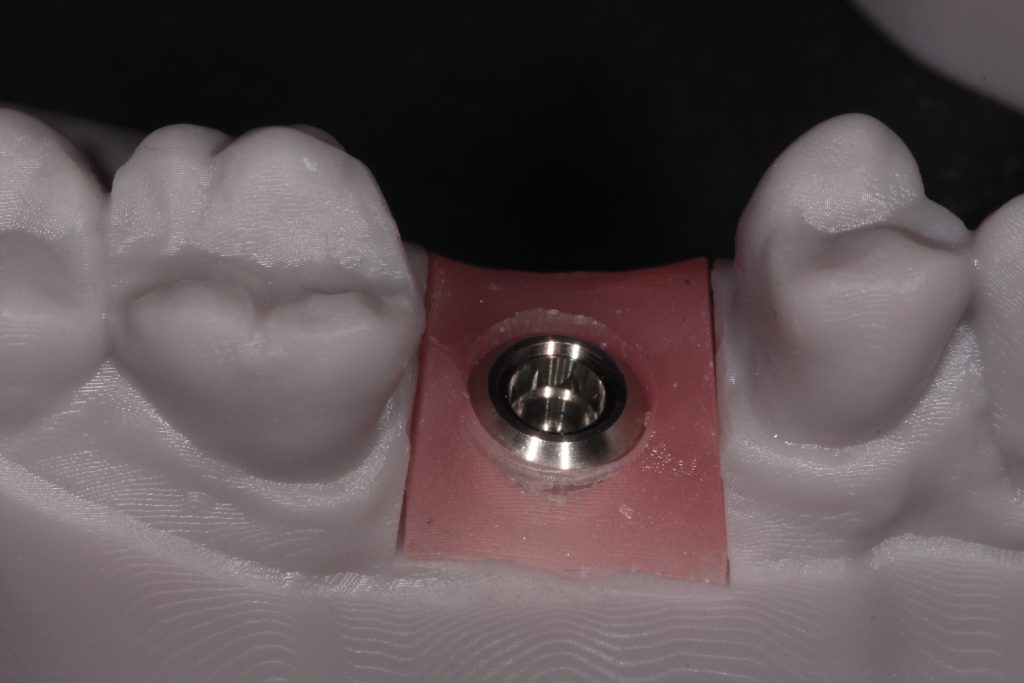
For long term gingival health, we require smooth, even emergence profiles that allow a sufficient “cuff” of keratinized mucosa at the point where the crown transitions into the implant fixture. With bone level implants this emergence profile can be determined by both the clinician and the dental laboratory working together – but there are lots of opportunities for this to be miscommunicated and subsequently over or under built which can cause many different issues with maintaining gum health and critically bone levels around the implants.
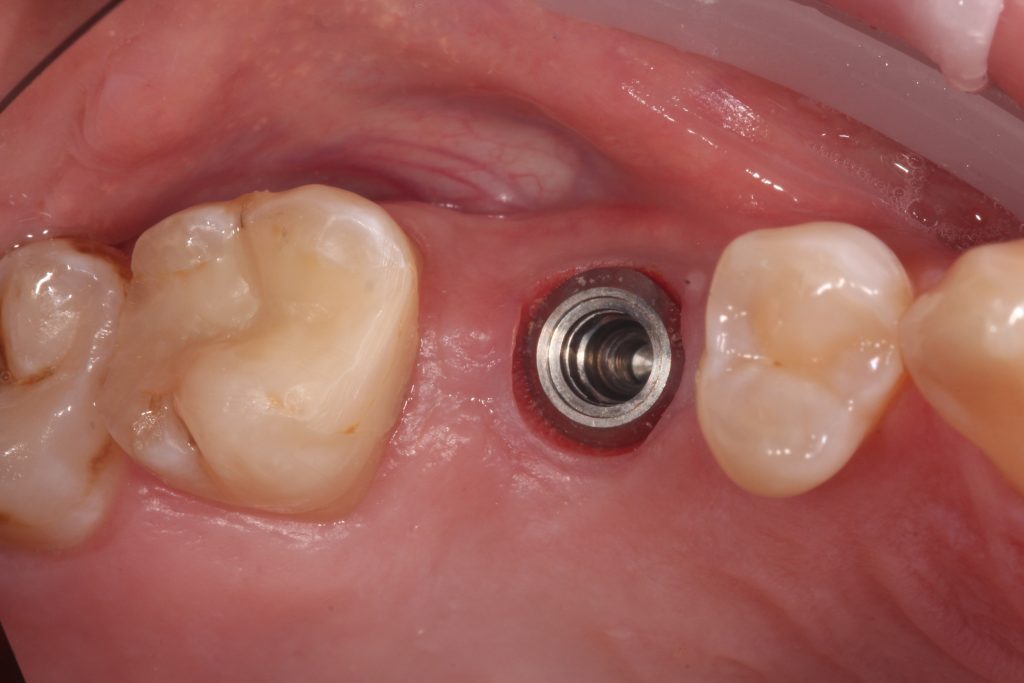
Tissue level Implants have a largely predetermined emergence profile when placed correctly surgically. Not only does this mean that the restorative stages are very straightforward, but it also crucially means that the weakest point in the system – the interface between the implant abutment and the implant fixture – are supragingival. This interface is the point at which micro-movement of the superstructure can cause bacterial contamination and inflammation and potential bone loss. But of course if this margin is supracrestal, the actual bacterial contamination is minimal, and this is the success behind the long term successful outcomes of these implants.
