Introduction
Implant-supported restorations have been the standard of care for the past 30 years. In the beginning, the success criteria were mainly related to the survival of restorations over time (Albrektsson et al. 1986). This definition, however, has evolved in such a way that health, function, and esthetics are also crucial to reach the desired result in implant dentistry (Fürhauser et al. 2005; Papaspyridakos et al. 2012).
After tooth extraction, a reduction in soft and hard tissue volume is expected (Araújo & Lindhe 2005). Therefore, different surgical approaches have been proposed to counteract the effect of this process and provide an appropriate clinical scenario to receive implant-supported restorations (Chappuis et al. 2017). Furthermore, the correct implant position is decisive in providing a final restoration capable of integrating naturally with the adjacent teeth (Buser et al. 2004). It is important to note that the diameter and the cylindrical shape of an implant or a prefabricated healing abutment will not coincide with the natural cervical contours of teeth (González-Martín et al. 2020). Therefore, management of the transgingival region is important to deliver a natural-looking final restoration (Su et al. 2010). When adequate soft tissue volume and the correct three-dimensional implant position have been achieved, contour management of this region using provisional restorations can be considered. Otherwise, additional surgeries may be necessary before applying this strategy.
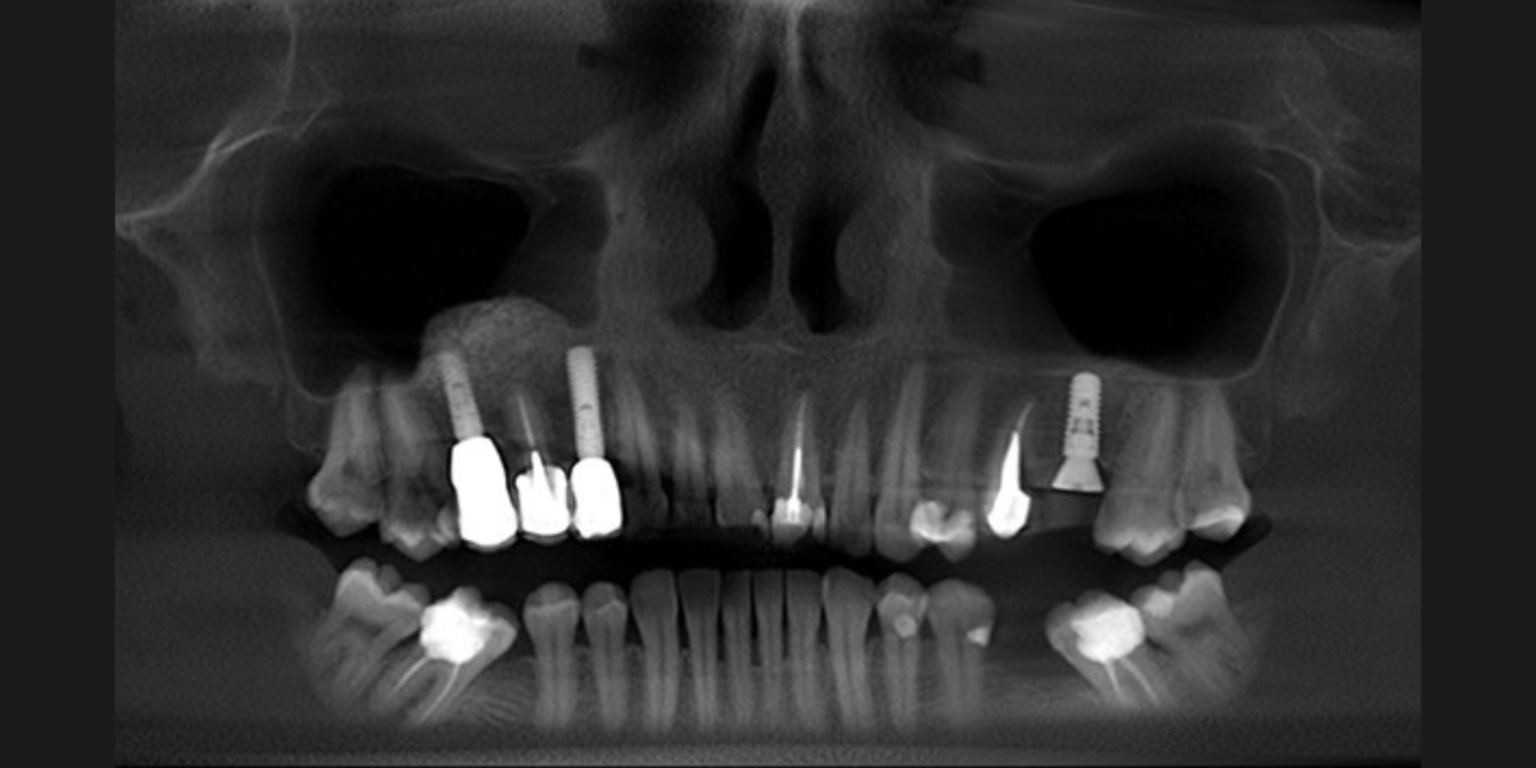
When it comes to soft tissue management using provisional restorations, different approaches have been suggested to obtain adequate contours capable of integrating white and pink esthetics (Fig. 1). This review aims to highlight some relevant concepts and techniques related to this topic.


