Introduction
The Straightforward, Advanced and Complex (SAC) classification in implant dentistry was introduced following an International Team for Implantology (ITI) Consensus conference held in 2007 (Dawson 2009). The classification aimed to assist clinicians in evaluating the difficulty of cases, and serve as a tool for case selection and treatment planning. Individual cases can be classified into straightforward, advanced, or complex in both surgical and restorative aspects depending on their associated risk factors and complexity.
The aim of this article is to illustrate how the SAC classification was used to identify a case of high surgical and esthetic risk, the steps undertaken to minimize potential complications, and its successful long-term follow-up.
Clinical presentation and treatment planning
In January 2018, a 44-year-old Singaporean Chinese male presented at National Dental Centre Singapore after being informed by his private general dental practitioner that his upper front tooth could not be saved and would need to be removed. He had no relevant medical history and no known drug allergies. He did not smoke or drink alcohol.
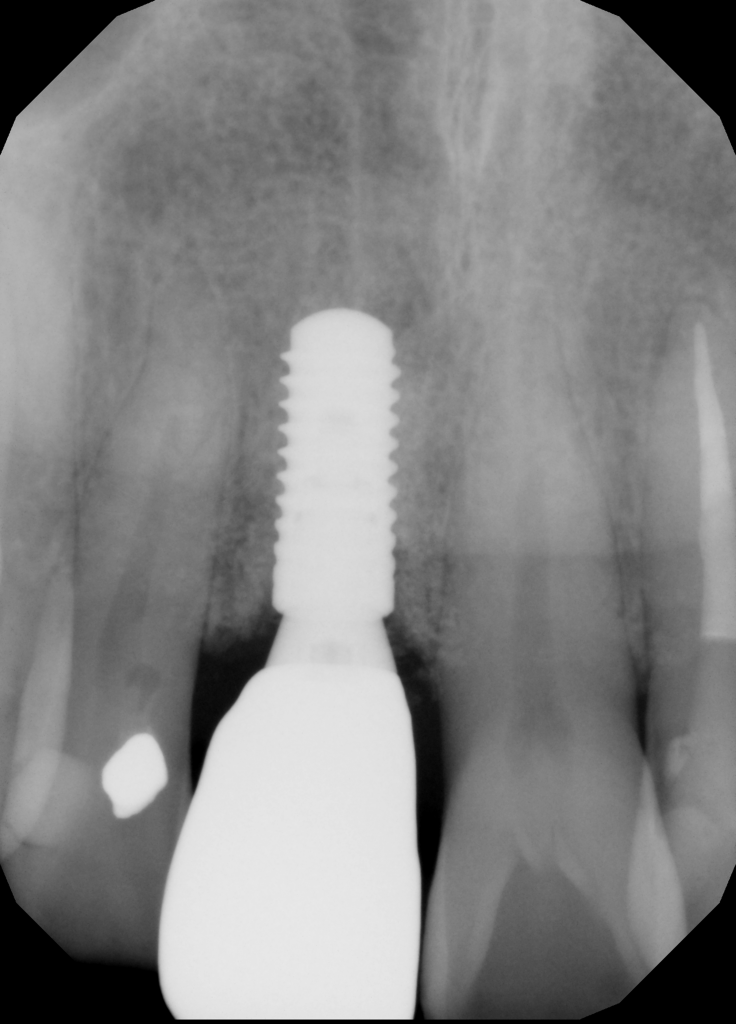
The tooth in question was his upper right central incisor (#11) which sustained trauma and received root canal treatment about 20-25 years ago (Fig. 1). Subsequently, the tooth was restored with a crown about 10 years ago.
He has a moderate smile line. His gingiva is of scalloped margins and knife-edge architecture. His phenotype is thin anteriorly and moderate posteriorly. There was a sinus tract present at the buccal aspect of #11 alongside with deep probing pocket depth of 6-11 mm at the buccal sulcus. Tooth #11 was extruded compared to the rest of his upper anterior teeth.
Radiographic examination revealed a large periapical radiolucency at root canal treated #11 (Fig. 2). Sinus tract tracing showed communication from the sinus tract through the apex of #11, distal surface and finally the cervical region.
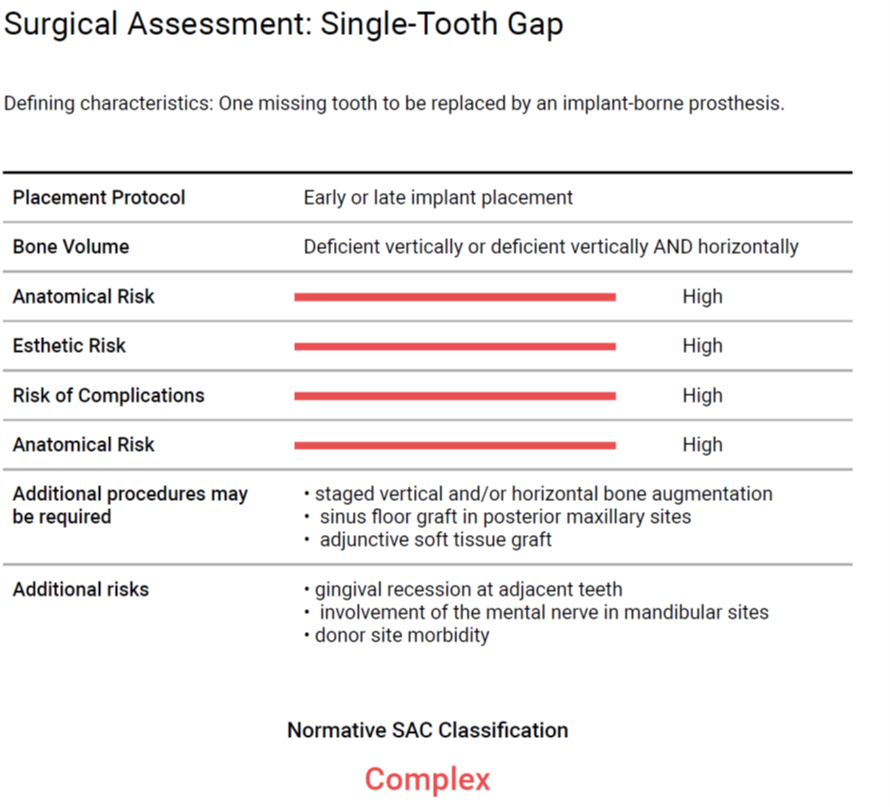
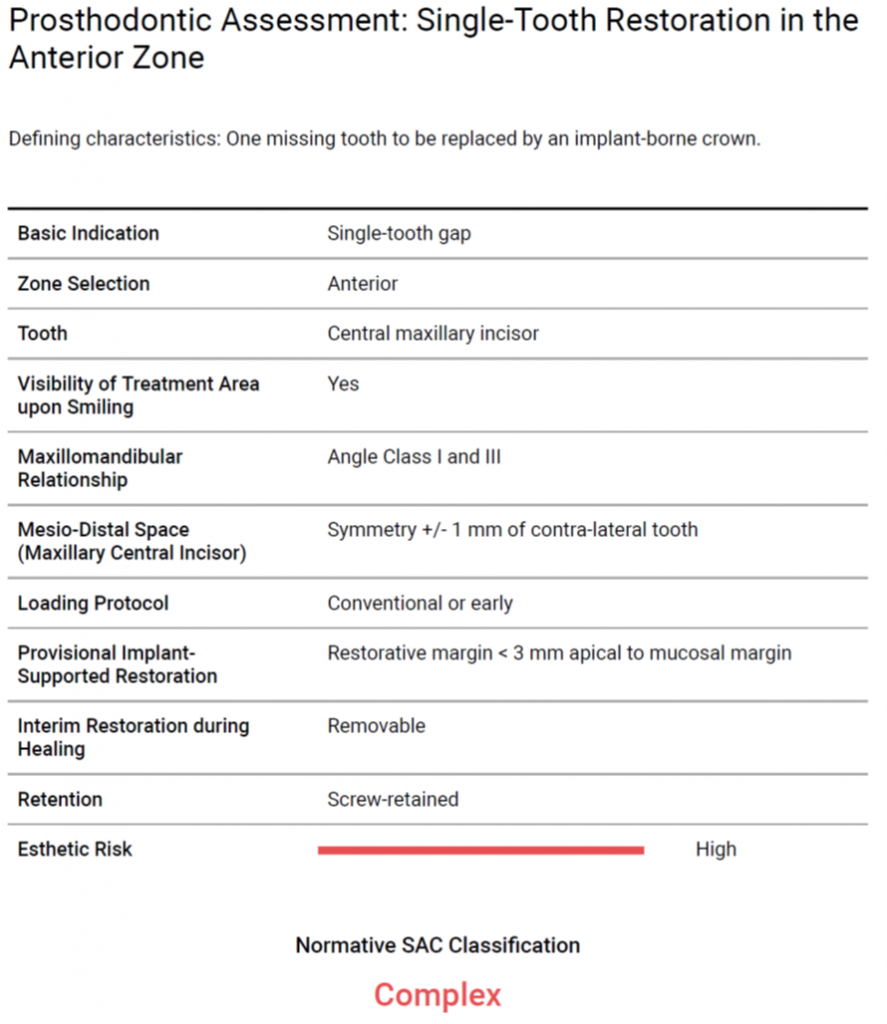
Tooth #11 was diagnosed as previously treated with a chronic apical abscess associated with a vertical root fracture. The pre-therapeutic prognosis of #11 was deemed irrational to treat. Surgical and prosthodontic risk assessment categorized this patient as complex in both instances (Fig. 3 – 4).
