Introduction
Full-arch fixed implant-supported restorations are a commonly utilized strategy for the rehabilitation of fully edentulous patients. Managing patients with severe atrophy in both the maxilla and mandible presents challenges such as diminished vertical height and poor bone density (Nickenig et al. 2016). Achieving favorable long-term functional and esthetic results and enhancing patients’ quality of life necessitate a meticulous approach to implant positioning based on prosthetic factors (Cabanes et al. 2021, Buser et al. 2008).
There has been an increased preference for computer-assisted implant surgery, which may be static or dynamic. Through this technology, the surgeon is directed in the placement of dental implants, thus optimizing safety and minimizing the risks associated with conventional surgical techniques (Xiaojun et al. 2009, Wei et al. 2021). This shift towards the widespread adoption of computer-assisted implant surgery, whether static or dynamic, facilitates precise implant placement, ultimately increasing safety and decreasing the risks linked to traditional freehand surgery (Aydemir & Arısan 2020). In dynamic navigation surgery, preoperative planning utilizing navigation software directs implant placement in real-time during surgery through tracking and guidance mechanisms. This technology is particularly advantageous for patients with limited mouth opening, and it allows for modifications to the plan during the surgery, which is impossible with the static guide (Gargallo-Albiol et al. 2019). A recent meta-analysis by X. Yu et al. reviewed clinical studies from the last decade to determine the effectiveness of dynamic computer-assisted implant surgery in fully or partially edentulous patients compared to static navigation. The analysis concluded that dynamic navigation is a reliable method for implant placement, capable of reducing angular deviations during placement (Yu et al. 2023). The implementation of surgical navigation systems has shown a notable enhancement in the precision and safety of implantation procedures. Nevertheless, the constant need for surgeons to shift focus between the surgical field and computer screen poses challenges. This issue is anticipated to be addressed through the integration of mixed-reality technology, utilizing HoloLens devices to align virtual 3D images with the actual surgical site within the same visual field (Fan et al. 2023).
Intraoperative navigation encompasses a registration procedure that aligns the patient’s position with the preoperative imaging data. Registration is the key factor of navigation surgery, and the registration process largely determines the accuracy of the navigation feedback (Wu et al. 2019). Any errors in image registration can lead to inaccurate virtual implant placement and guide template fabrication, resulting in discrepancies between the planned and actual implant position (Schreurs et al. 2021).
Zygomatic implants (ZIs) are specifically recommended for treating severe maxillary atrophy and defects. The intricate anatomy and narrow bone width of the zygomatic bone present difficulties for clinicians during implant placement procedures. A real-time surgical navigation system utilized for quad zygomatic implant placement exhibited high accuracy, showing minimal deviations from the planned locations, regardless of implant lengths or positions. The proper utilization of fiducial configuration is imperative for successful zygomatic implant placement (Wu et al. 2019, Hung et al. 2017, Wang et al. 2018).
What are the different methods of registration currently employed in dynamic-navigation-assisted implant placement in edentulous patients?
Depending on the reliance on marker points, there are marker-based and markerless registration methods (Lübbers et al. 2011, Zhou et al. 2021). Marker-based can be further classified as invasive and non-invasive based on invasiveness. Correspondingly, pair-point or surface-based techniques are employed based on the underlying registration algorithm. User dependency is another factor for classification, where some methods require more user involvement than others. Apart from this, manual and automatic registration methods are also used (Fig. 1). Selection of a registration technique depends on factors such as accuracy requirements, invasiveness of fiducial placement, soft-tissue deformation, and pre- or intra-operative logistics.
