Introduction
Patient-centered treatments are at the core of how we approach treating our patients, and with developments in technology there are viable alternatives to major augmentation. In implant-supported reconstructions, if we have the ability to avoid large invasive procedures without compromising biological principles while minimizing morbidity, then this modality can be used to rehabilitate patients. The case report below outlines how a multidisciplinary treatment approach and utilization of the implant portfolio available today can achieve good results for patients while reducing invasiveness.
Initial presentation and periodontal treatment
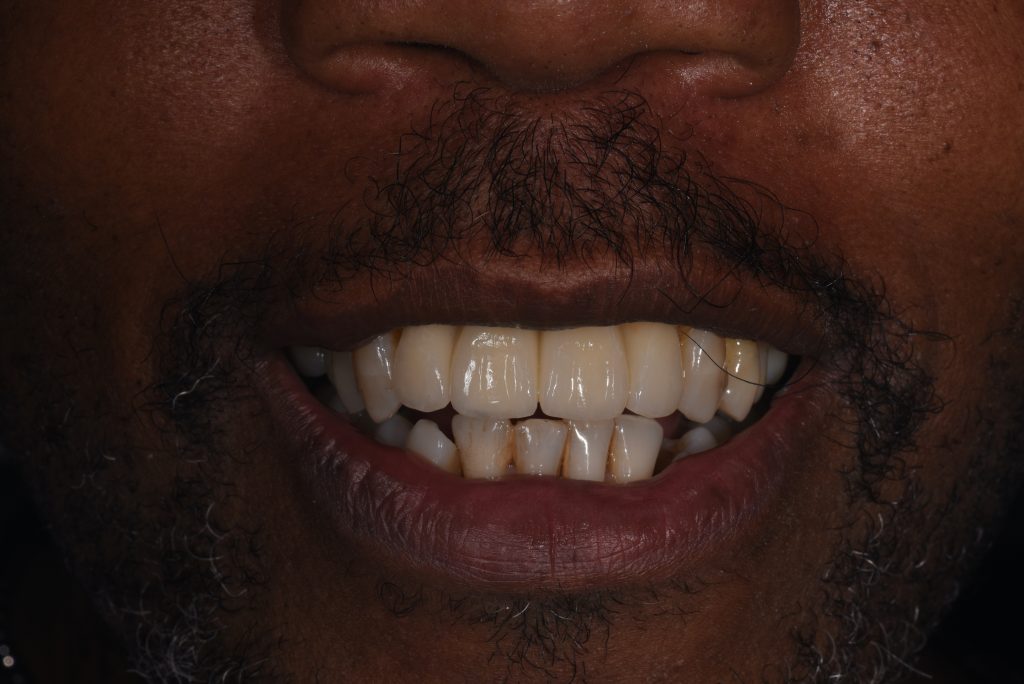
A 57-year-old man with no contributory medical history presented at the clinic, complaining of significant gingival recession and tooth mobility. Clinical and radiographic examination revealed up to 90% bone loss in certain areas (Figs 1 – 2).
Generalized stage IV grade C periodontitis was diagnosed (Papapanou et al. 2018). The initial treatment plan included non-surgical periodontal treatment and re-assessment. At re-assessment, several teeth still had probing pocket depths of >5 mm with bleeding upon probing. Therefore, a surgical periodontal therapy plan was created which involved resective periodontal therapy, including furcation tunneling of teeth #46 and #36. The lower anterior teeth were splinted with a fiber-reinforced composite splint. The maxillary anterior incisors had a poor periodontal prognosis and would be extracted and replaced with implants. The treatment aimed to ensure no pockets of >5 mm depth at the time of implant placement (Lee et al. 2012).
An immediate acrylic partial denture was made, ensuring there would be adequate tooth support since it could also be used during any implant healing stage (Fig. 3).