The emergence profile
Located between the implant platform and the soft tissue cervical margin, the emergence profile is responsible for the transition from the cylindrical shape of the implant to the final contour of the crown (González-Martín et al. 2020). This region should respect the anatomical characteristics of the soft tissues as well as allowing the maintenance of hygiene. In this sense, and in order to help clinicians work within this transgingival region, the critical and subcritical contours have been proposed (Su et al. 2010). The critical contour, related to the cervical margin of the restoration, is responsible for the final shape of the tooth. While the subcritical contour, apically positioned, is responsible for the support of the soft tissues (Fig. 2).

An adequate emergence profile should allow a smooth transition from the implant platform to the cervical margin. To achieve this goal, a correct three-dimensional implant position is essential, as well as sufficient tissue volume (Buser et al. 2004). For example, a too-shallow position of the implant would impair the possibility of working on the emergence profile, which could result in an over-contoured restoration (Fig. 3). On the other hand, a too-deep position of the implant would result in a large supracrestal tissue height (STH) (Avila‐Ortiz et al. 2020), which has been reported to exhibit a less favorable pattern of resolution of peri-implant mucositis (Chan et al. 2019).

Provisional restorations design
Two clinical situations must be differentiated when considering the design of provisional restorations. In the case of immediate implants, the goal is to maintain the gingival architecture. In the case of delayed implants, the challenge is to recreate the tooth contours that were lost (González-Martín et al. 2020).
In our experience, the following strategies may allow for adequate soft tissue contour conformation:
Immediate implants
In this clinical situation, it is interesting to support the soft tissue architecture at the critical contour level (Wang et al. 2020). For this, the marginal region of the provisional restoration should accompany the gingival soft tissue contours. On the other hand, a concave subcritical contour in the buccal region will provide space for a stable blood clot that will ultimately result in thicker soft tissues after healing.
In addition to achieving this goal with a provisional restoration, the use of customized healing abutments has also been described as a favorable alternative for this purpose (Ruales‐Carrera et al. 2019).
Delayed implants
After osseointegration and soft tissue maturation, site development to recreate the desired tooth contours can be achieved through the use of customized healing abutments or provisional restorations. In this scenario, a concave or flat subcritical contour may be adequate, while the critical contour might be positioned at the zenith level of the desired tooth.


Soft tissue conditioning
If the contours are not as expected after soft tissue healing, it is still possible to condition them to achieve the desired result (Wittneben et al. 2013). For this purpose, strategic modifications can be made to the volume of the provisional restorations with the help of flowable composite resin or acrylic resin (Fig.4). Consequently, after insertion of the provisional restoration, mucosal pressure and transient ischemia (up to 10 minutes) are to be expected. It is essential to control this reaction, as excessive pressure on the mucosa can lead to a lack of vascularization and thus to the induction of necrosis and tissue inflammation (Wittneben et al. 2013). Pauses of at least one week between each increment should be considered to maintain mucosal health. These gradual modifications can be performed until the desired contours and final emergence profile are obtained (Fig. 5).
Transfer of the emergence profile
Once the desired contours have been obtained, special care must be taken to transfer all these features to the master model. Conventional or digital impressions can be used for this purpose. However, the contours of the provisional restoration should be copied using individualized transfer abutments or digital scanning to avoid the influence of the collapse of the emergence profile achieved (Hinds 1997). This will allow the delivery of a final restoration with the same contours that were achieved with the provisional restoration and, therefore, stable esthetic results can be obtained.

Contour soft tissue management through the use of provisional restorations represents an appropriate approach to achieve natural contours and improve the esthetic outcome of implant-supported restorations. Healthy tissues with adequate volume and the correct three-dimensional implant position are essential to take advantage of the benefits of this strategy. In the absence of favorable conditions, further surgical procedures may be necessary prior to the application of these techniques. Attention to detail at each stage will provide greater control and predictability.
For further references, check out the following content pieces on the ITI Academy: