Why this review matters
Implant dentistry has always been a balance between biology, mechanics, patient expectations, and time. Over the years, clinicians have developed multiple surgical and prosthodontic approaches to improve predictability, shorten treatment duration, and deliver better functional and esthetic outcomes. But in daily practice, one reality keeps coming back: implant placement timing and loading timing are not independent decisions. They are two parts of the same treatment strategy.
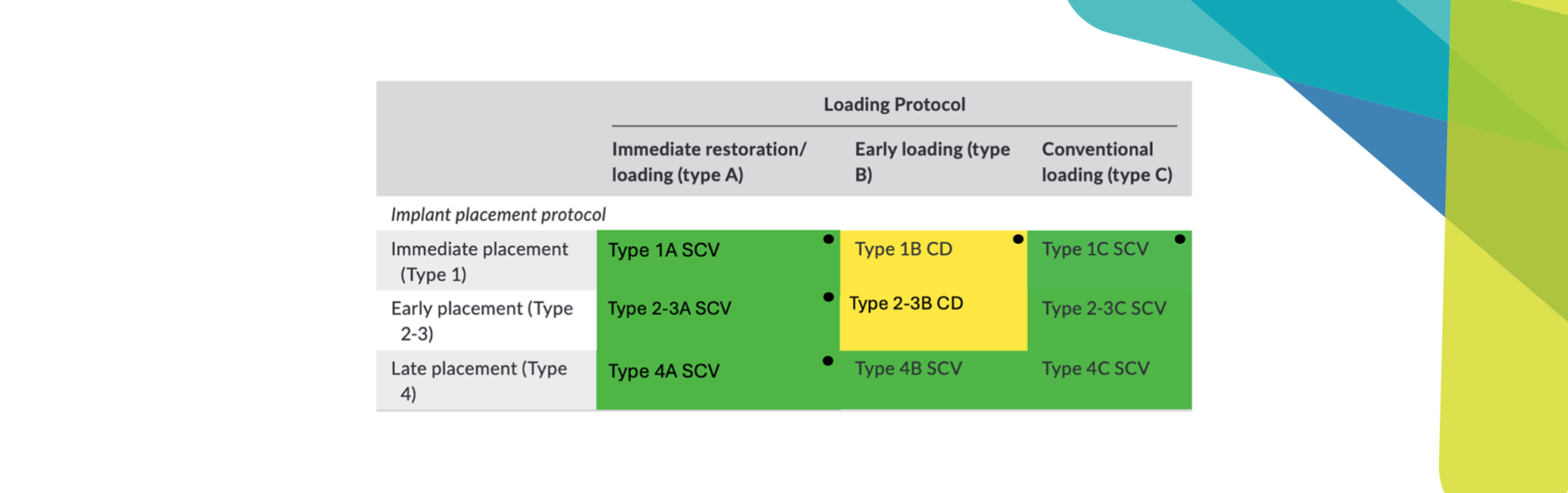
Earlier reviews often discussed these variables separately (placement or loading). A key conceptual shift came in 2018, when Gallucci et al. 2018 proposed an integrated classification that combines both decisions in a single framework. This integrated approach matters because it aligns more closely with how clinicians plan: we choose a surgical timing (immediate, early, or late) and then decide on a loading strategy (immediate restoration/loading, early loading, or conventional loading). Based on this, the following table was developed:

CD (yellow): clinically documented; CID (red): clinically insufficiently documented (includes loading protocols that are not documented); CWD (green): clinically well documented; SCV: scientifically and clinically validated.
How to read the implant placement and loading table
The framework organizes protocols in a simple grid:
- Rows = timing of implant placement
- Type 1: Immediate placement (at extraction)
- Type 2–3: Early placement (after initial healing)
- Type 4: Late placement (in healed sites)
- Columns = timing of loading
- A: Immediate restoration/loading
- B: Early loading
- C: Conventional loading
Many clinicians find this matrix useful because it provides a shared language: instead of loosely saying “immediate implants” or “early loading,” we can define the full pathway clearly and compare outcomes across protocols more consistently.
The 2026 update: a stronger evidence map for everyday decisions
This 2026 updated article is the result of a major research effort developed within our team at the Harvard School of Dental Medicine, by German O. Gallucci, Adam Hamilton, Kevser Pala, Samuel Akhondi, and Juan F. Peña-Cardelles. Recently published in January 2026, it provides an updated, evidence-based overview of implant placement and loading protocols in partially edentulous patients and may play an important role in guiding clinical decision-making in the years to come.
The newest systematic review (published in Clinical Implant Dentistry and Related Research) revisits this same framework with a much larger contemporary evidence base. In practical terms, that means the 2026 update acts less like a “snapshot” and more like a clinical map: it highlights where the evidence is already strong, where accelerated workflows appear promising, and where caution is still warranted due to limited data.