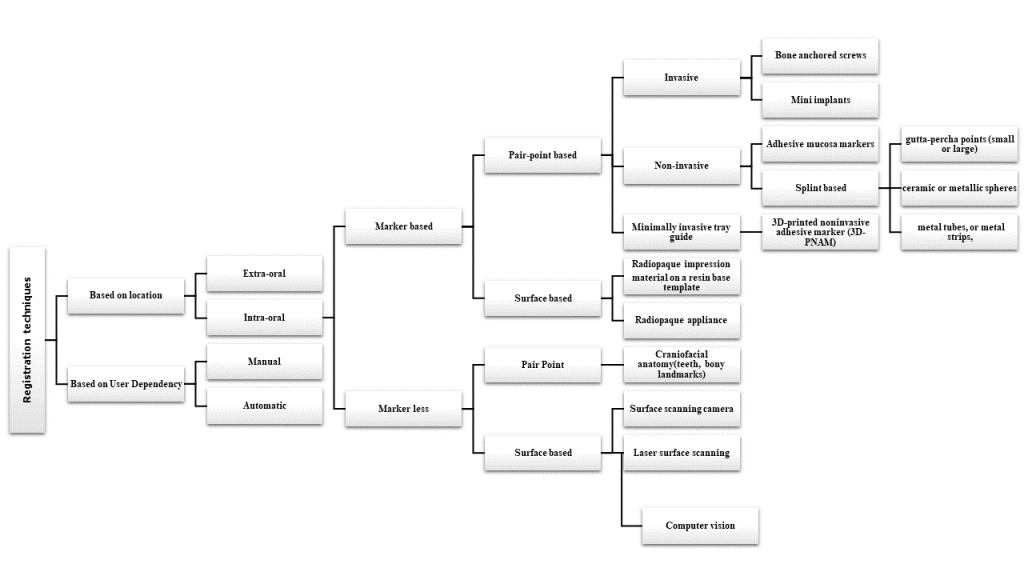
Fig. 1: Classification of registration techniques used in dynamic navigation assisted implant placement
This review paper is structured in two distinct sections and articles to enhance clarity. The first section extensively discusses various marker-based registration methods. Conversely, the second section offers a detailed investigation of markerless registration techniques utilized in the context of dynamic-navigation-assisted implant placement.
What are the frequently used marker-based registration methods in edentulous patients?
Marker-based registration methods are commonly employed in edentulous patients to facilitate navigation-assisted surgery. The application of markers followed by radiography is a widely utilized technique for achieving accurate and reproducible registration (Lübbers et al. 2011).
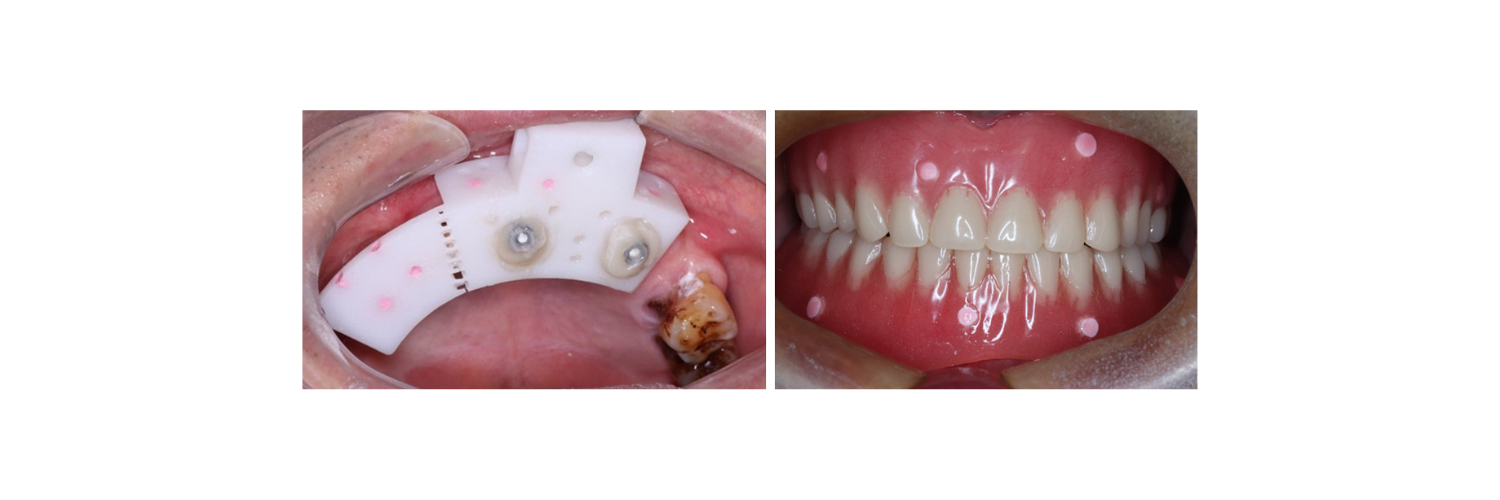
Numerous approaches have been described in the literature, ranging from invasive methods such as bone-anchored titanium mini screws (Lübbers et al. 2011) (Fig. 2), and mini implants, to minimally invasive techniques like 3D printed tray (DENA tray, Mininavident) in combination with an optical marker as well as the use of splints or appliances with attached radio-opaque materials such as gutta-percha (Woo et al. 2020) (Fig. 3), metal strips, ceramic, or metallic spheres. Additionally, non-invasive methods such as the utilization of silicone elastomer material with titanium screws, the use of radio-opaque appliances (barium sulfate scan appliance) and adhesive fiducial markers attached to the mucosa have also been explored (Lan et al. 2022, Ekram et al. 2022) (Fig. 4). A brief description of the methods is given below.
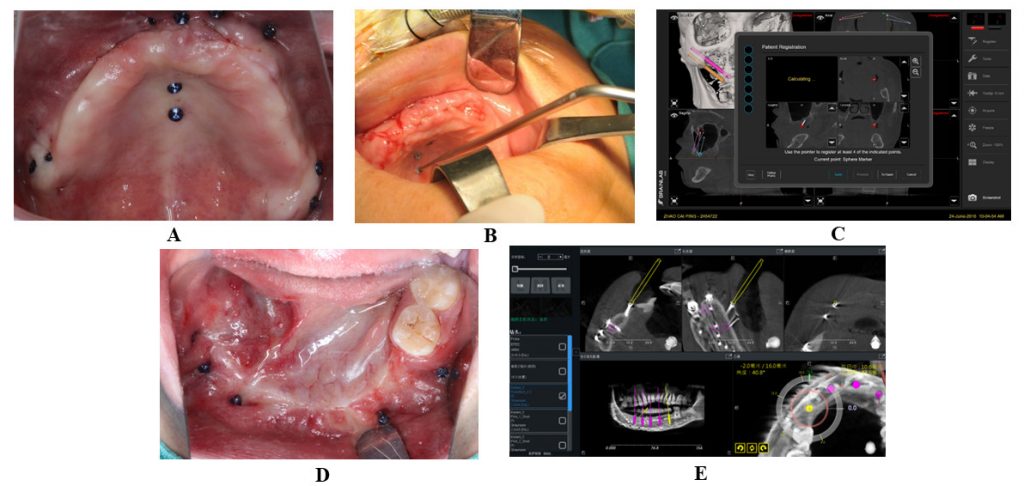
Fig. 2: Bone-anchored fiducial screw-based registration technique in completely edentulous patient using Brainlab software. A: Bone-anchored fiducial screws placed in maxilla in a specific configuration; B: Registration of markers using specific probe recommended by manufacturer; C: Registration method shown on the dynamic navigation software for maxilla; D: Bone-anchored fiducial screws placed in mandible; E: Registration method shown on the dynamic navigation software for mandible 
Fig. 3: Splint-based registration technique. A: 3D-printed template containing radiopaque markers (gutta percha) for registration; B: Patient’s existing complete denture modified by adding radiopaque markers (gutta percha) for registration 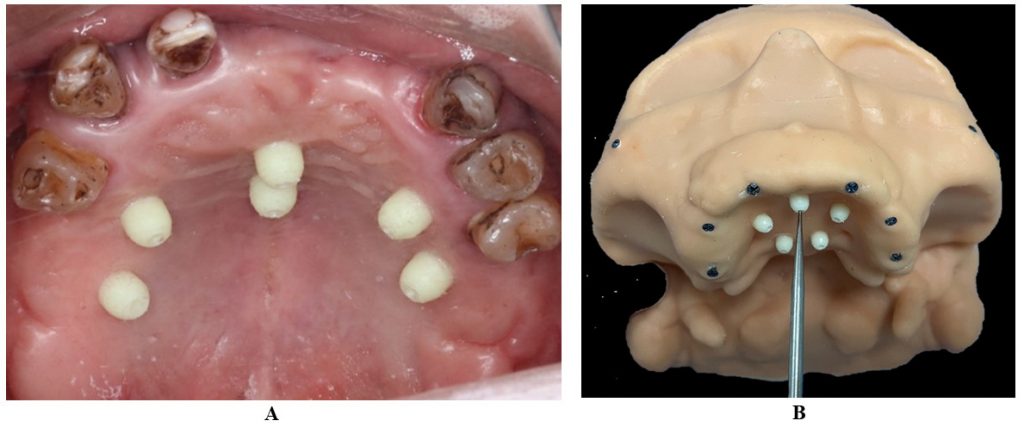
Fig. 4: Adhesive fiducial markers attached to the oral mucosa. A: 3D-printed ceramic markers attached to mucosa using bio-adhesive glue; B: Registration of adhesive markers using specific probe recommended by manufacturer
Bone-anchored screws and mini implants (Wei et al. 2021, Woo et al. 2020).
Small titanium screws and narrow-diameter implants are strategically positioned in the edentulous ridges or adjacent bone, providing precise guidance during dynamic navigation for implant placement and prosthetic alignment, thereby enhancing treatment precision and outcomes. The utilization of bone-anchored screws as a marker-based registration technique is widely regarded as the gold standard for “paired-point” registration in dynamic navigation for dental implant surgery. Bone-anchored screws offer a dependable approach for obtaining accurate navigation feedback and are especially valuable in procedures where precision is paramount, such as zygomatic implant placement (Fig. 1).
3D printed tray (DENA tray, Mininavident) in combination with an optical marker (Fan et al. 2023).
Combining a 3D printed tray, such as the DENA tray or Mininavident tray, with an optical marker involves the customized design of a tray that perfectly fits the patient’s oral anatomy. An optical marker integrated into the tray is a reference point for dynamic navigation systems or intraoral scanners, ensuring accurate tracking and positioning during procedures such as guided implant placement or digital impressions. This approach enhances accuracy, efficiency, and patient comfort in dental treatments and prosthetic fabrication processes.
Splint or denture with radiopaque markers (Lübbers et al. 2011, Ekram et al. 2022)
This method entails using a splint or existing denture containing radiopaque markers for registration. It ensures accurate registration for dynamic navigation in dental implant surgery; however, it necessitates the patient wearing a splint or denture with markers, which may cause discomfort (Fig. 3).
Adhesive fiducial markers attached to the oral mucosa (Lan et al. 2022)
Adhesive fiducial markers affixed to the mucosa play a crucial role in dynamic navigated dental implant surgery by offering non-invasive reference points for precise navigation and alignment during procedures. These markers securely adhere to the surface of the skin, thereby assisting optical tracking devices and cameras in maintaining meticulous positioning between the patient and pre-operative imaging data (Fig. 4).
Extraoral registration technique (Zhou et al. 2021)
Severe maxillary defects resulting from maxillectomy pose challenges to rehabilitation efforts. While the zygoma can be a viable option for implant placement in such cases, its irregular shape and limited visibility present obstacles that can lead to complications. Dynamic navigation surgery emerges as a minimally invasive solution, ensuring precise implant placement (Hung et al. 2016). The accurate placement and configuration of fiducial markers are crucial in these scenarios.
Zhou et al. (2021) proposed a novel technique for the registration of a dynamic navigation system which involves the use of fiducial markers positioned at extraoral sites that can serve as a viable registration technique to overcome anatomical limitations in patients who have undergone maxillectomy and still achieve a satisfactory level of registration accuracy (Zhou et al. 2021) (Fig. 5).
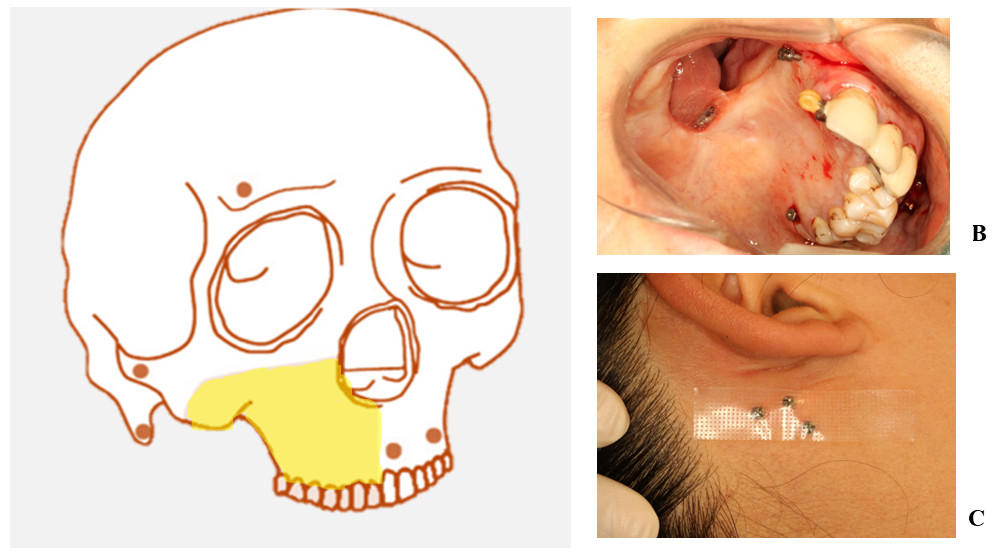
Fig. 5: Registration technique for patients with unilateral maxillectomy defects. A: Diagrammatic presentation of fiducial marker position in unilateral maxillectomy defect; B: Bone-anchored fiducial screws placed intraorally near the maxillectomy defect area; C: Bone-anchored fiducial screws placed extraorally
Most of the methods involve radiopaque markers to aid in the registration of scans for preoperative planning and implant placement (Lübbers et al. 2011, Fan et al. 2023, Zhou et al. 2021). Different registration techniques have varying levels of accuracy and coverage. These marker-based methods provide reproducible positioning of the markers and automatic localization in different imaging modalities, making them practical for clinical interventions
What are the most important factors when choosing a marker-based registration method for edentulous patients?