A comprehensive case presentation and discussion was held with the patient. It was proposed to remove #11 with simultaneous ridge augmentation. Due to a high esthetic risk, the patient was informed that a connective tissue graft may be necessary to correct soft tissue deficiencies before delayed implant placement and restoration with an implant-supported single crown.
Case management – surgical phase
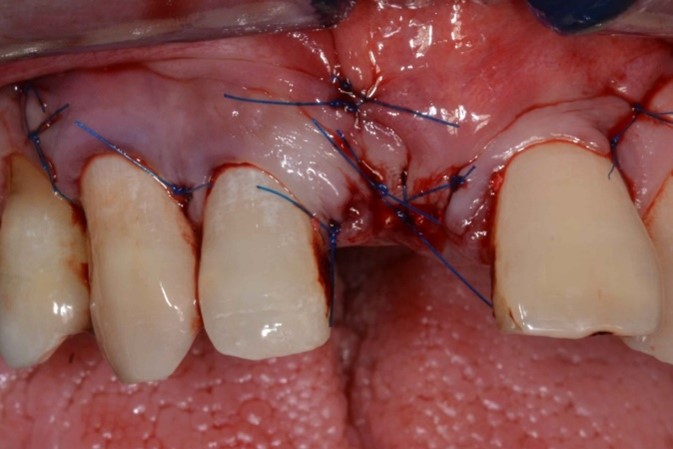
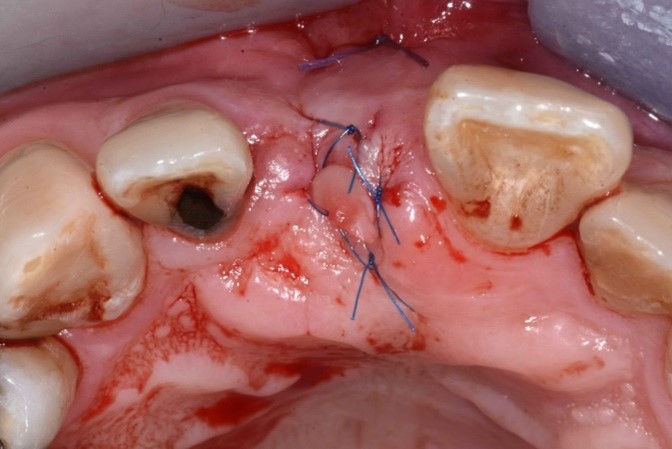
On raising the flap, it was found that the buccal bone of #11 was lost and a fracture line was detected at the disto-buccal surface of the tooth. There was also a fenestration of the buccal bone at #12 (Fig. 5).
