Introduction
Fully edentulous patients with severely resorbed ridges and unfavorable jaw relations often encounter difficulties with their conventional denture due to an impaired load-bearing capability, especially in the lower arch. Implant-retained overdentures (IODs) were proposed as an effective treatment for rehabilitating such patients to restore both function and esthetics and increase patients’ level of satisfaction. (Akoglu et al. 2011; Balaguer et al. 2011). According to the McGill consensus of 2002, a 2-implant retained overdenture should be the minimum treatment offered to patients for treating an edentulous mandible (Feine et al. 2002; Thomason et al. 2009). Some authors also suggested rehabilitation with single implant mandibular overdentures as a therapeutic alternative for elderly patients experiencing discomfort and functional difficulties with conventional mandibular overdentures since several prospective studies showed that it does not differ significantly from 2-implant-retained overdentures and is easier for elderly patients to remove (Srinivasan et al. 2014; Passia et al. 2015; Passia et al. 2015). However, 1-IODs require more long-term studies and a larger range of prosthodontic, functional, and patient- related outcomes . Despite the disadvantages of IODs compared to an implant-supported, fixed dental prosthesis, IODs are easily cleansable for elderly patients, require fewer implants, and are relatively lower in cost when compared with fixed reconstructions (Borges et al. 2020). IODs are an assembly of different components: the denture, mucosa, bone, implant, and attachments. Several attachments exist, each of which has a different stress-bearing capacity and strain tolerance, with the Locator attachment being the most popular type currently used for restoring mandibular overdentures. During oral function, IODs are subjected to a variety of forces in different directions, exerted along the hinge axis representing the fulcrum line of the attachments (Tokuhisa et al. 2003). Retention provided by these attachments to resist withdrawal along the path of insertion results in lateral forces around the attachment assemblies and implant during function, leading to several mechanical and biological complications (Yang et al. 2011). Such lateral dislodging forces are affected by several factors including implant position, implant angulation, implant depth, and attachment height (Balaguer et al. 2015). This article summarizes these influencing factors, which, if well-controlled, can increase the long-term survival of IODs, decrease their need for maintenance, and enhance patient satisfaction. The article concludes with clinical tips and recommendations to ensure predictable results.
Factors affecting the long-term success rate of mandibular implant overdentures
Implant-related factors (ITI Treatment Guide 9, chapter 8)
a. Position of implants
As bone resorption occurs, the residual mandibular ridge may affect the availability of locations for implant placement (Swasty et al. 2009), which, in turn, may affect surgical planning and treatment outcomes. The possible locations of implant placement in 2-IODs have been suggested in the lateral incisor, canine, and premolar regions, with controversy remaining as to which location is the most advantageous. Studies advocating for implant placement in the canine or lateral region report advantages of bone preservation and a decrease in marginal bone loss (Elsyad et al. 2018; Elsyad et al. 2016). On the other hand, when implants are placed in the premolar area, the fulcrum line upon which overdentures usually rotate is moved more posteriorly, often increasing the “seesaw effect” (Hong et al. 2012), and consequently transmitting the load to the implants. This is less evident in the canine and lateral zones. Another reason for increased bone loss around implants in the premolar position is the proximity of the implants to the first molar area in which edentulous patients often exert the maximum occlusal forces due to contraction of the levator muscles (Sadowsky et al. 2004). When deciding on whether to choose the lateral or canine position, the practitioner should evaluate the amount of bone available in both positions, which are usually greater in the canine region. Moreover, if the patient wishes to later upgrade the restoration from a mandibular overdenture to a fixed prosthesis, such as an all-on-four concept, it’s more favorable to place the implants in the lateral incisor area.
b. Parallelism of implants
The prosthetically desired implant inclination or position may not be clinically achieved due to the morphology of the present bony tissues, anatomical structures, or limited surgeon experience. Implants should ideally be positioned parallel to each other and as perpendicular to the occlusal plane as possible to attain uniform stress distribution, a factor critical in maintaining peri-implant bone level (Elsyad et al. 2017 a,b), and to reduce lateral or axial forces, (Mericske-Stern et al.1993) which could increase mechanical risks on IODs such as loosening of the attachment, and fracture of the attachment assemblies (Yang et al., 2011; Stephens et al., 2014).
A study by Patil et al. evaluating the stress and strain distribution patterns under unilateral and bilateral loading in 2-mandibular IODs with different positions and angulations of implants concluded that implants placed with a higher degree of angulation resulted in the highest level of stress (Patil et al. 2022). The authors also reported that minimum changes in the stress values were observed in the denture and supporting mucosa, and maximum changes were seen in the bone and implants. This increase in stress levels consequently poses a higher risk to the implant and the attachment components when implants are not placed in a parallel configuration (Patil et al. 2022).
c. Height of locators and implant depth
The height of the attachment has a major effect on both the lateral forces transmitted to the implant and on denture displacement. Ying et al. reported that attachments with lower heights transmitted a smaller lateral force to the implant and resulted in less denture displacement (Ying et al. 2017). The practitioner’s choice when selecting attachment height is affected by several factors including the implant depth, gingival height, and vertical space. Placing the implants at different depths makes it harder for the practitioner to correct this mis-leveling using different locator heights. An uneven level of 2 Locator abutments might also produce a rotational path of dislodgement resulting in a higher level of cumulative tensile forces, which could then be transferred to the implant and result in unfavorable stresses on the implant and surrounding alveolar bone (Sia et al. 2017). Therefore, implants should be placed at the same or similar crestal level to prevent a mismatch in locator height.
Although a direct relation between implant depth and tissue thickness has not yet been established, a thicker mucosal lining demands the use of high collar attachment. Thus, practitioners should nevertheless attempt to place implants at equal depths to avoid varying levels of tissue thickness at the prosthetic phase. In addition, a critical consideration when case planning an attachment overdenture is vertical space known to be an average of 8.5 mm with locator attachments (Ahuja et al. 2010) and 12-14 mm for bar attachments (Carpentieri et al. 2019). The difference between the prosthetic space needed for locator and bar attachment is demonstrated in Tables 1 and 2 and Figure 1.
| Locator attachment (mm) | |
| Thickness of soft tissue | 1-2 |
| Locator + housing | 2.5-3 |
| Acrylic denture base | 2.0 |
| Tooth | 3.0 |
| Total height requirement | 8.5-9 |
| Bar attachment (mm) | |
| Thickness of soft tissue | 1-2 |
| Hygiene space under bar | 1-2 |
| Thickness of bar | 4.0 |
| Clip and housing | 1.5 |
| Acrylic denture base | 2.0 |
| Tooth | 3.0 |
| Total height requirement | 12-14 |
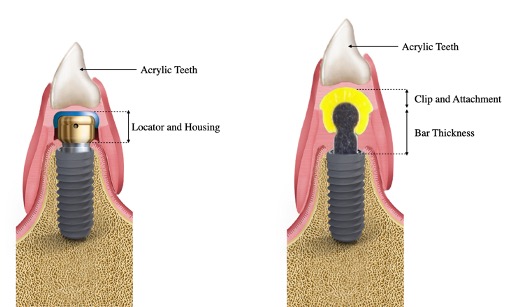
Adequate space is required to allow room for the acrylic base, denture tooth, and the metal reinforcement over the assembled complete attachment and housing.The locator attachment height is divided into two parts: a cuff height which is generally chosen according to the available gingiva height and a male seating working area height standardized to be 1-1.5 mm as shown in Figure 2.
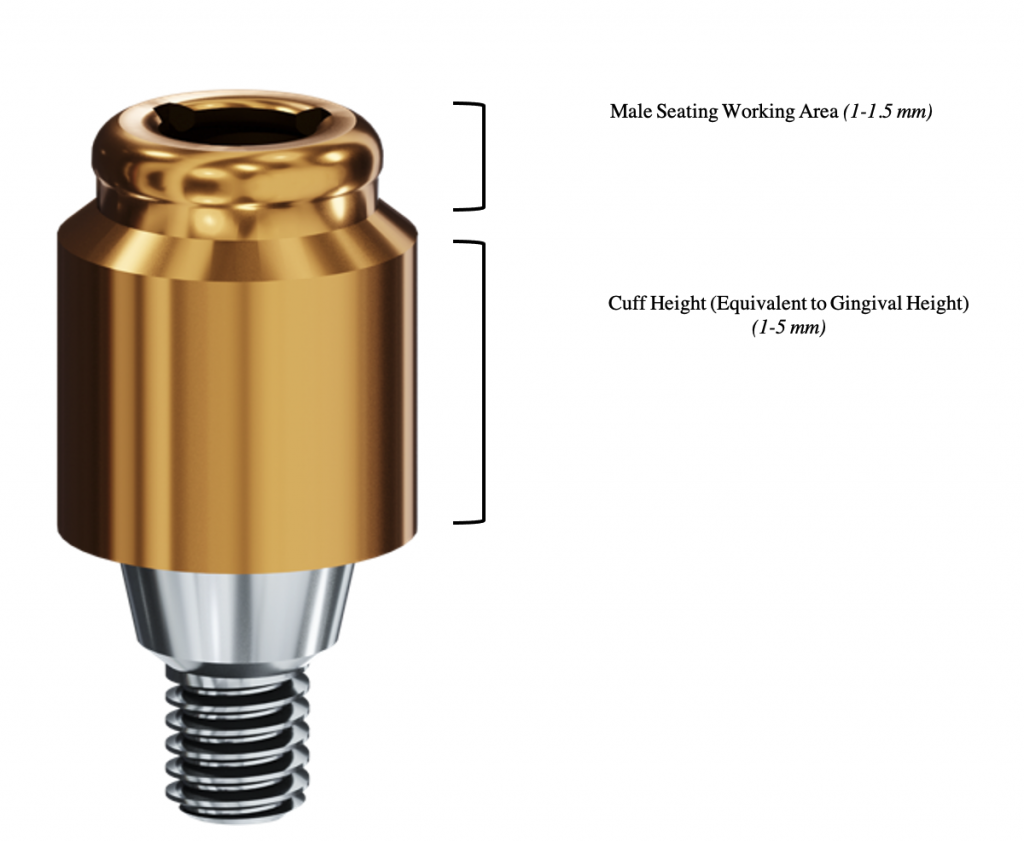
For example, selecting a locator attachment with an excessive vertical cuff height that is more than the actual gingival height can result in an inadequate thickness of acrylic resin in the anterior portion of the overdenture and an over- or under-contoured restoration with weak areas subject to breakage.This will often result in a potentially reduced longevity of the prosthesis, which can be frustrating for the patient.
Prostheses-related factors
a. Reinforcement of the overdenture prosthesis
Metal reinforcement has been advocated as a technique to decrease complications like fractures or cracks in IODs. This reinforcement should be fabricated at a level where it will not interfere with the attachment components. It is also imperative to select a suitable site to install the metal reinforcement to prevent excessive bulk to the denture base which can affect esthetics and/or phonetics unfavorably (Rodrigues et al., 2000).
b. Maximum area of support
Since an IOD is supported by both tissue and implant, appropriate extensions to the primary and secondary stress-bearing areas in the mandible provide posterior support and resist occlusal forces exerted on the posterior lever arm. Adequate flange extensions especially to the buccal shelf area are also required to seal and prevent food impaction and provide facial support (Lee et al. 2006).