By this stage of the treatment, the patient had shown very good oral hygiene compliance and the periodontal tissues showed a good response to the treatment. It was decided to replace the four missing maxillary incisors with an implant-supported fixed dental prosthesis (ISFDP). Although a history of periodontitis is not a contraindication for implant placement, patients with such a history should be made aware of the higher biological risks for implant failure (Heitz-Mayfield & Huynh-Ba 2009). Successful periodontal treatment and patient compliance are key, as a history of periodontal disease is a risk factor.
ITI Academy Learning Pathway: Local and Systemic Risk Factors for Implant Therapy
ITI Academy Learning Module: Transitional Prostheses Used During Implant Therapy
Implant planning and placement
Following the extractions, a healing time of around 6 – 8 weeks was proposed to allow soft tissue closure of the sites (Figs 4 – 5).
A CBCT scan was performed to visualize the anterior bone volume alveolar process (Bornstein et al. 2017). The CBCT was combined with a digital wax-up of the ideal position of the teeth in implant planning software. The wax-up copied the size and position of the denture teeth with which the patient was happy. The radiographic assessment revealed that the patient had an abundance of maxillary alveolar bone in height and width. A Type 2C placement protocol was proposed due to the short roots and abundance of apical bone available to gain adequate primary stability of the implants (Gallucci et al. 2018).
The anterior alveolar process was proclined to the extent that prosthetically-driven implant placement for an implant level, screw-retained ISFPD would necessitate extensive bone grafting. It was decided to place the implants with their long axis towards the incisal edge of the proposed tooth position and correct this by using multi-unit abutments with 17-degree angulation (Fig. 6).
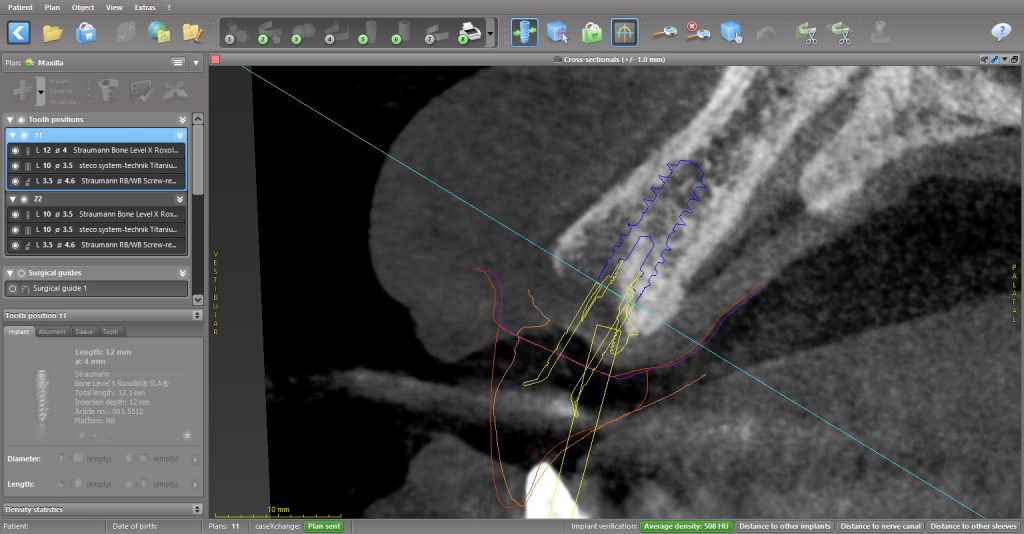
When using two implants to replace four missing maxillary incisors, the best implant configuration seems to be to place the implants at the lateral incisor sites, one at a lateral incisor site and one at a central incisor site. This configuration avoids having two implants adjacent to each other and allows shaping of the soft tissue at the pontic sites (Vailati & Belser 2007). In this case, the plan involved placing two Straumann BLX implants at positions #11 and #22 and connecting two Straumann SRA multi-unit abutments with 17-degree angulation on the day of the surgery. A surgical guide was designed and printed, allowing a fully guided approach to the surgery to ensure maximum implant placement accuracy (Tahmaseb et al. 2018).
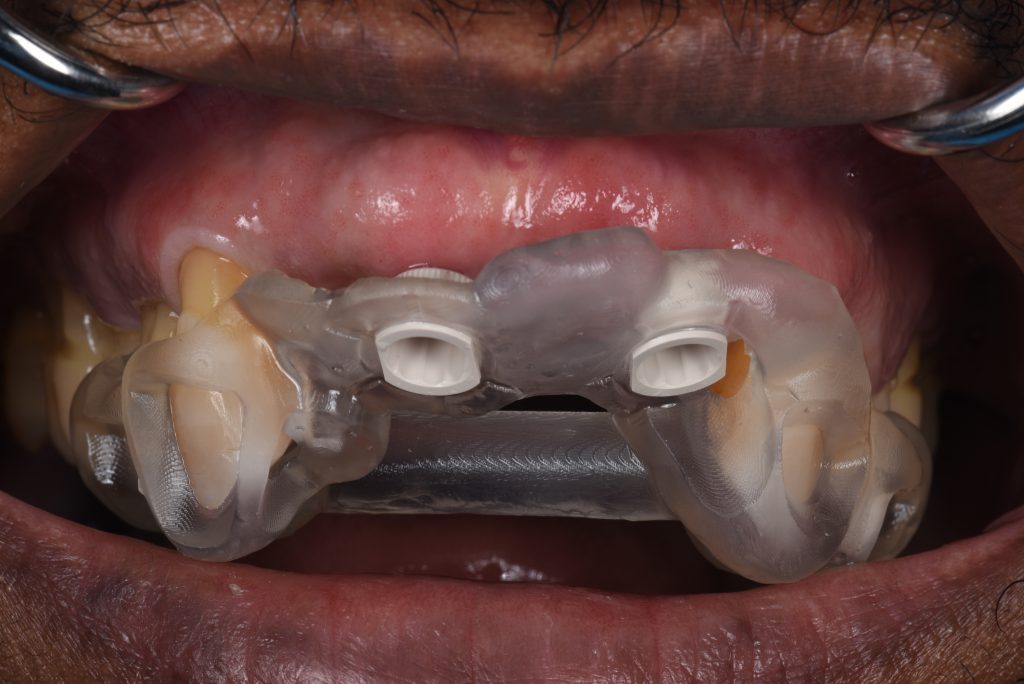
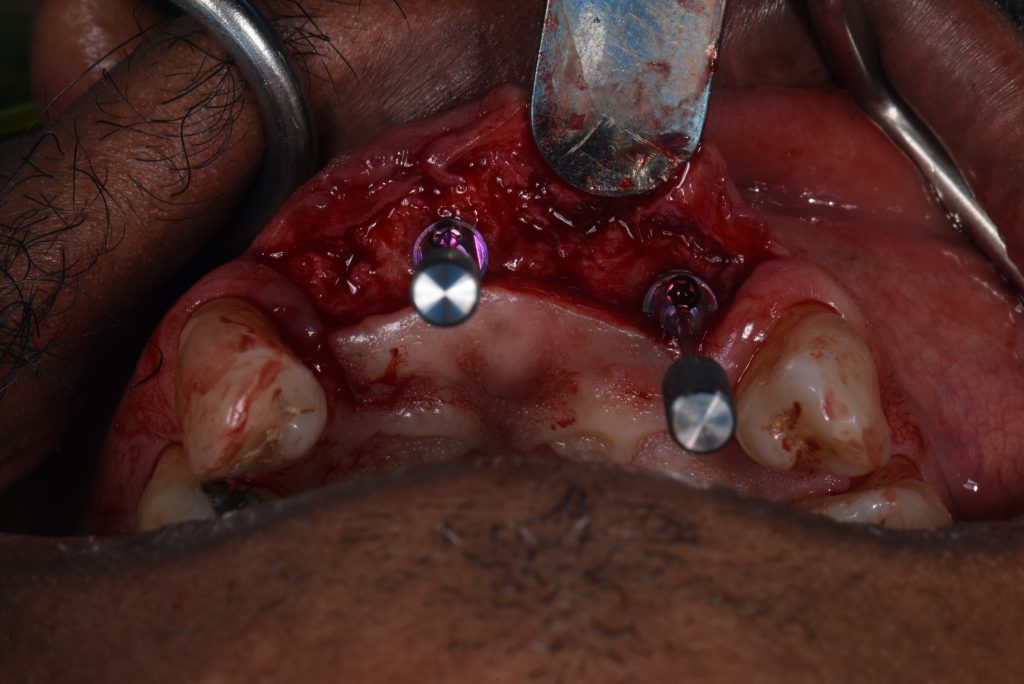
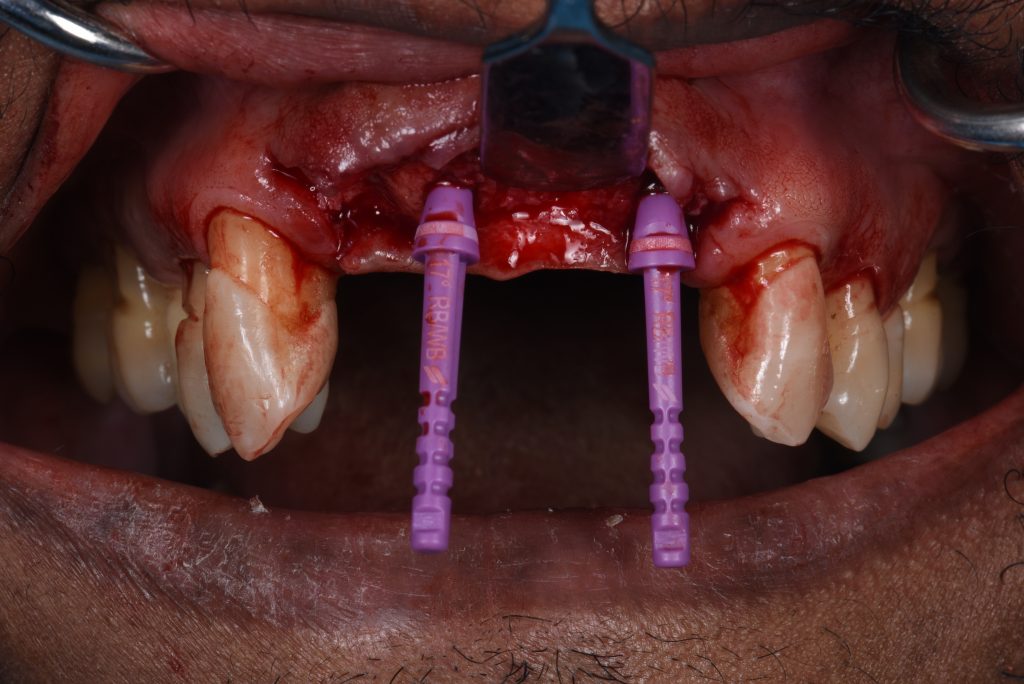
The implant surgery involved a flap design with mini papilla-sparing incisions mesial to the maxillary canines and placement of the implants at the pre-planned positions with the aid of two surgical guides. The first guide was a pilot-driven guide with longer sleeves. These types of sleeves allow for accurate initial osteotomy preparation to the bone in partially healed sites (Figs 7 – 9).
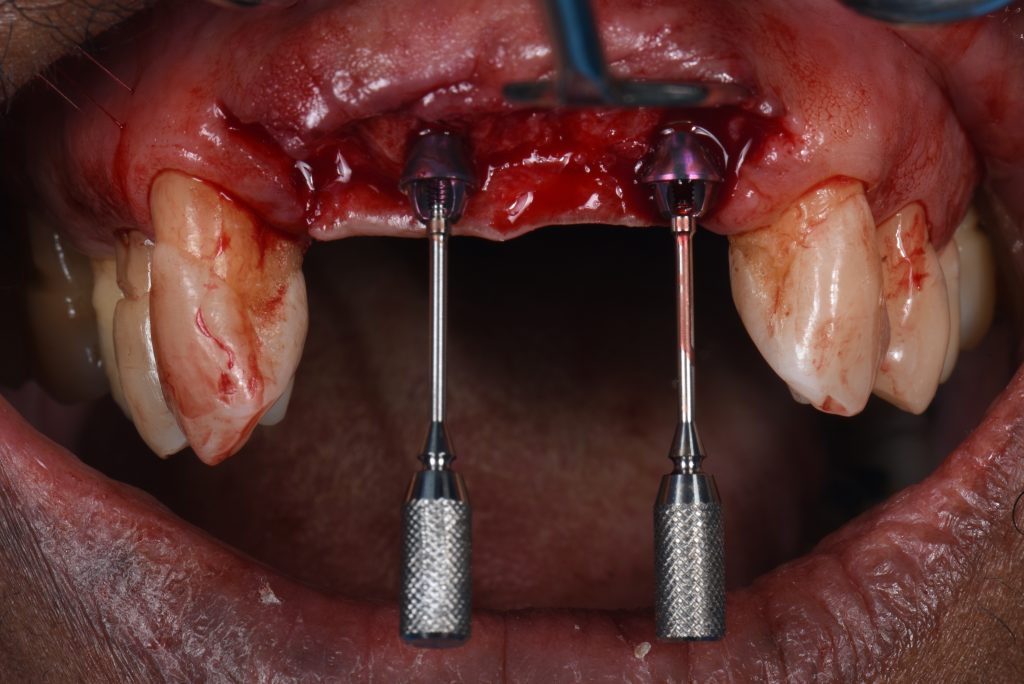
A second, more conventional guide utilizing the Velo drills from the Straumann BLX guided surgery kit was used to complete all osteotomy preparations for the insertion of the implants.To ensure that the long axes of the definitive multi-unit SRA abutments would be parallel, plan abutments were used to confirm their position (Fig. 10).
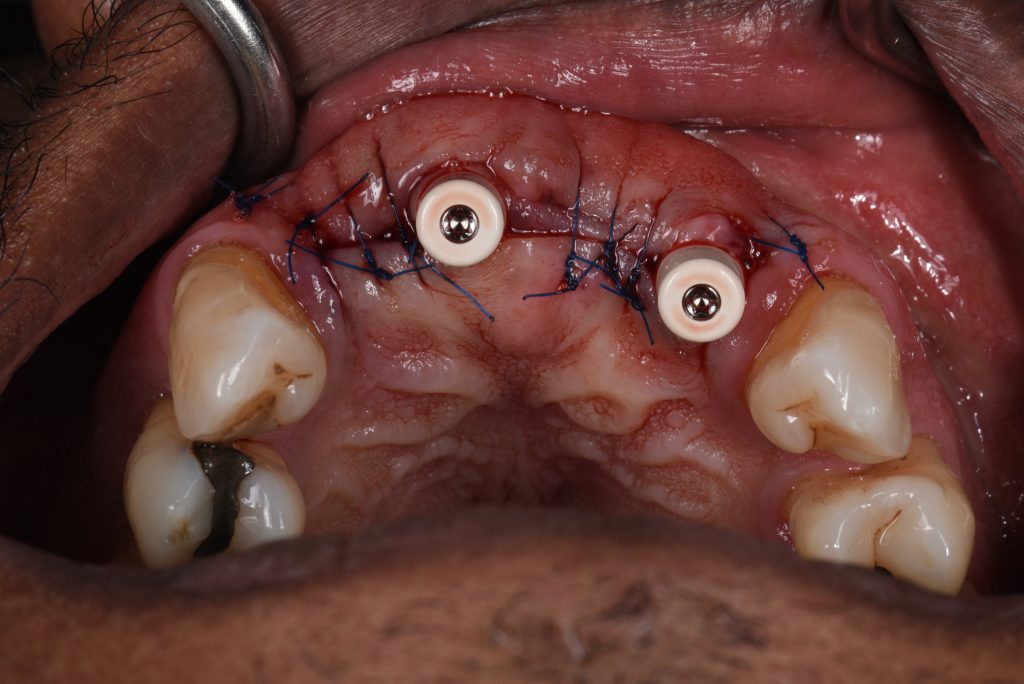
These plan abutments show if any further rotation of the implants is needed at this stage to achieve parallelism. Furthermore, the desired gingival height of the abutments can be confirmed. The multi-unit abutments were torqued to their definitive value to aid the one-time concept which helps to ensure the soft tissue seal around the implants remains undisrupted during healing and also during the prosthodontic phases (Pelekanos & Pozidi 2017). Connection of the abutments to the final torque was possible since the initial implant primary stability achieved was in excess of 35 NCm2, and the ISQ reading of the implants was more than 70 (Gallucci et al. 2018) (Figs 11 – 12).
Since in this case it had been decided to load conventionally (Ganeles & Wismeijer 2004), healing caps were connected (Fig. 13) and the patient wore a removable vacuum-formed retainer with composite pontic teeth for two weeks (Fig. 14). This ensured that no pressure was applied on the surgical site and after suture removal the patient continued to wear his removable denture after it was adjusted and relined with a soft lining material.
Prosthodontic stages
Three months following implant placement, an abutment level impression was made to construct a screw-retained provisional prosthesis (Fig. 15). Such provisionals can be made from a composite or acrylic material and this means the clinician can easily add or remove material as needed in order to shape the ideal soft tissue architecture (Fig. 16).
ITI Academy Learning Pathway: Soft Tissue Management Using Implant-Supported Provisional Prostheses
After several weeks of the provisional ISFDP in situ, the esthetic and functional parameters were confirmed, and a second abutment level open tray impression was made to produce the definitive prosthesis (Kim et al. 2015). The soft tissue architecture at this stage is captured to be transferred to the definitive restoration (Papadopoulos et al. 2014), and the shape of the prosthesis should be a copy of the approved provisional. A verification jig was manufactured (Fig. 17) to confirm the accuracy of the impression (Ercoli et al. 2012), followed by fitting of a screw-retained zirconia ISFDP (Figs 18 – 21).
A number of studies have established that zirconia implant-supported fixed dental prostheses perform well, with high success rates ranging between 93 – 100%. The incidence of chipping can be reduced by using fully monolithic restorations or a design where the occlusal guidance is kept on the monolithic part of the restoration. Case selection and correct prosthesis design are crucial; in this case the anterior open bite and lack of parafunction made minimal buccal porcelain layering a safe choice. Although research suggests that metal-ceramic is still the gold standard for multiple-unit, implant-supported FDPs, emerging good quality evidence supports the use of zirconia as a material (Sailer et al. 2018; Laumbacher et al. 2021).
The use of multi-unit abutments has the advantages of shifting the slim prosthetic platform more coronally, thus not disturbing the supracrestal complex (Mattheos et al. 2021), and making prosthetic procedures easier for the clinician and more comfortable for the patient. Also, with their use it is easier to achieve a passive fit of the prosthesis, and the angle correction options allow for screw-retained access. On the other hand, although the use of multi-unit abutments is well-established in implant-supported fixed complete dental prostheses (Papaspyridakos et al. 2020, Balshi et al. 2014), it is less documented in partially edentulous situations as in this case. Further studies are required, investigating the long-term performance of this treatment modality.
The one-year review following delivery of the screw-retained zirconia prosthesis showed optimal functional and esthetic integration (Figs 22 – 24).
The patient was extremely satisfied and very motivated, with excellent oral hygiene. The patient was also placed on a 3-monthly recall for lifelong supportive periodontal therapy. A regular record of the patient’s plaque and bleeding score as well as a six-point pocket chart will be performed at each visit (Monje et. al 2016).