What’s new in the 2026 update
The main difference compared with 2018 is simple: there is now much more evidence, especially for protocols that were previously underrepresented. This strengthens protocol-to-protocol comparisons and gives clinicians more confidence when selecting accelerated pathways. A new table was developed based on the updated findings:
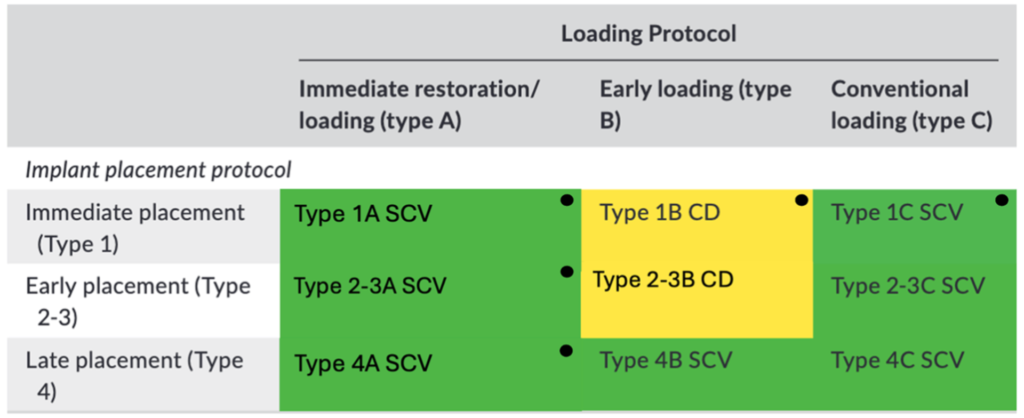
Immediate placement + immediate loading
Type 1A (immediate placement + immediate loading) now includes a large body of clinical documentation and maintains high survival (~98%). Importantly, the increase in documented implants reflects growing clinical interest in immediate placement with immediate restoration, particularly where esthetics drive decision-making. With the broader evidence base, Type 1A can now be considered to be clinically and scientifically validated, with the important caveat that predictability depends on appropriate case selection, stability, and prosthetic control.
Early placement + immediate/early loading
In 2018, some early placement accelerated pathways were less represented. The 2026 update shows stronger documentation for:
- Type 2–3A (early placement + immediate loading), with high survival and improved support.
- Type 2–3B (early placement + early loading), showing excellent outcomes but still based on relatively limited datasets, which limits definitive validation.
Clinically, this matters because early placement is often the compromise option: it may reduce some biological risk compared with immediate placement, while still shortening the overall timeline compared with waiting for fully healed sites.
Immediate placement + early loading
Type 1B (immediate placement + early loading) remains the most uncertain pathway in this framework. The evidence base is smaller, and survival is lower compared with other protocols. From a practical perspective, this pathway sits in a “risk window”: immediate placement already demands careful site management and stability, and early loading adds another layer of mechanical demand before tissues fully mature.
Late placement procotols
The 2026 update reinforces what many clinicians already feel in practice: late placement protocols (Type 4A/4B/4C) remain the most consistently documented and predictable options overall. Among them:
- Type 4C (late placement + conventional loading) remains the conservative benchmark for long-term predictability.
- Type 4A and 4B continue to support controlled acceleration in healed bone when clinical conditions allow.
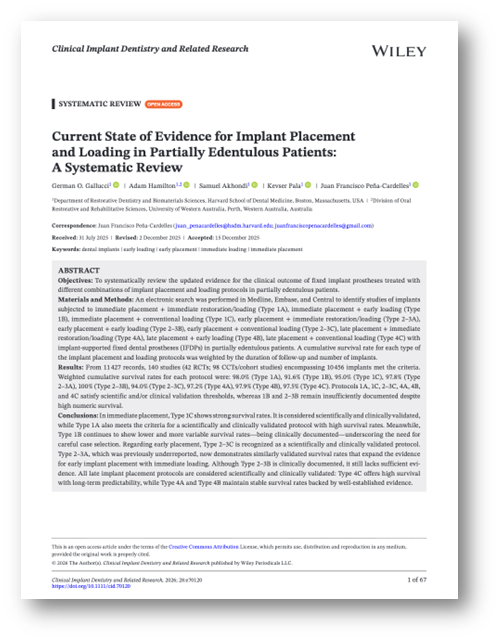
For a deeper dive into methods, validation thresholds, and study-level details, read our full review:
Gallucci GO, Hamilton A, Akhondi S, Pala K, Peña-Cardelles JF. Current State of Evidence for Implant Placement and Loading in Partially Edentulous Patients: A Systematic Review. Clin Implant Dent Relat Res. 2026 Feb;28(1):e70120. doi:10.1111/cid.70120. PMID:41574557.