Importance of computer-aided implant placement in IODs
Advancement in radiographic 3-dimensional imaging techniques and computer technology has made a breakthrough in accuracy and precision in implant placement in the past decade. Computer-aided implant placement techniques allow the visualization of implant position in terms of anatomical and prosthetic parameters using computed tomography and 3D implant planning software. Together with advances in computer-aided design/computer-assisted manufacturing (CAD/CAM) techniques, planned implant positions and digital data can be transferred to the actual clinical setting using computer fabricated guides for static computer-aided implant placement (sCAIP) (Jorba-García et al. 2021). However, there is also the option of dynamic computer-aided implant placement (dCAIP), where real-time tracking of implant placement can be performed with markers and a tracking device (Jorba-García et al. 2021). In IODs, achieving proper implant position, angulation, and depth can be safeguarded by using either sCAIP or dCAIP. Even if the practitioner is very experienced, the relatively restricted space of the oral cavity can limit the possibility of placing implants in the desired location and inclination.
Clinical case
The case presented here demonstrates the importance of utilizing surgical guides to achieve (Patil et al., 2022) optimum results in IOD cases. A 60-year-old male presented himself to the clinic complaining of his lower non-retentive denture. After proper clinical examination and assessment of the case, the possible treatment options were then discussed with the patient, listing the advantages, disadvantages, and risks of each option. The patient chose to receive 2 implants on the mandibular arch with 2 locator attachments. The patient was a non-smoker, with a clear medical history, no active dental disease, and no contraindications to implant therapy.
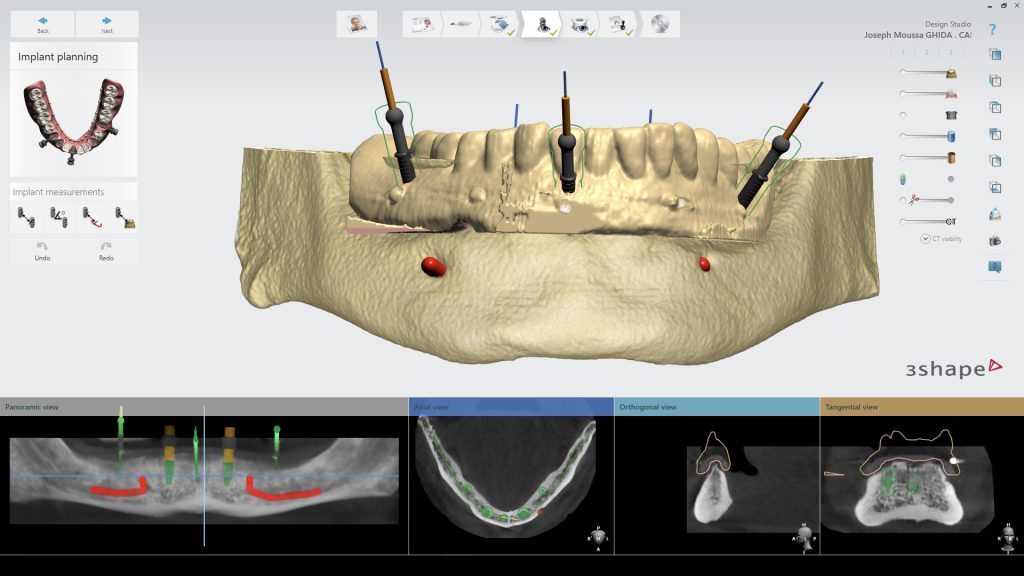
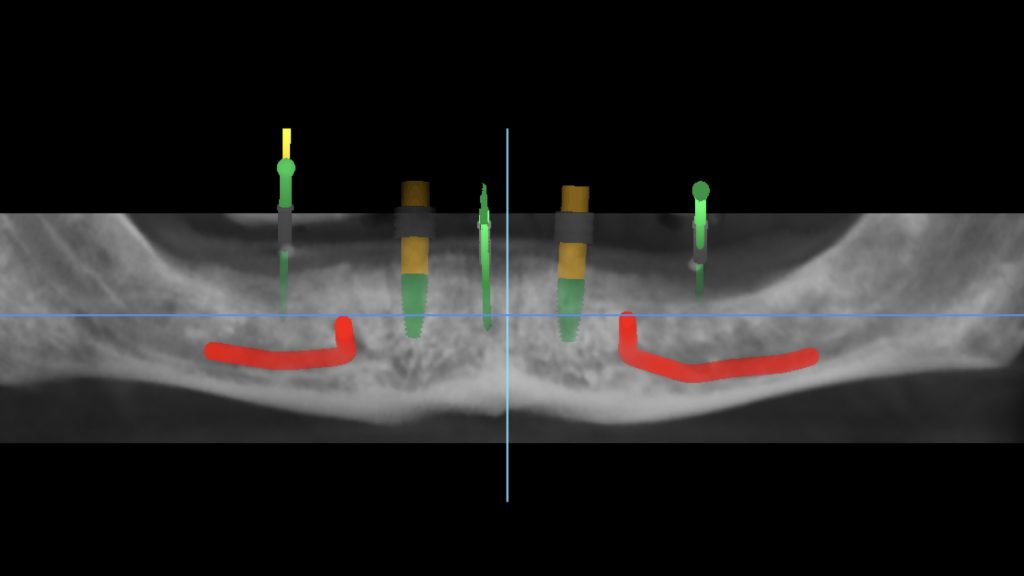
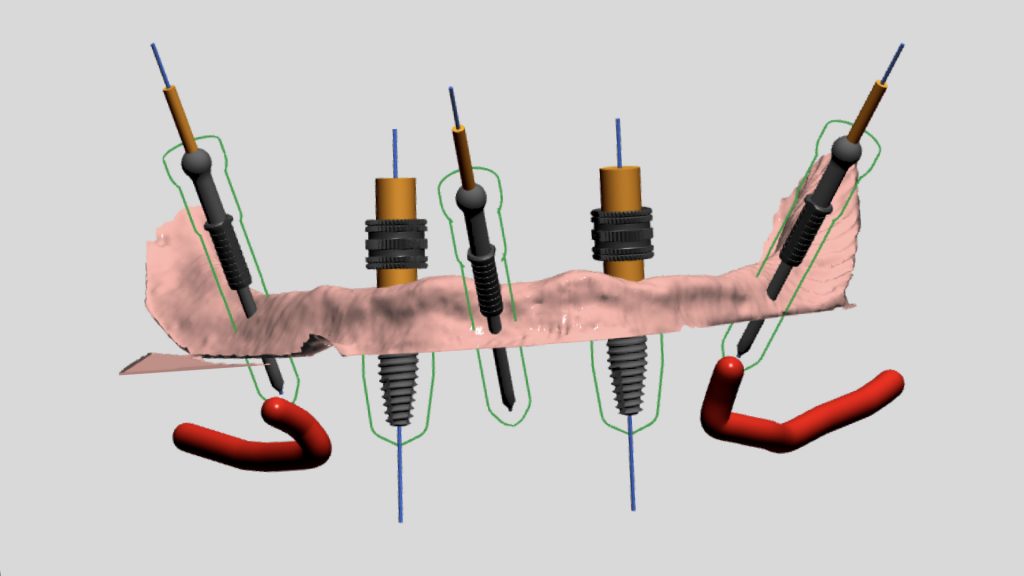
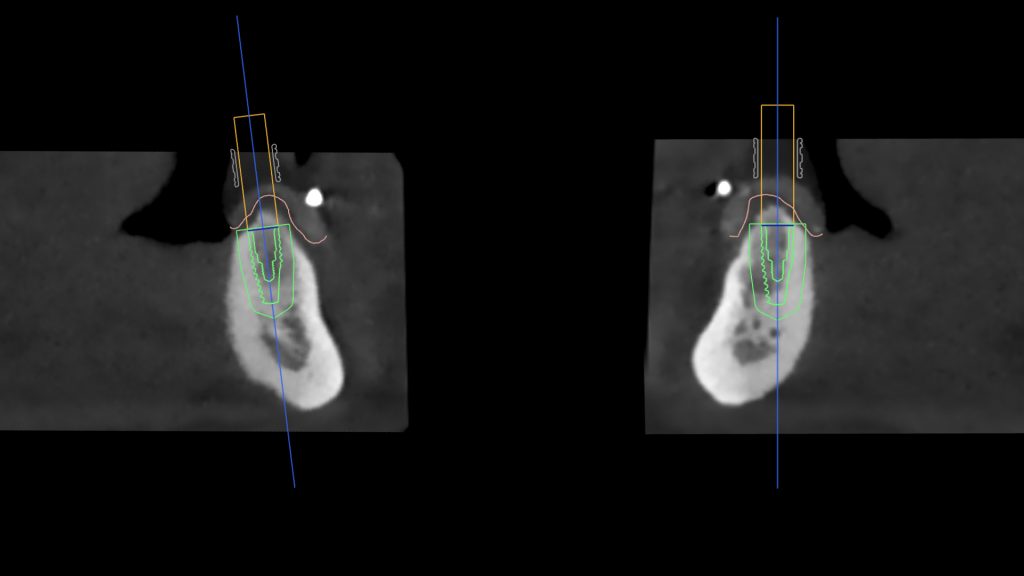
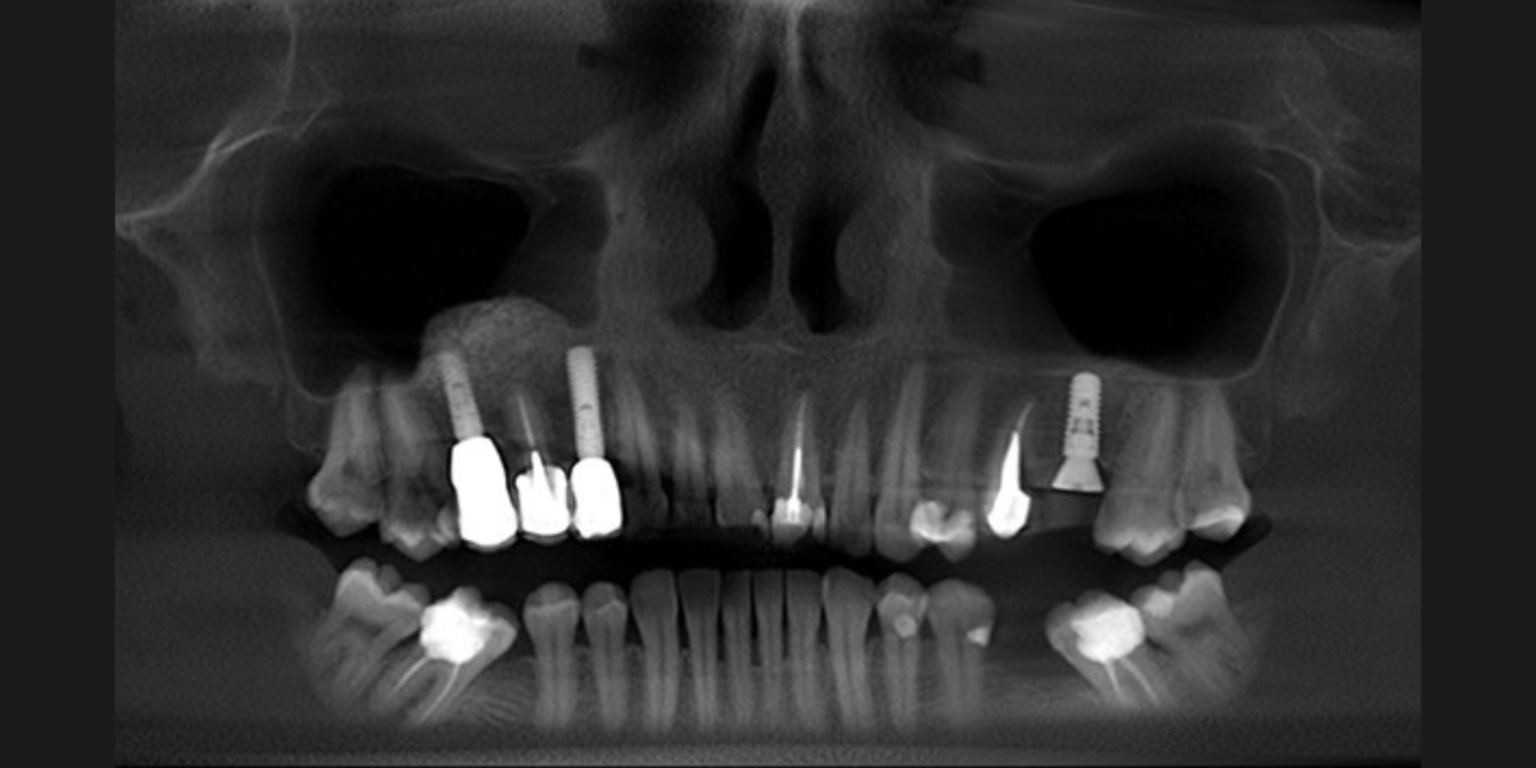
First, a dual-scan protocol was applied for the fully edentulous patient to receive 2 implants for locator attachments in the mandibular arch (Resnik et al. 2016) (Fig. 3). This protocol involves a 2-step scanning process where the first CBCT (NewTom GiANO HR 3D CEPH – CBCT Machine, Newtom) is for the patient’s denture with radiopaque markers and the second CBCT is for the patient while wearing the denture/radiographic guide. These two scans are obtained to superimpose the two files over each other using the radiographic markers as a reference, resulting in a model of the patient’s bone together with the denture (Fig. 4). The scans were then imported into a planning software where the position and orientation of implants were determined with a prosthetically-driven concept (Figs 5-7).
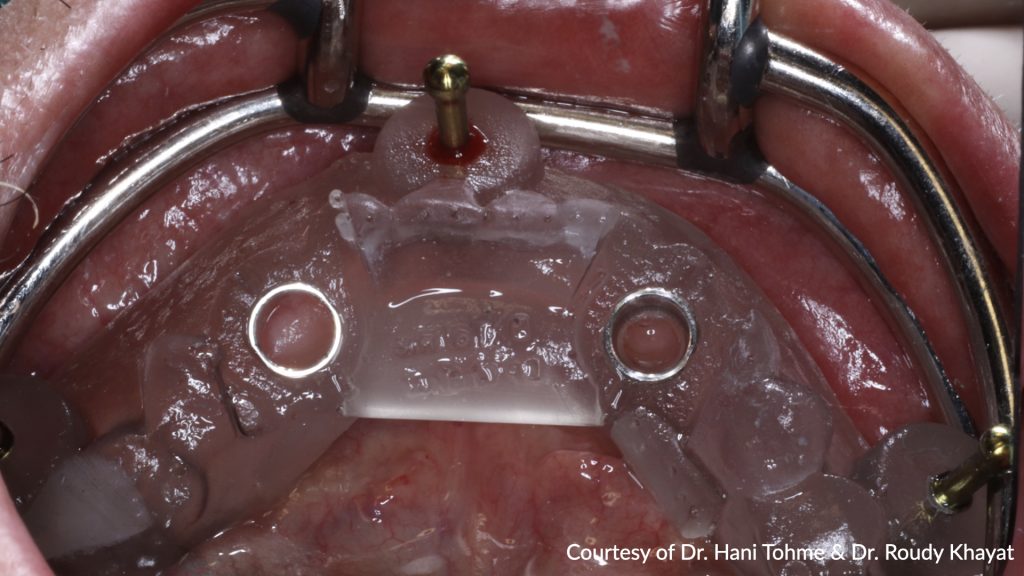
A surgical guide was designed (Implant Studio, 3Shape), exported to the printing machine (NextDent 5100, 3D systems), and fabricated using resin for surgical guides (Fig. 8). Subsequently, the guide was inspected and fixed in place with fixation screws to stabilize it in place (Fig. 9).
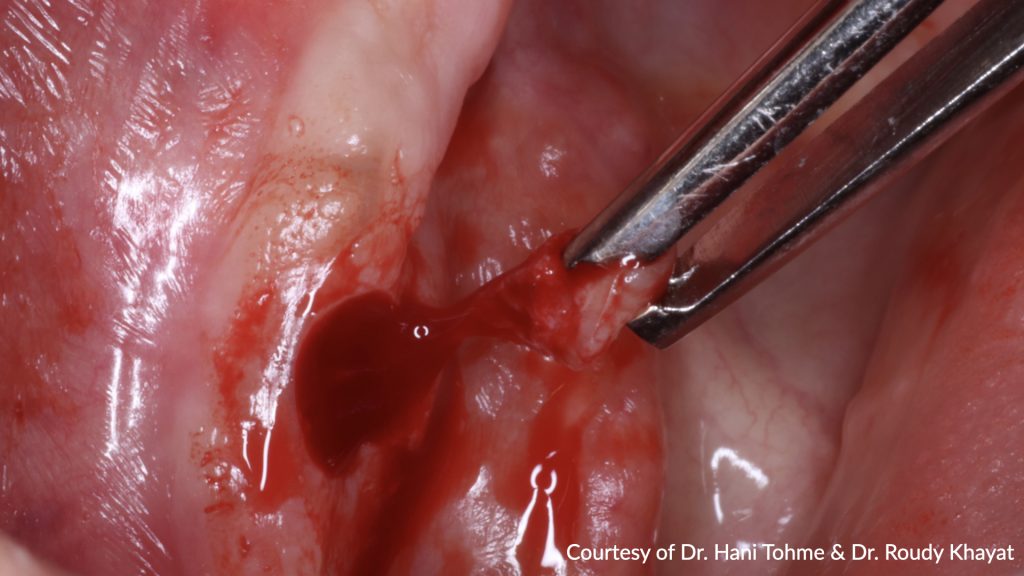
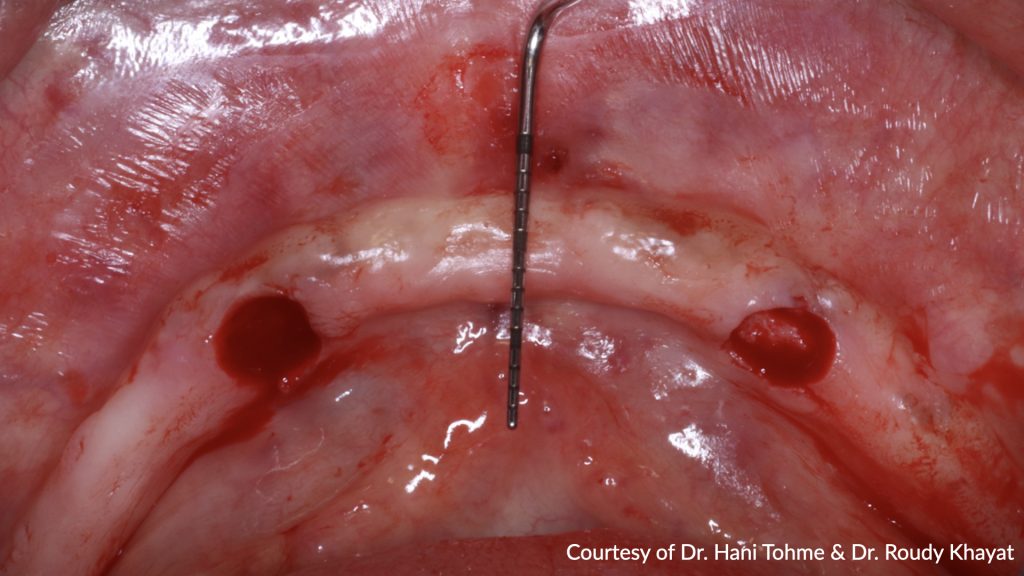
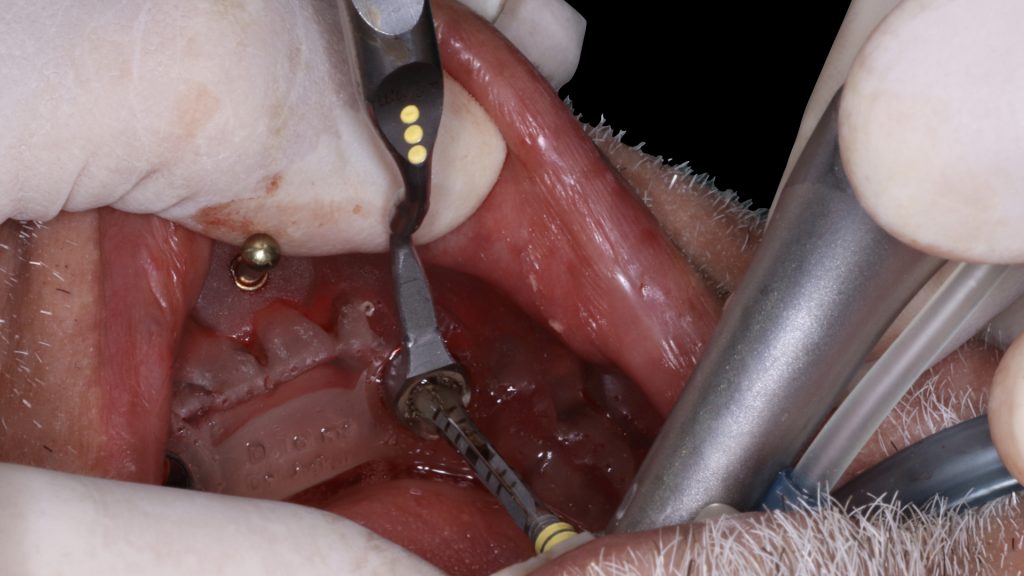
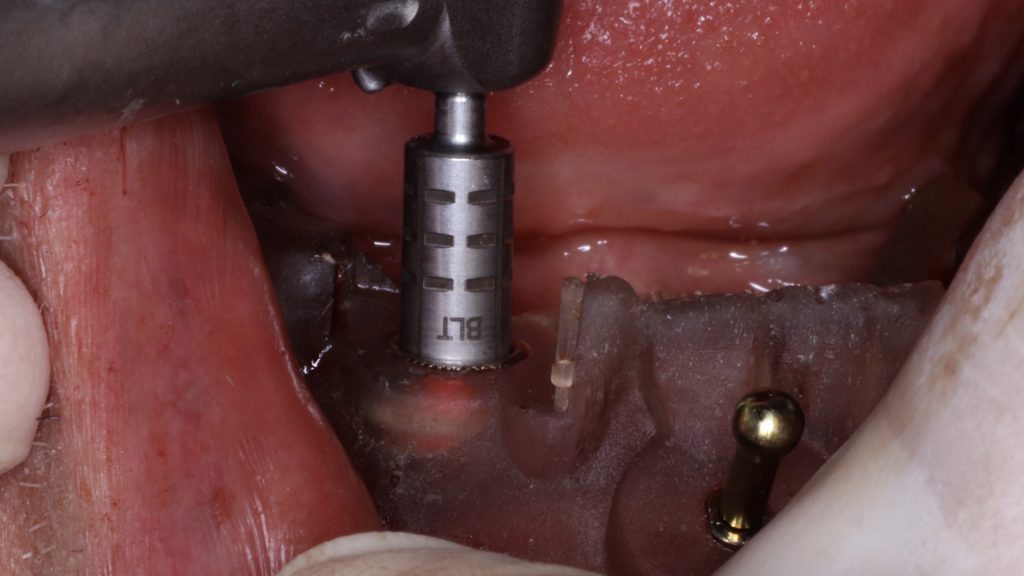
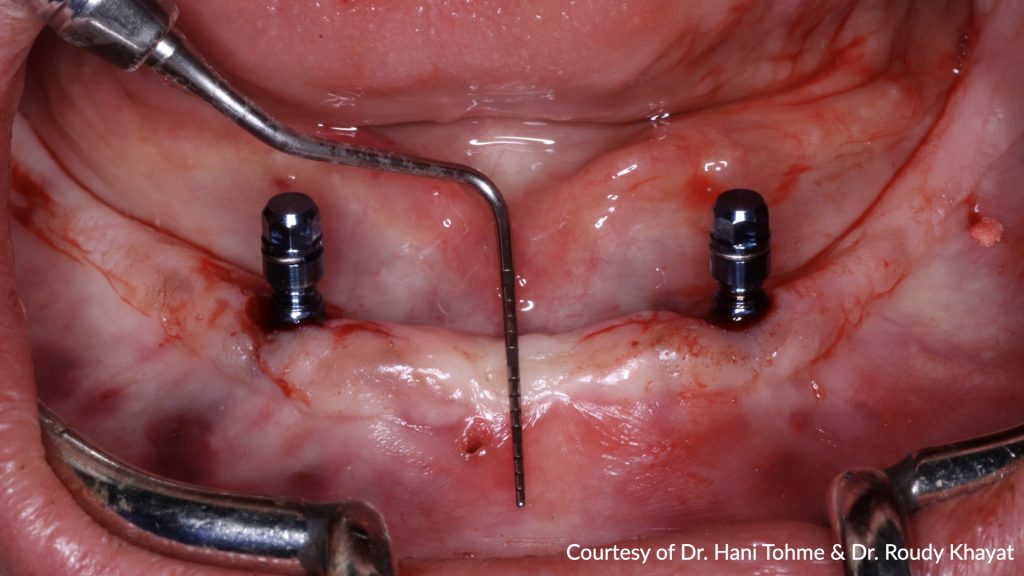
The guided surgery was performed under a flapless approach. This approach is advantageous in being less traumatic surgically when sufficient keratinized tissue exists. Tissues were then punched with the puncher specified in the surgical protocol. The guide was detached to remove the punched tissues prior to the drilling step (Figs 10-11) and then re-secured to proceed with implant bed preparations using the drills specific to guided surgery (Surgical Kit Guided Surgery, Institut Straumann) (Fig. 12). Implants (RC Bone Level Tapered Implant ⌀4.1, length 10 mm, Institut Straumann AG) were then placed into the prepared bed sites as previously planned (Fig. 13). The parallelism and distance between implants attained allow the use of maximum strength of the retentive components and ease the insertion and removal of the overdenture (Fig. 14). Healing abutments were placed (Fig. 15), and post-surgical instructions were given to the patient.
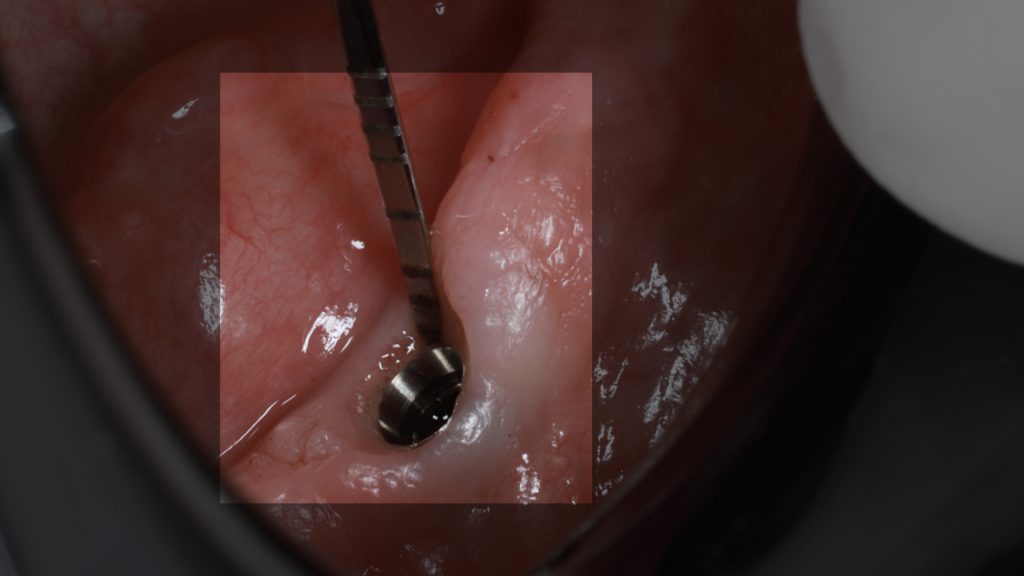
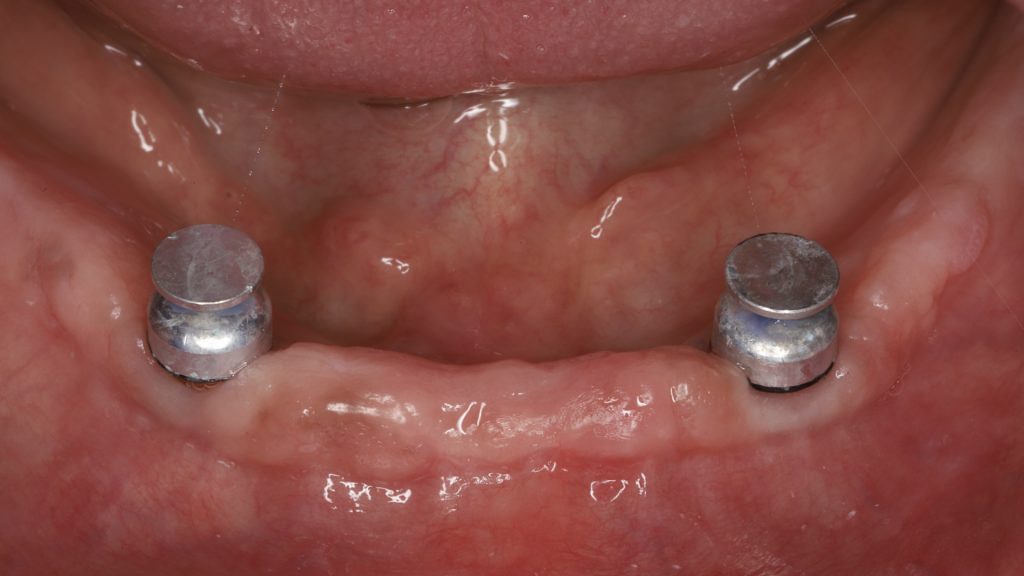
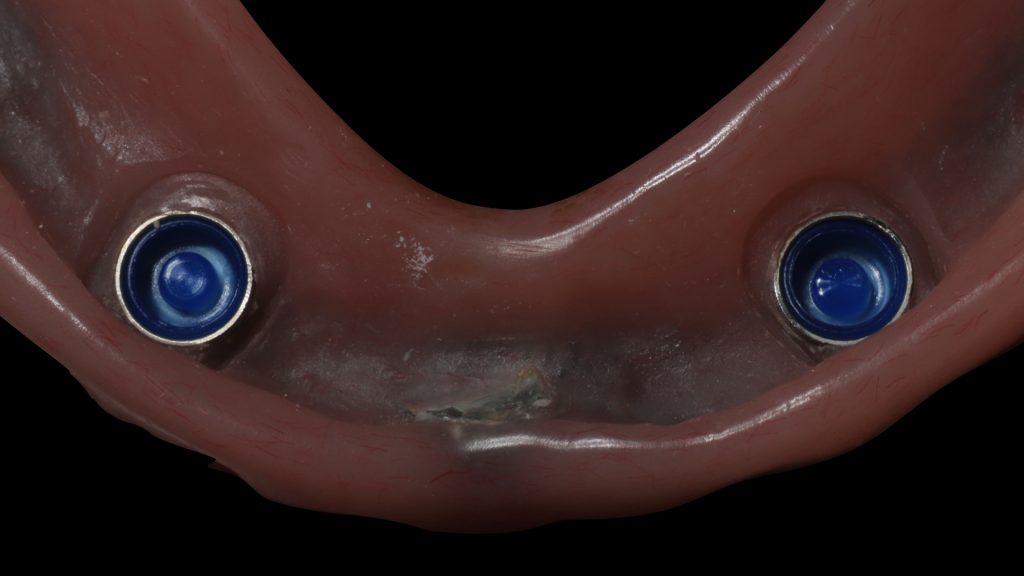
After 3 months of osseointegration, the healing abutments were removed (Fig. 16), and gingival height was measured using a periodontal probe to choose the appropriate locator abutment height (Fig. 17). The placement of implants at equal depths resulted in the relatively equal gingival height of both locators. After selecting the appropriate locator height (LOCATOR® RC AH 2 mm, Institut Straumann), the locator abutment was placed on each implant using the locator hand driver with the locator abutment holder (Fig. 18). Locators were then hand-tightened and a radiograph along the long axis of the implants was taken to ensure the proper seating of the abutments onto the implant fixtures. A locator impression coping was then snapped onto each locator abutment (Fig. 19) and the impression was taken using polyether material anteriorly and zinc oxide eugenol posteriorly (Fig. 20). The lab technician then poured the impression and performed all the steps to fabricate the acrylic overdenture. The black processor was replaced by a blue retention insert (Figs 21-22). The patient was highly satisfied with the stability of the denture during function.
Conclusion
In brief, the long-term survival of mandibular implant-retained overdentures mainly depends on a thorough diagnosis, treatment plan, space analysis, and proper execution of the surgical and prosthetic plan. The practitioner should understand the biomechanical aspects of this treatment modality as well as the relationship between the implant, the surrounding tissues, and the attachment assembly. It is also essential to establish a well-informed interaction between the surgeon and the prosthodontist to help avoid errors in implant placement with the aid of digital technology.
Discover more about this topic:
ITI Consensus Statements on Computer-Guided Implant Surgery
ITI Academy Learning Module: Complete Removable Overdentures: Implant Configuration and Retention