Background
In static computer-assisted implant surgery (sCAIS), a digitally planned and fabricated surgical guide (SG) is crucial to the successful placement of dental implants in an optimal three-dimensional position. While the high accuracy of this treatment approach is widely acknowledged, factors contributing to heightened inaccuracies are only partially comprehended and not widely addressed. Some of the factors affecting the final outcomes are data acquisition and merging, guide design, fixation and support, guide production (method and material), along with surgical and technical factors. Numerous studies have highlighted the impact of guide stability and support on the accuracy of sCAIS. Optimal guide design, a commonly underemphasized factor, plays a substantial role in guaranteeing the stability, accuracy, and reliability of surgical guides, as well as avoiding common complications such as guide fracture. This blog article aims to describe the main challenges and principles of sCAIS planning for partially edentulous cases. It outlines the relevant steps of the process with a special focus on guide design in a manner applicable to the daily practice of the readership.
Designing the Guide
The translation of the virtually planned implant position into the actual implant placement is crucial, and a range of factors within the digital workflow may lead to deviations. While the software typically provides a plan for guide production, specific considerations in the guide designing process, such as stabilization and support, sleeve height, guide-hole design, inspection windows, and material thickness demand meticulous attention to guarantee a successful outcome. The design of the guide can significantly influence the accuracy of sCAIS.
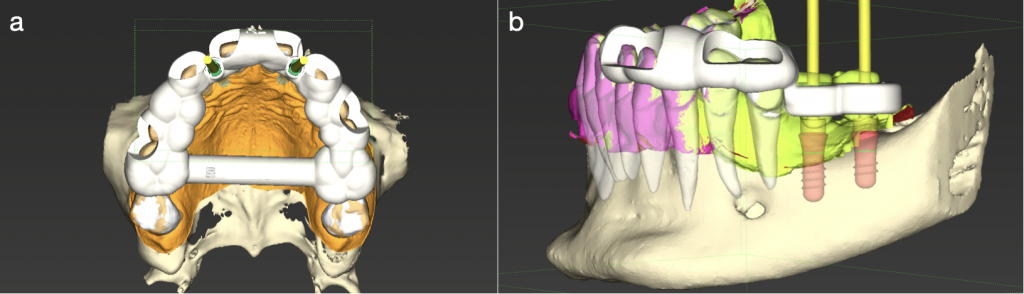
Guide stabilization and support
Surgical guide (SG) stability is a well-known essential factor for a successful outcome, as mobility of the surgical guide during drilling/implant placement is related to a high deviation between planning and clinical result. In partial edentulism, the SG can be supported by teeth (tooth-supported), a combination of teeth and mucosa, or teeth and bone (Fig. 1). Tooth-supported guides provide higher stability and accuracy compared to the other supporting structures (Arisan et al. 2010; Raico et al. 2017; Pozzi et al. 2016), and there is a positive relationship between the number of supporting teeth and sCAIS accuracy. Furthermore, the use of posterior teeth as support results in higher accuracy when compared to the same number of anterior teeth (El Kholy et al. 2019). Moreover, scenarios involving a single-tooth gap (STG) present more accurate surgical results, whereas clinical situations with unilateral anchorage (e.g., distal extension) are associated with heightened deviation. Extended edentulous spaces may require additional support to maintain the same level of accuracy as STG (Van Assche et al. 2007; Pozzi et al. 2016; El Kholy et al. 2019). In such scenarios, supplemental mucosa support, preferably attached keratinized tissue, can improve implant placement accuracy. Additionally, support alternatives such as mini-implants or fixation with pins and screws can provide greater stability (Mai & Lee, 2020; De Souza et al. 2022; Pessoa et al. 2022). The guide must be accurately positioned on the teeth or ridge. Otherwise, fixation will perpetuate erroneous positioning. Inspection windows serve as valuable tools to verify the proper seating of the surgical guide.
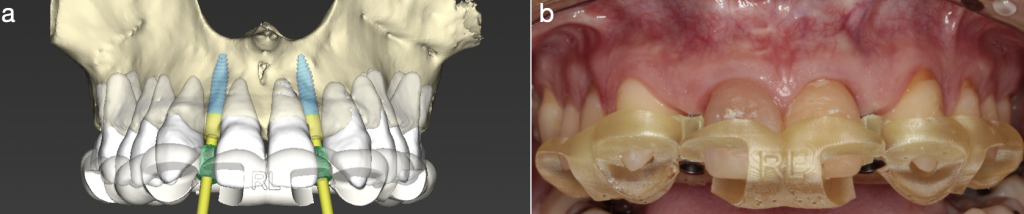
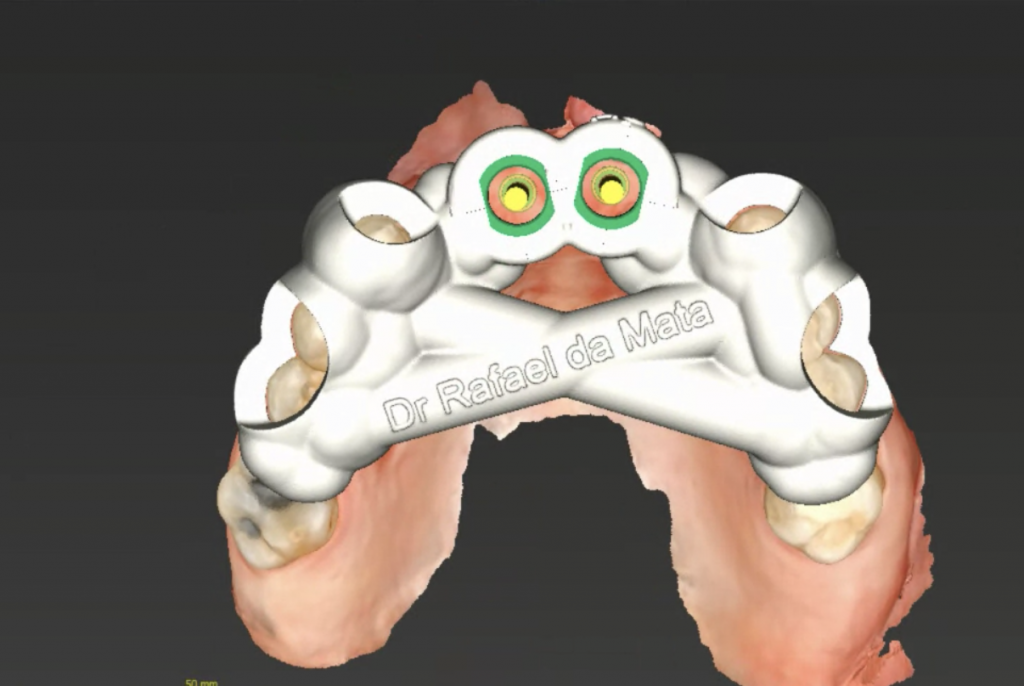
Inspection windows
Inspection windows serve as a valuable means of ensuring proper settlement and adaptation of the guide (El Kholy et al. 2019; De Souza et al. 2022). It is recommended to position them bilaterally to the implant site (Markovic et al. 2024), and, according to our experience, this resource also facilitates and enhances the visualization and access of the contra-angle during the osteotomy procedure in the region of interest. Additionally, it may be advantageous to place inspection windows both on the vestibular and lingual aspects of the guide (Fig. 2). However, caution should be taken to avoid overuse of this resource, thus preventing weakening of the template (Markovic et al. 2024). Despite literature reports that guide fracture is not a frequent occurrence (Pimkhaokham et al 2022), such a complication should be avoided as it can compromise the entire execution of the sCAIS protocol, which is a surgical-guide-dependent procedure. To address this issue with foresight, it is advised to ensure the proper passive fit of the guide before commencing the surgery (Tahmaseb et al. 2014; Chackartchi et al. 2022).
In fact, guide misfitting or inadequate stability is one of the most frequent complications in sCAIS (Pimkhaokham et al. 2022). Also, according to the literature, approximately 85% of guides exhibit good adaptation and stability (Mangano et al. 2018), and up to 50% may require some form of adjustment to enable their use (Peñarrocha et al. 2012). This issue could be attributed to guide deformation that may take place during the interval between the guide manufacture and utilization.
Guide deformation
Although there is no consensus on the ideal time between SG fabrication and its utilization (i.e., day of the surgical procedure), scientific evidence demonstrates that the SG is susceptible to post-manufacturing structural deformations over time (Lo Russo et al. 2022), which can ultimately compromise the adaptation and subsequent stability of the guide. In addition, the equipment used may also have an impact on the guide dimensional stability over time (Chen et al. 2019). Nevertheless, evidence suggests that if stored and maintained under appropriate conditions, the guide may undergo minimal alteration over a period of 14 days (Rios et al. 2023) to one month after fabrication (Chen et al. 2019).
Despite the evidence on the dimensional stability of the guide-post fabrication, its real impact on clinical practice remains uncertain. Nevertheless, it’s undoubtedly a matter worthy of attention in everyday clinical practice.
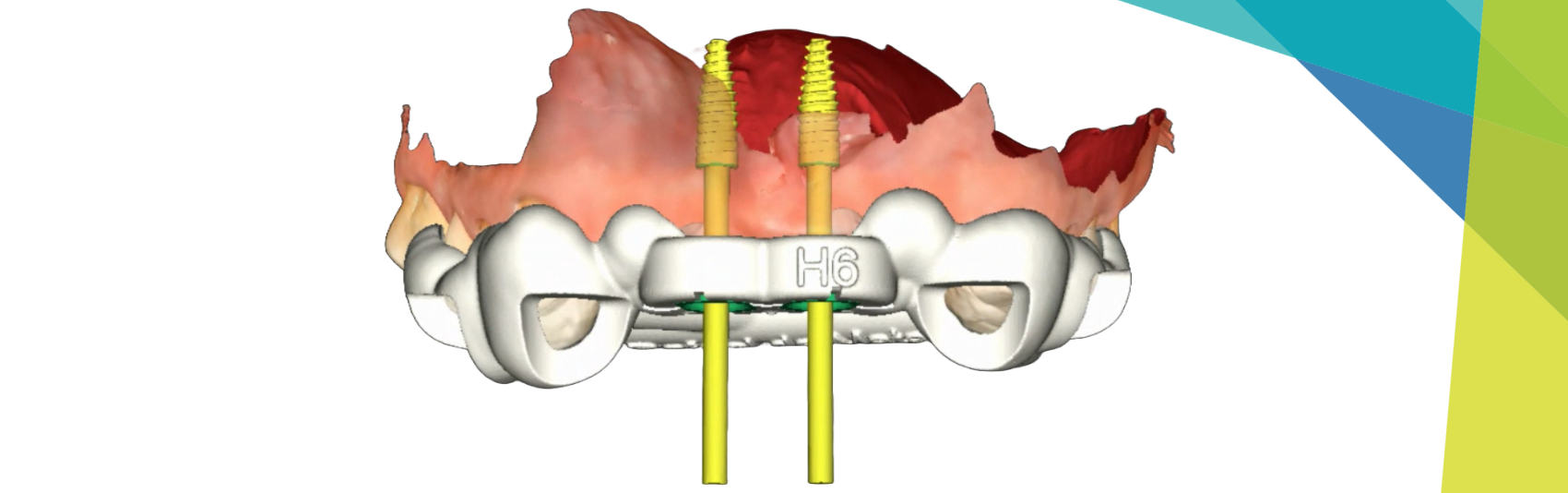
Bridging element
While consensus on this topic is also lacking, a bar or bridging element can be designed to connect the template laterally from one side of the arch to the other (Fig. 3). This design purportedly helps prevent distortion during the 3D printing process (Khalil et al. 2021; Lim et al. 2021), serves as reinforcement for the template (Torok et al. 2020), and may increase the SG stability during the surgical procedure. However, when designing a guide connecting both sides of an arch, attention should be given to the insertion axis, which should guarantee the fit of the guide on both sides. Inclined teeth and/or large interproximal spaces can hinder such characteristics.
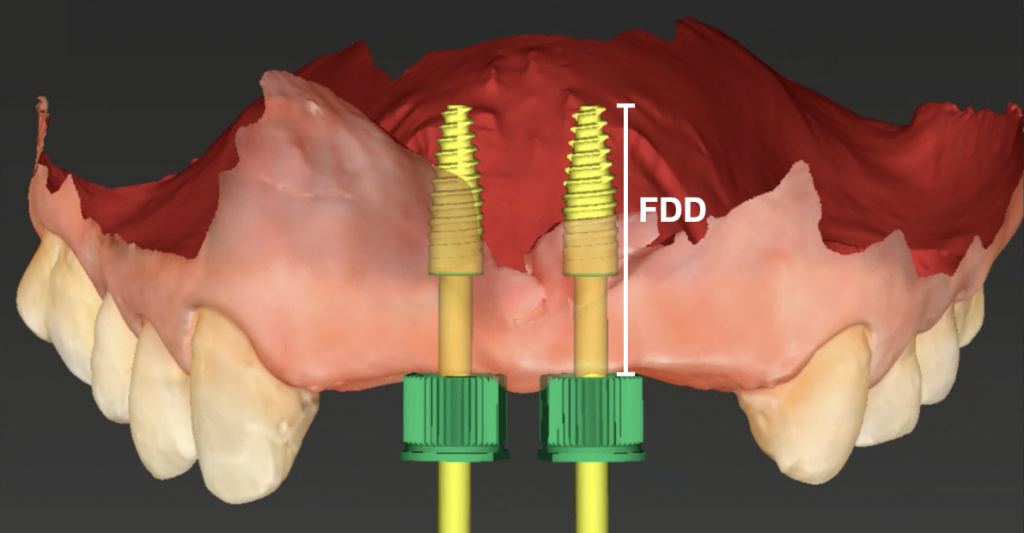
Sleeve height and guide-hole design
It is acknowledged that various guided implant systems exhibit different behaviors and precision levels (Guentsch et al. 2023). The height of the sleeve and related variables currently remain a topic of discussion. In a pre-clinical study, El Kholy et al. (2019) demonstrated that minimizing the free drilling distance (linear measurement from the bottom of the guided sleeve to the bottom of the osteotomy) can enhance the accuracy of sCAIS (Fig. 4). Accordingly, Guentsch et al. (2021) and Van Assche & Quirynen (2010) showed that the closer the sleeve is to the bone, the more accurate and precise sCAIS becomes. Other findings suggest that longer sleeve cylinders play a significant role in optimizing accuracy (Choi et al. 2004; Koop et al. 2013).
While most manufacturers’ systems recommend the use of sleeves, some studies have compared the accuracy between sleeve (S) and sleeveless (SL) guides, finding similar accuracy between the groups (Oh et al. 2021; Adams et al. 2023). In contrast, Raabe et al. (2023) and Dulla et al. (2023) reported higher accuracy in the SL group, potentially justified by the reduction of one gap (guide-sleeve) in the guide, resulting in two gaps (guide-key and key-drill) while S guides involve three gaps (guide-sleeve, sleeve-key, and key-drill). There is limited evidence to favor SL over S templates. Therefore, we recommend clinicians adhere to the manufacturer’s guidelines for better results, as suggested by Joda et al. (2018).
Material thickness and guide-to-tooth offset
To ensure mechanical strength and avoid complications, such as guide fracture, it is essential to have a minimum of material thickness. In stereolithographic (SLA) printing (refer to the production section below), surgical guide thickness ranging from 3.0 to 3.5mm is considered adequate for safe and effective sCAIS. A guide-to-tooth offset of 0.1-0.15mm is recommended to achieve an optimal guide-to-tooth fit (El Kholy et al. 2019; Wegmuller et al. 2021; Raabe et al. 2023; Dulla et al. 2023). According to Lim et al. (2021), setting the offset during the design process can improve the accuracy of the surgical template.
Production
Following the completion of computer-aided design (CAD), the production of the surgical guide through computer-aided manufacturing (CAM) takes place. Various 3D printing technologies and methods are available, each presenting distinct sources of errors and cost-effectiveness. The fabrication of a surgical template can be achieved using either additive or subtractive technologies (Bathija et al. 2023).
Additive manufacturing involves the process of joining materials to produce components based on three-dimensional model information, typically through the deposition of layers, creating personalized designs (Lim et al. 2021). The popularity of SLA printing, an additive manufacturing method, has risen among clinicians due to its cost-effectiveness and easy accessibility. A pre-clinical study revealed a statistically significant difference in implant positioning accuracy between SLA, fused filament fabrication (FFF), and digital light processing (DLP) printing methods. However, this discrepancy was deemed clinically negligible (Wegmuller et al. 2021). Accordingly, Herschdorfer et al. (2020) assessed the final implant position, comparing surgical guides manufactured with different printing technologies (SLA, PolyJet, and MultiJet), demonstrating clinically acceptable results across all groups. Moreover, Wegmuller et al. (2021) reported that, from a clinical perspective, consumer-level desktop 3D printers could produce guides of similar accuracy to a high-end professional 3D printer.
Considering the established reliability of desktop printers and the widespread use of SLA in daily practice, the choice of resin must prioritize biocompatibility in alignment with ISO standard 10993 for the biological evaluation of medical devices (Elliot et al. 2022). The selected material should also exhibit qualities such as translucency to enhance visualization during procedures and dimensional resilience to withstand pressure, heat, and steam, allowing the sterilization of the template in an autoclave (Torok et al. 2020; Sharma et al. 2020; Elliot et al. 2022), although other effective sterilization/disinfection methods, such as plasma sterilization, are also available (Torok et al. 2020). It’s worth noting that the market offers resins developed specifically for surgical guide printing.
Take-Home Messages
Each step of virtual surgical planning is of utmost importance to the success of sCAIS. Specifically for guide design, key factors must be taken into consideration to minimize the chances of deviation between the virtually planned and the inserted implant. Most of them may be automatically set up depending on the software used, however the clinician should understand their relevance to sCAIS accuracy and clinical outcomes. We can consider:
- Assess guide support carefully, considering additional fixation methods, such as pins and screws, to ensure proper retention.
- Inspection windows are valuable resources to ensure settlement and adaptation of the surgical guide.
- A bridging element can be useful to provide the guide with more stability and attenuate distortion during the printing process.
- It is advisable to follow the system recommendations regarding sleeve or sleeveless guides.
- Reduction of the free drilling distance is beneficial in terms of accuracy.
- Prolonged interval between the production and utilization of the surgical guide may produce a dimensional distortion, impacting guide fitting and reliability.
Conclusion
Meticulous adherence to a precise protocol from data acquisition to surgical execution is paramount to achieving the high accuracy guided surgery is reported to provide. This article underscored the role of guide design, emphasizing key variables. By comprehensively addressing these factors, the user should be able to ultimately enhance sCAIS outcomes.