Tooth #11 was removed, and cortical perforation done in preparation for ridge augmentation (Fig. 6). Simultaneous ridge augmentation was performed using a 90% porcine xenograft and 10% porcine collagen, and a porcine pericardium membrane (Fig. 7). Horizontal periosteum release was performed, and primary closure of the surgical site was achieved (Fig. 8).
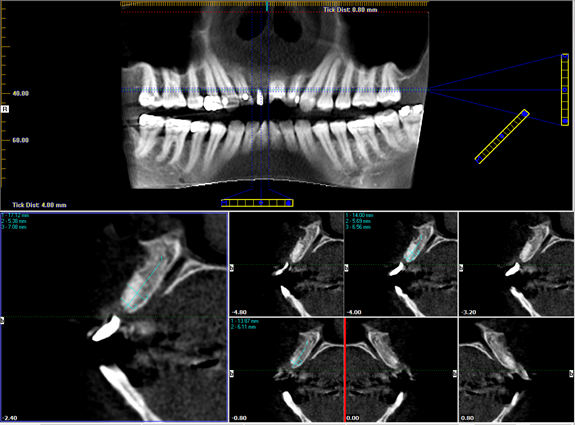
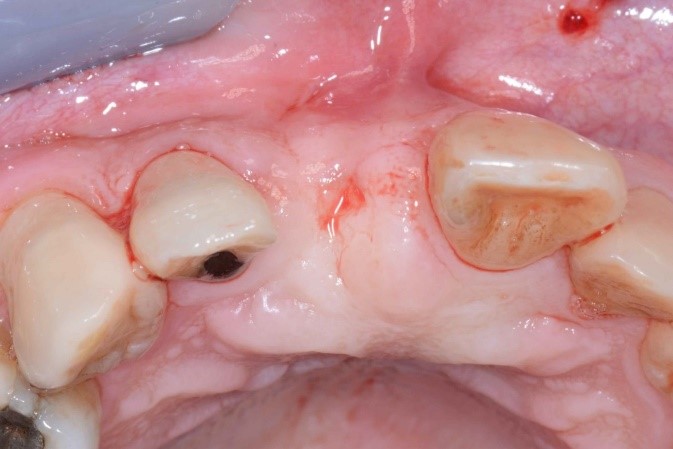
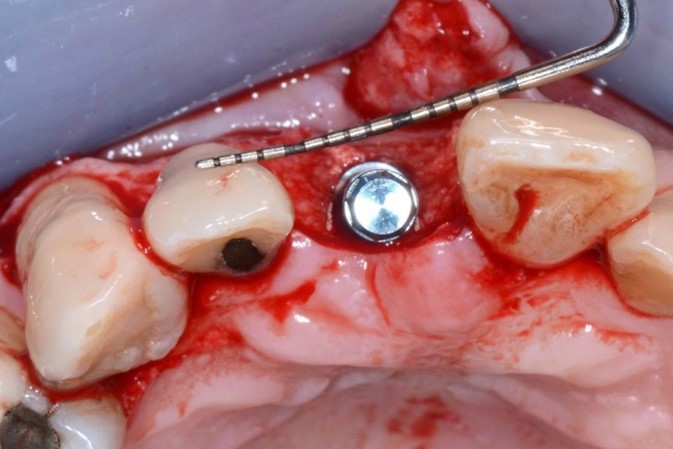
A cone-beam computed tomography examination was performed 6 months later, revealing ridge width of 6-7 mm, sufficient for placement of a regular diameter implant in a restoratively driven position (Fig. 9).
However, clinical examination revealed a horizontal soft tissue deficiency (Fig. 10). Given the high esthetic risk assessment, soft tissue augmentation using connective tissue graft and a tunneling technique (Fig. 11 – 12) was performed.