Of course having a fixed emergence profile does not allow for true esthetic modification. Whilst there are some excellent clinicians around the world who are able to use the tissue level implant in the esthetic zone, we mere mortals combine a mixture of tissue level implants in the non-esthetic zone and bone level implants in the esthetic zone for their restorative flexibility.
In the UK and Ireland, as part of the Foundation in Implant Dentistry for new clinicians to implant dentistry, we teach surgical placement and restoration of tissue level implants in the non-esthetic zone. Whilst clinicians sometimes feel they want to learn about bone level implants too, they often acknowledge a year or so after attending the program that learning the correct placement of the tissue level implant according to biological principles is more difficult initially but enables them to go on and place a bone level implant more precisely.
Accurate implant placement is essential to ensuring their restorations have smooth and even emergence profiles creating highly cleansable fixed and removable restorations.
Ease of tissue level prosthodontics
Having a fixed emergence profile to capture either at gingival level or supragingival should be the most straightforward crown and bridge impression technique in dentistry. Complications to this can occur when implant fixtures are buried too deep or there are thick gingival tissues around the machined collar of the implant. At this stage sometimes a scalpel with a small sickle shaped blade or a tissue punch can be used to ease the placement of components.
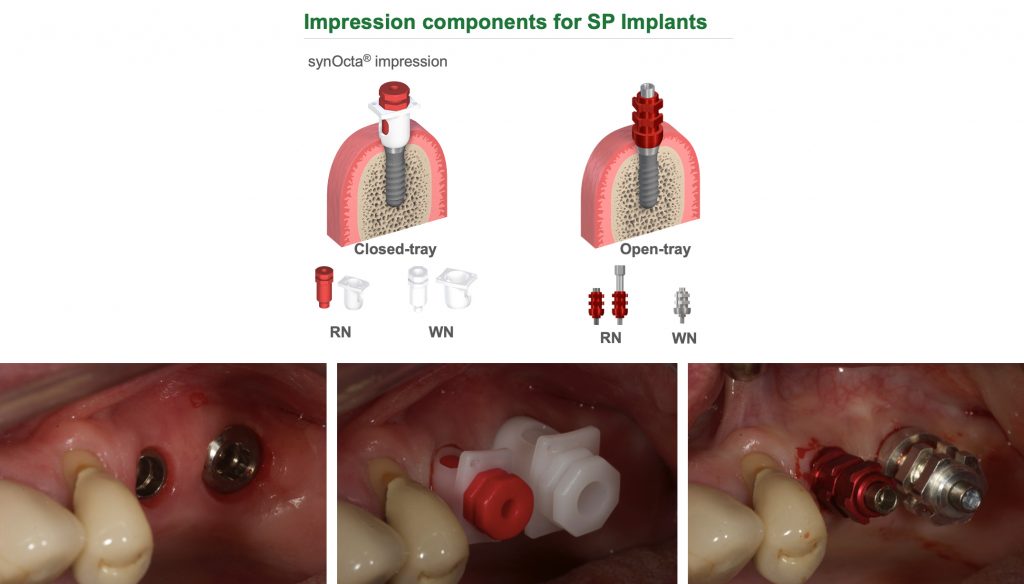
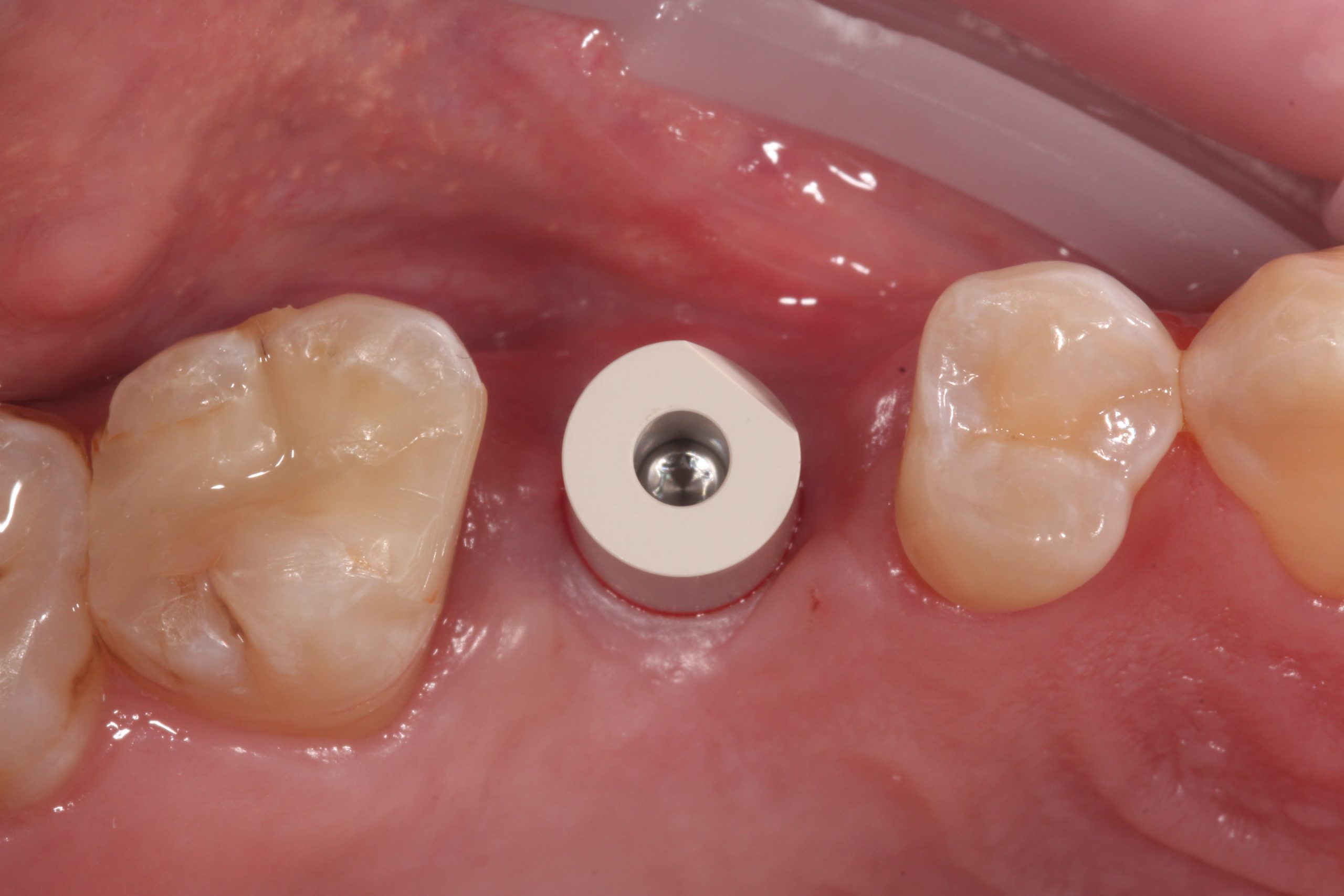
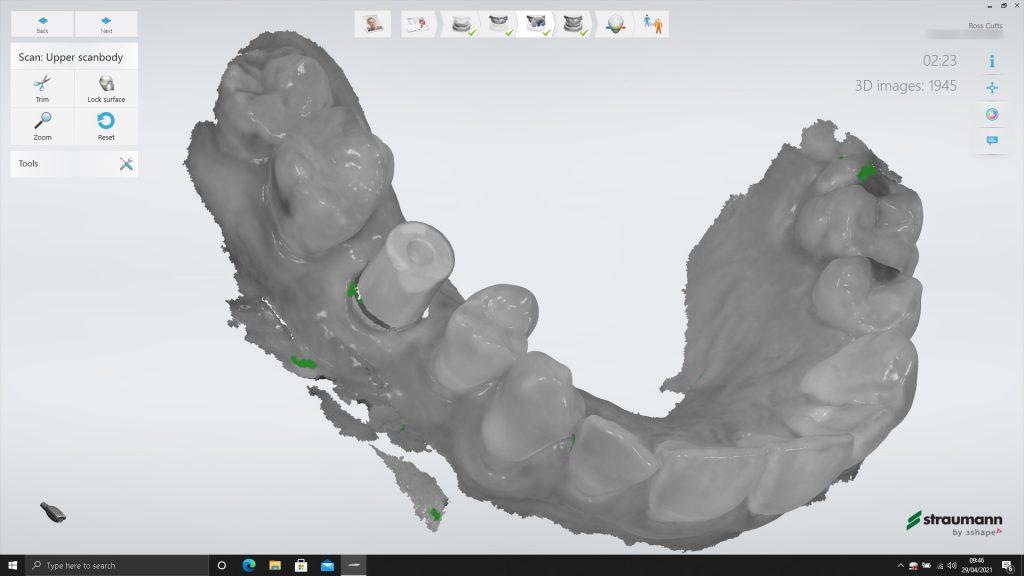
With the latest technologies available, intraoral scanning of a tissue level scanbody is the easiest crown and bridge impression I take. The margins of the restoration are predetermined and, provided the scanbody is correctly seated without hard or soft tissue impingement, we can achieve highly accurate transfer of the implant fixture position in relation to the adjacent and surrounding teeth.
Conclusion
Whilst there is a current trend towards immediacy in implant dentistry and consumer-driven protocols, I think we would do well to remember the long-term success story that the tissue level implant has been.
It continues to be my “workhorse” implant in the non-esthetic zone because it is a very straightforward restoration to manufacture and maintain when placed correctly surgically according to the biological principles touched upon earlier.
Patients are able to maintain these simple restorations well over time, due to the supra/gingival nature of the restorative interface.
When clinicians are coerced into immediate implant delivery often due to marketing from implant companies or patient pressure – the bone level implants become positioned deeper and in less favorable surgical positions for ease of restorability. The definitive restorations become thicker and bulkier in the transition zone through the gingiva, increasing the likelihood of plaque stagnation zones at the crestal bone level. This can often be made worse by choosing a cement-retained restoration (for ease of laboratory fabrication) resulting in cement inclusion with these very deep and bulky restorations.
CLINICAL keys to success with tissue level implants:
- If you are a less experienced implantologist, find a suitable ITI mentor – don’t start this journey alone! The ITI is a great family
- Accurately plan and execute the surgical placement of the tissue level implant – it is fundamental to long term success
- Work closely and develop a close relationship with your prosthodontic technician/s – discuss your restoration goals – this may well affect your surgical placement
- List the non-negotiable design aspects to your restorations
- Screw-retained restorations – unless the screw access hole exits through a cusp tip – (but you can now discuss angle correction solutions)
- Cleansability interproximally – tight but smooth and long contact points
- Smooth emergence profiles – no ridge laps!
- Correct occlusal design principles – generally minimal lateral guidance/nil interferences and light hold with shimstock in centric
- Original components! Often forgotten to make more economic solutions – insist on original components for accuracy of the fit
- Review the health of your implants and look at what you want for your family members as an implant solution to be successful (not just survive) over many years in function
More from the author:
More on the topic: