Introduction
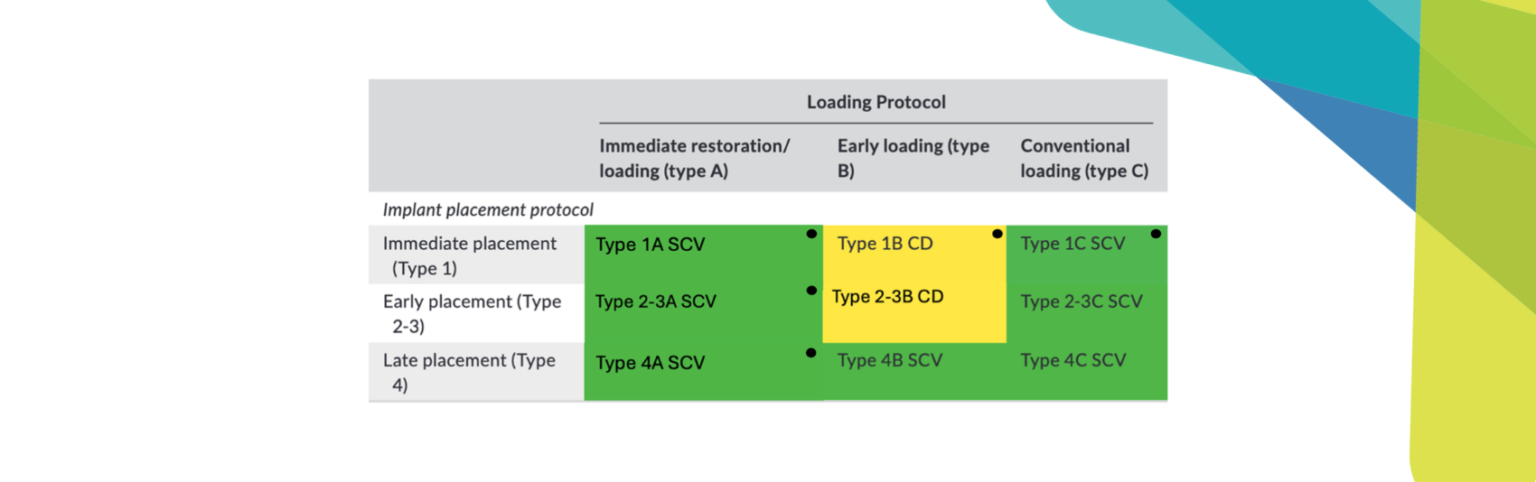
Over the past decades and especially in recent years, dental implantology has become established in everyday clinical practice worldwide. To achieve satisfactory results, various factors, such as hard and soft tissue quality, availability, and prosthetic prerequisites, should be carefully evaluated before surgery (Morton 2017).
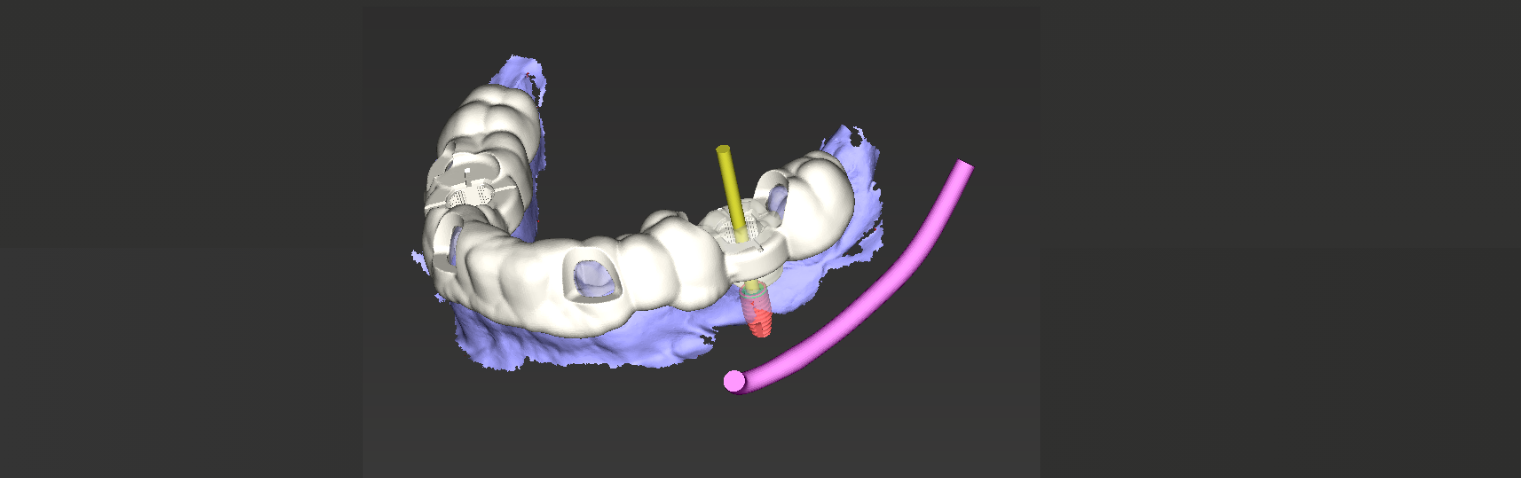
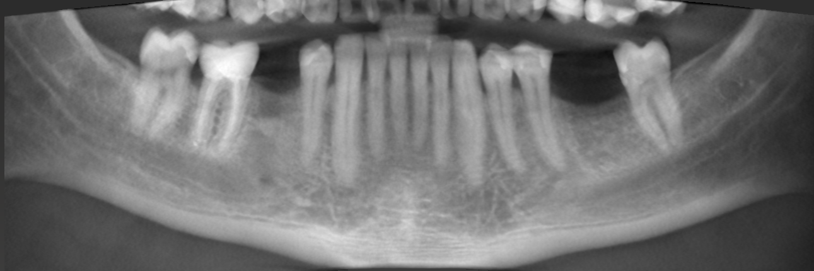
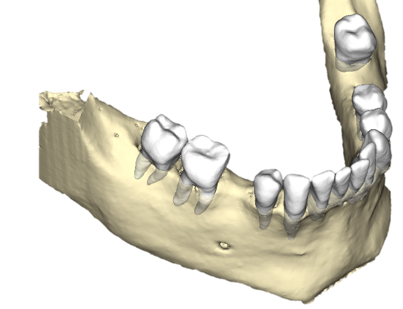
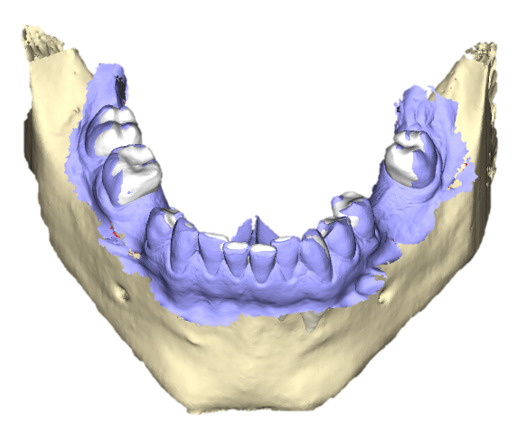
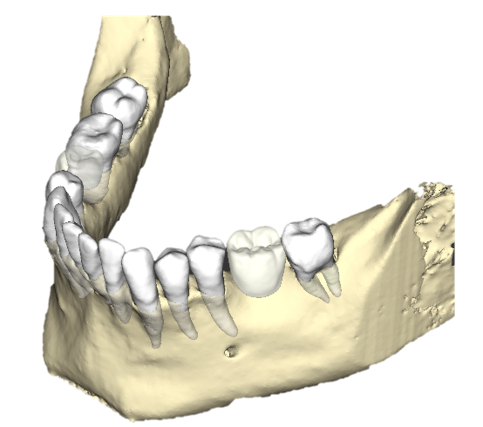
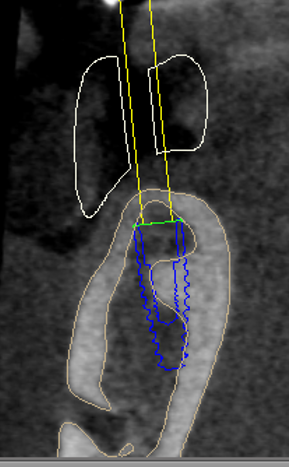
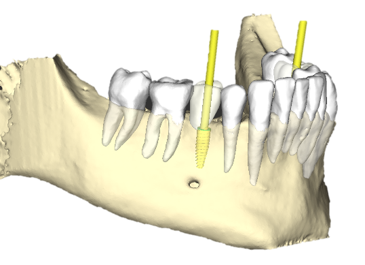
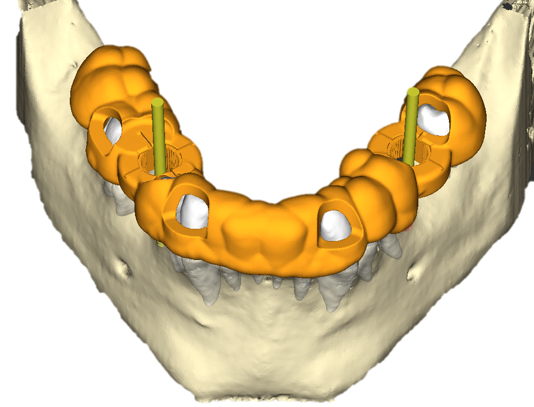
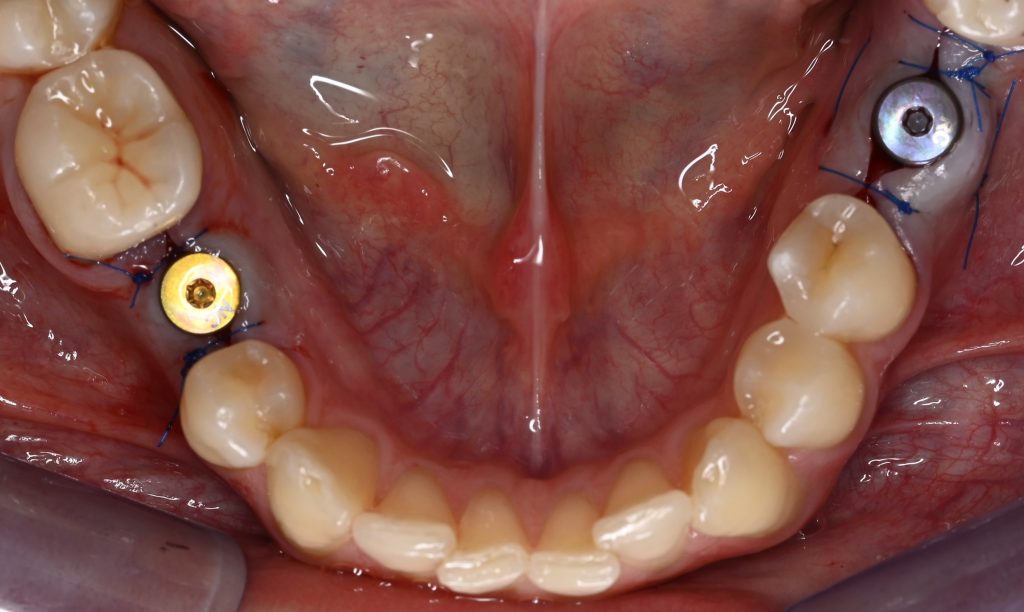
Prosthetically driven backward planning, where the desired restorations guide the surgical phase, has changed the approach to current implant dentistry. In addition, due to technological advancements, powerful tools for ideal virtual implant planning and accurate implant installation are available. Resources such as intraoral scanners (IOS) and cone-beam computed tomography (CBCT) devices allow the creation of virtual three-dimensional (3D) patient models using digital datasets in Standard Tessellation Language (STL) and Digital Imaging and Communications in Medicine (DICOM) formats. These datasets are aligned with the prosthetic set-up using dedicated implant planning software in a process named registration.
An accurate registration of the different datasets is essential to avoid the malposition of implants (Flugge et al. 2017). Today, users are supported by artificial intelligence (AI) during registration to automate and accelerate the process (Ntovas et al. 2024). However, with image artifact sources such as highly opaque metals, additional manual superimposition is still required. After ideal implant planning, surgical guides are designed and subsequently manufactured, usually by milling or 3D printing ( Revilla-Leon et al. 2020). In guided approaches, the drilling protocol defined by the manufacturer is applied to prepare the surgical site and install the implant.
Benefits
Virtual planning
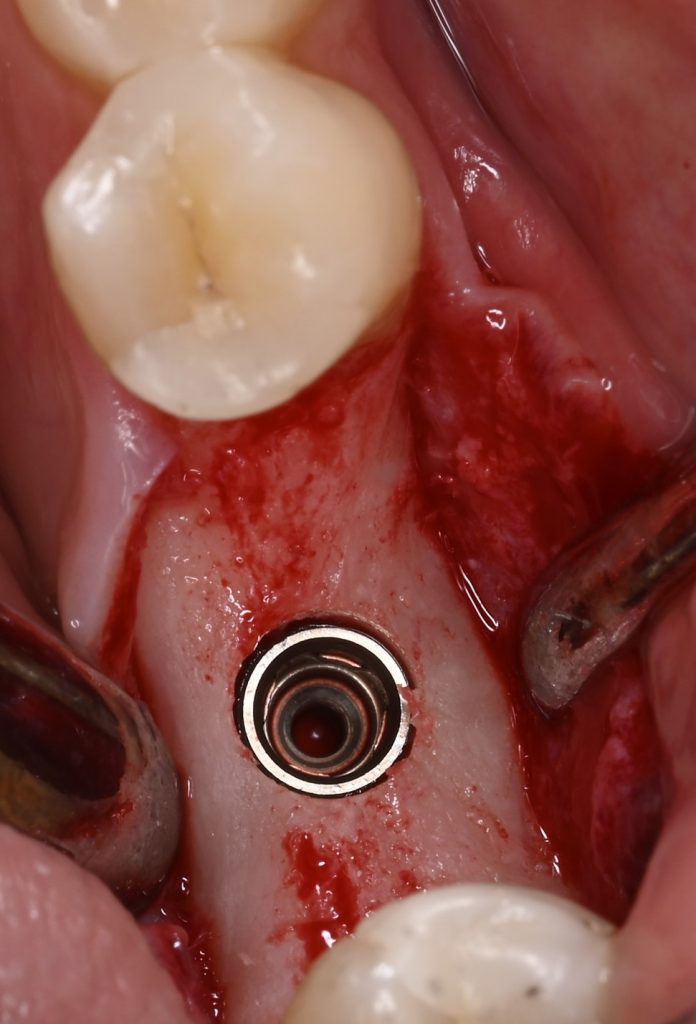
Current research indicates that static computer-assisted implant surgery (sCAIS) is more predictable and accurate than freehand implant placement, as the surgical template guides the drilling and implant installation sequence to the virtually planned position ( Schneider et al. 2021). Accuracy is paramount to avoid damaging critical anatomical structures, such as adjacent roots, nerves, vessels, and sinuses, and to improve implant primary stability.
Moreover, in selected cases virtual implant planning may reduce or even eliminate the need for hard-tissue augmentation procedures by selecting shorter or inclined implants.


Communication
Digital planning software allows for optimal visualization of the clinical case by creating a 3D virtual patient. This facilitates communication between clinicians, dental labs, and patients. Moreover, by connecting implant planning systems with computer-aided design/manufacturing (CAD/CAM) software or systems for virtual wax-up/set-up design, the potential for communication within the team can be further increased. This results in a more effective and faster work routine.
Surgical time
With sCAIS, the time needed to perform surgeries can be reduced compared to conventional techniques. This results in increased efficiency for clinicians and shorter surgical operations for patients, an advantage, especially for elderly patients or those taking specific medications such as anticoagulants.
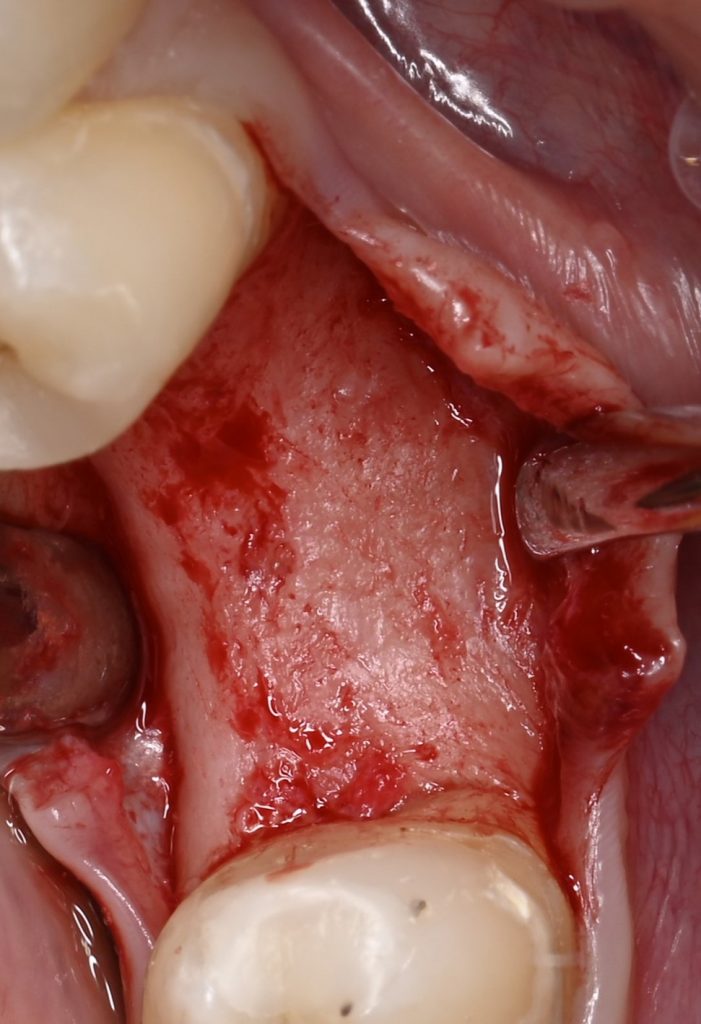
Surgical invasiveness
The flap design can be less extended than with traditional techniques when applying SCAIS. Furthermore, it allows for flapless implant surgery procedures if desired. Avoiding large incisions leads to less trauma for soft tissues and, therefore, faster and less painful wound healing.
Accuracy of implant installation
Due to its high level of accuracy and the accompanying increased predictability, guided implant installation can reduce the risk of incorrect positioning of the implant. Dental implants planned in a prosthetic-oriented backward manner and installed using surgical guides tend to have increased clinical outcomes and show less complications. Thereby, it should be noted that the long-term prognosis of dental implants is associated not only with osseointegration, but with a multitude of further factors.
Challenges
Cost
One of the main obstacles to guided surgery is the higher costs involved. The procedure relies on expensive technological equipment, requiring implant planning software, intraoral scanners, milling machines, and/or 3D printers. As a result, it can increase the costs, making sCAIS unaffordable for some patients and limiting its application by dentists operating in resource-limited contexts.
Training
Clinicians need to undergo specific training to perform guided implant surgery. This creates a recognizable learning curve that can be arduous, while a lack of knowledge can lead to failures, resulting in frustration. Continuous training and keeping up to date with current technologies are the best ways to improve performance.
Dependence on technology
The need for advanced technology can also pose risks. Problems with hardware equipment or planning software can lead to image distortion and complicate the procedure. Furthermore, the accuracy of surgical guides depends on the quality of DICOM images, intraoral scanning, and software assertiveness.
Possibility of human and technical failures
Although guided surgery is accurate, according to the present literature, human and technical errors may occur. Incorrect intraoral adaptation of surgical guides or failures during manufacturing can compromise the accuracy of the final implant position. Additionally, planning errors, such as incorrect interpretation of DICOM images, can produce unsatisfactory results.
Anatomical limitations
Other limitations mainly relate to the patient’s anatomy. Complex clinical scenarios involving poor hard and soft tissues, in terms of quality or/and quantity, may not be solved simply by applying sCAIS. Backward planning is essential to achieve clinical excellence.
Further applications
Digitally planned periodontal surgeries have already been applied to the clinical routine. One example is clinical crown lengthening procedures, where a guide directs the removal of soft and hard tissues ( Tohme et al. 2024). This approach increases the safety and predictability of the surgical procedure, allowing for controlled tissue removal.
Furthermore, static computer-assisted workflows can benefit maxillofacial surgery when planning bone transplants or reconstruction ( Tommasato et al. 2024).
Conclusion
Static computer-assisted implant surgery in dentistry is constantly evolving, enabling greater accuracy and efficiency while providing predictable results. However, it is important to emphasize the need to balance the benefits and challenges of this technique to achieve the best outcome for each patient.
Successful adoption of guided surgery requires investment in technology and training and involves spending more time in the virtual planning phase than with conventional techniques. This time, however, is generally recovered later in the surgical phase, which is faster, simpler and more accurate. As dental technology continues to develop, sCAIS promises to transform dental practice further, improving our patient’s quality of care and clinical outcomes.
Explore every facet of computer-assisted implant surgery at the CAIS conference in Bangkok on November 21, 2024. From static guides to dynamic navigation, from robotic systems to AI integration, we’re covering it all.
- Learn how to seamlessly incorporate computer-assisted techniques into daily practice
- Find out about the maturity, reliability, cost-effectiveness and potential downsides of CAIS
- Discover workflows that can save you time and reduce patient chair-time.
Registration is open. ITI Member discounts available. Reserve your spot today!