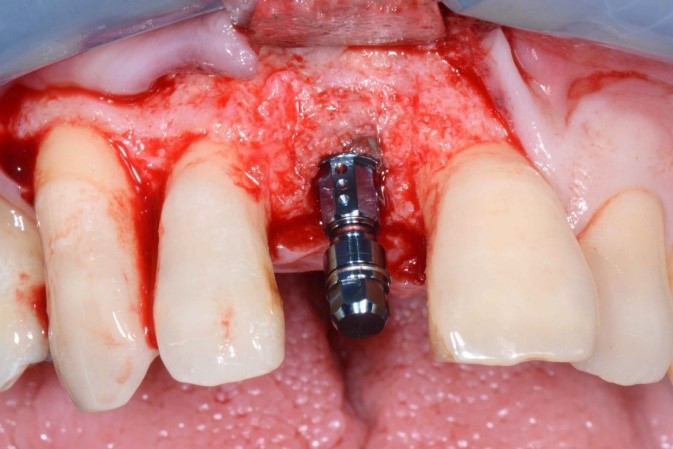
Correction of the horizontal soft tissue deficiency was achieved (Fig. 13), and delayed implant placement was performed 4 months later. A regular diameter Straumann Bone Level implant 4.1mm by 10 mm was placed in an ideal 3-D position (Fig. 14) and as the buccal wall thickness was <2 mm, simultaneous contour augmentation was performed using a porcine xenograft and porcine pericardium membrane (Fig. 15). Stage 2 implant surgery was performed 2 months later (Fig. 16).
Case management – restorative phase
Provisionalization of an implant supported single crown was carried out using a Straumann Temporary Abutment with layered composite resin. The planned implant position was executed as planned, allowing for a screw-retained configuration. The implant provisional allowed for appropriate adjustment of the soft tissues and for the patient to evaluate if the esthetics were satisfactory, and function adequate. The provisional restoration was inserted for 4 months for soft tissue conditioning (Fig. 17) before the definitive crown was delivered (Fig. 18).
The definitive crown was designed using CAM software and fabricated using monolithic zirconia. The monolithic zirconia was stained to mimic the color of the contralateral central incisor and was cemented on a Variobase, with GH 2 (Gingival Height 2). The Straumann Variobase allowed the versatility of replacement with a monolithic material with a screw-retained configuration.
Clinical outcomes
An esthetic outcome was achieved for the patient, despite being classified as having a high esthetic risk. At 18 months post-loading, the esthetic outcome was maintained with stable scalloped gingival margins (Fig. 19), sufficient buccal tissue thickness (Fig. 20), and stable crestal bone level (Fig. 21).
Discussion
Recently it was identified that implant malposition and having a thin peri-implant phenotype are significant risk factors for recession of the peri-implant mucosa – an implant placed too buccally and an implant placed in thin peri-implant phenotype has an odds ratio of x15 and x8 respectively of developing soft tissue dehiscence (Romandini et al. 2021). To account for these risk factors in the case illustrated, the implant was placed in an ideal 3-dimensional position (Buser et al. 2004) and a connective tissue graft was performed to change the peri-implant tissue phenotype. Furthermore, as the buccal wall was thin following site preparation, simultaneous ridge augmentation was carried out during implant placement (Spray et al. 2000).
A screw-retained restoration allows for easy retrievability in the event of any complications. Given that it is a screw-retained restoration, there is also no risk of excess cement. A monolithic zirconia restoration reduced the risk of chipping by avoiding the need for veneering ceramic. However, there were slight colour variances due to the difficulty in achieving an exact reproduction of the color of the contralateral tooth (Farhad 2019). The patient was satisfied with the restoration and was not keen to undergo any additional staining.
The patient has been reminded to maintain good oral hygiene using an interdental brush around the implant. He is reviewed once yearly for any potential prosthetic complications and every 9 months for periodontal maintenance.
Conclusion
The SAC classification is a clinically relevant tool to identify the degree of difficulty and risks involved. Upon identification of a complex case, appropriate measures such as soft tissue augmentation must be taken to manage risk factors and ensure long term success.
Additional resources