When choosing a marker-based registration method, the most important factors to consider are accuracy and reproducibility, invasiveness of fiducial placement, soft-tissue deformation, and pre- or intra-operative logistics (Lübbers et al. 2011, Shen et al. 2023, Chackartchi et al. 2020). Other factors including the number, size and configuration of the markers used should also be considered. A study by Shen et al. reported that a scattered, polygonal distribution with a minimum of five fiducial markers in an edentulous maxilla could achieve acceptable target registration error values in registration (Shen et al. 2023, Zhang et al.2011).
What are the advantages and disadvantages of marker-based registration methods for edentulous patients?
Marker-based registration methods have both advantages and disadvantages. One benefit of employing marker-based methodologies, such as the implementation of markers succeeded by radiography, lies in their tendency to manifest a superior degree of precision and consistency in contrast to marker-less approaches (Lübbers et al. 2011). Another advantage is that the insertion of five fiducial markers significantly increases the accuracy of implant placement for edentulous mandibular arches(Lübbers et al. 2011, Shen et al. 2023, Zhang et al. 2011). Additionally, a personalized 3D-printed non-invasive adhesive marker has been developed as an alternative to invasive screw markers, with similar accuracy results (Shen et al. 2023). Conversely, marker-based methods have the disadvantage of potentially causing additional trauma, scar formation, and patient discomfort, particularly when invasive screw markers are employed (Lübbers et al. 2011, Woo et al. 2020). In summary, marker-based registration methods offer improved accuracy but may come with drawbacks such as invasiveness and patient discomfort.
What are the limitations/challenges of marker-based registration methods for fully edentulous patients?
Marker-based registration methods for fully edentulous patients face challenges regarding accuracy and reproducibility (Lübbers et al. 2011).In the absence of fixed dental markers, markerless techniques are generally considered to be less accurate and reproducible (Lübbers et al. 2011, Thiem et al. 2022, Ekram et al. 2022). Furthermore, the invasiveness associated with the use of screw markers for implantation in edentulous patients poses a challenge. This method can result in additional trauma and discomfort (Lübbers et al. 2011). However, non-invasive adhesive markers have been developed as an alternative, and they have been shown to have the same accuracy as screw markers (Lan et al. 2022). Intraoral scanning and soft tissue-based registration methods have also been used for edentulous patients, and they have been found to be highly precise (Chackartchi et al. 2020, Fan et al. 2014). Another challenge is radiation exposure.While, marker-based registration methods can be challenging in fully edentulous patients, advancements in technology and the development of non-invasive markers offer promising solutions for accurate and reproducible registration.
What are the potential solutions to the challenges of using marker-based registration methods for fully edentulous patients?
Potential solutions to the challenges of using marker-based registration methods for fully edentulous patients include the use of soft tissue-based registration and non-invasive adhesive markers (Lan et al. 2022, Benjamin et al. 2022, Deferm et al. 2023). Consequently, it is feasible to attain a notable level of precision in scanning the jaw and registering soft tissue, even when teeth are not present, by implementing a cone-beam computed tomography scan along with an intraoral scan (Benjamin et al. 2022, Deferm et al. 2023). Marker-free methods, although generally less accurate and reproducible, can be used for registration in edentulous patients (Thiem et al. 2022, Ekram et al. 2022). Additionally, a 3D-printed non-invasive adhesive marker has been developed as an alternative to invasive screw markers for implantation in edentulous patients, with comparable accuracy to screw markers (Ekram et al. 2022). These potential solutions offer alternatives to traditional marker-based registration methods, reducing the need for invasive procedures and improving accuracy in fully edentulous patients.
Would you like to read more about this topic?
Stay tuned – the second part of this article will be published September 24, 2024 on this blog.