Introduction
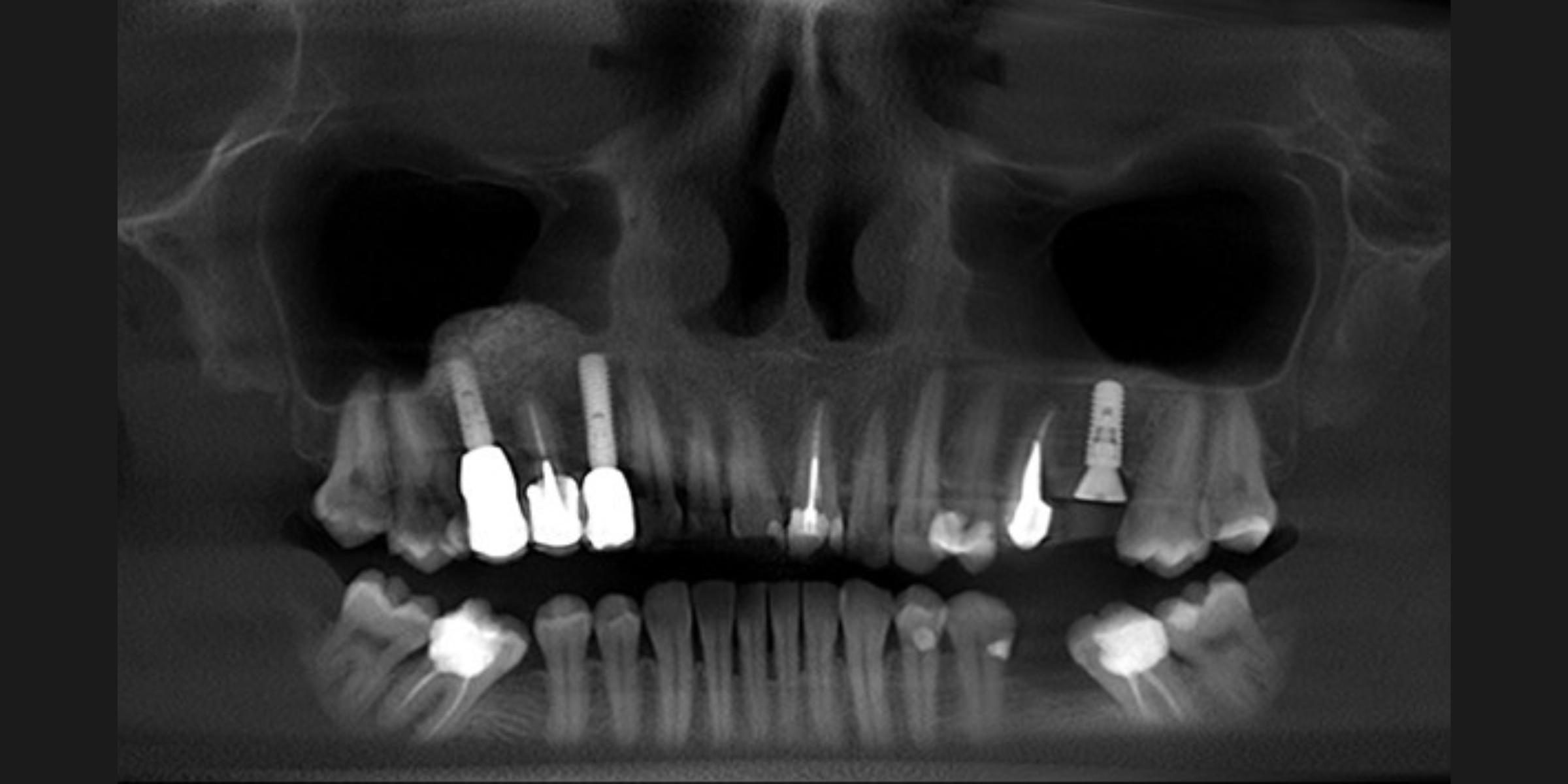
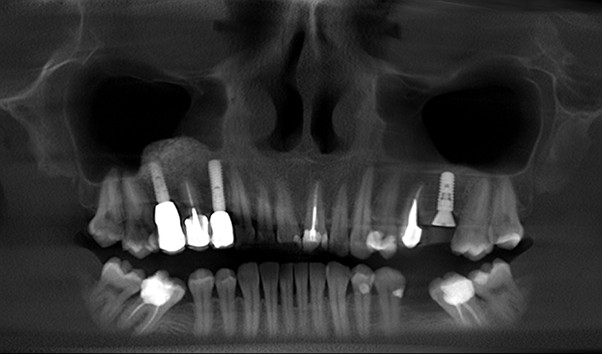
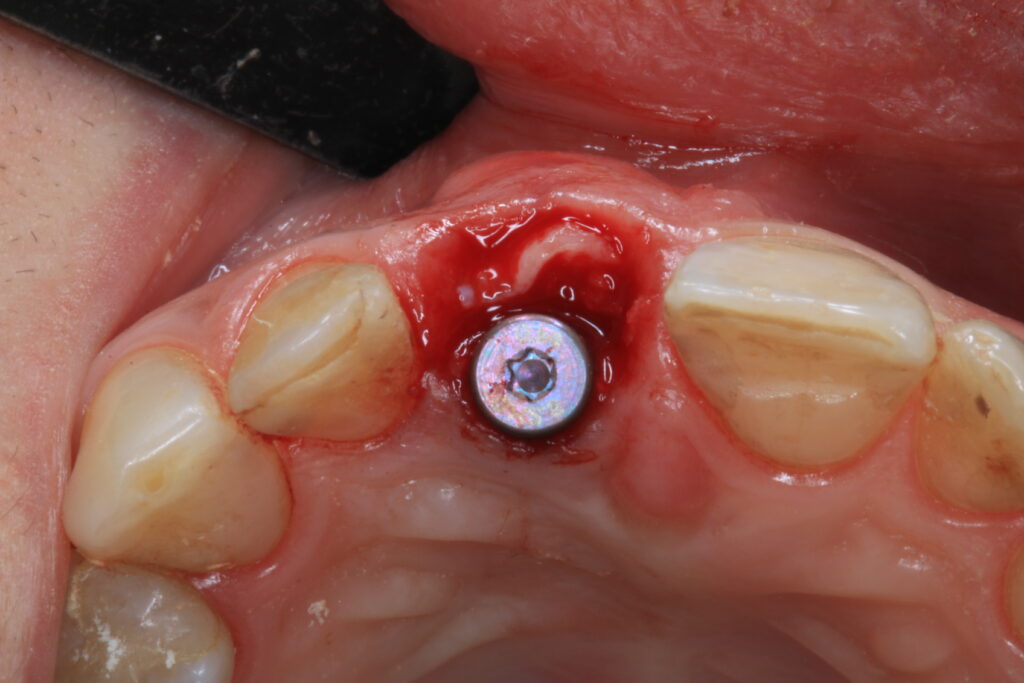
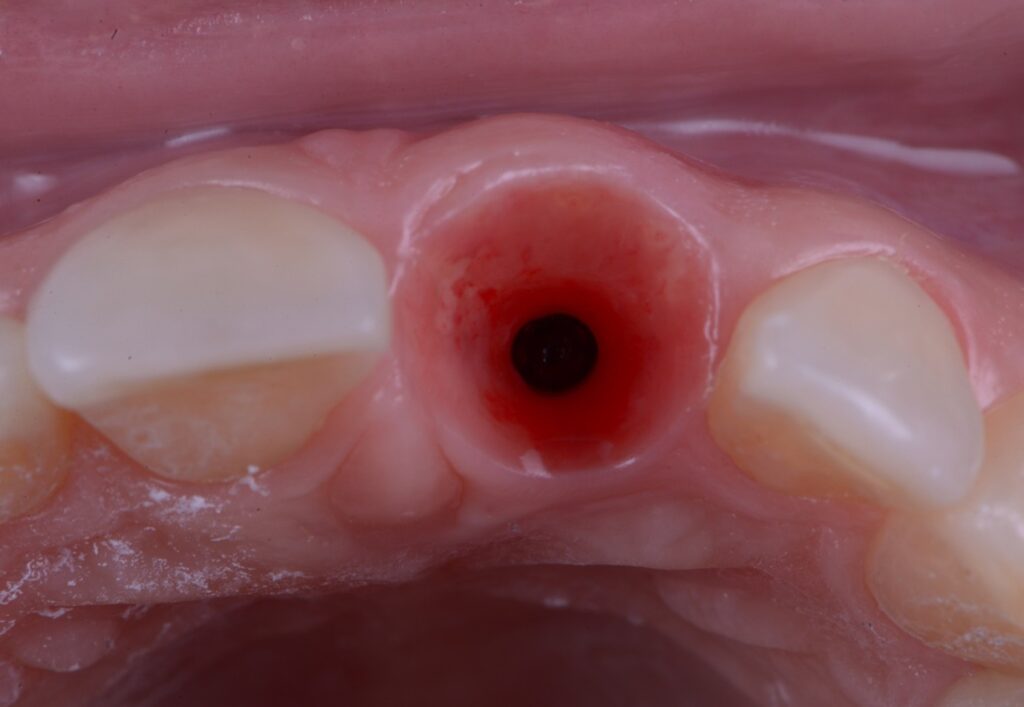
The increasing demand for efficient and minimally invasive tooth replacement options has driven the adoption of immediate implant placement. Within the framework of a patient-centered and comprehensive treatment plan, selecting the appropriate timing for implant placement is a crucial determinant of overall treatment success. Unlike delayed implant placement, which requires several months of healing after extraction, IIP involves placing the implant directly into the fresh extraction socket (Figures 1 and 2). This technique not only reduces the number of surgical interventions and associated patient morbidity but also allows for immediate implant-supported fixed restorations if conditions permit. It significantly reduces both chair time and overall treatment duration compared to other protocols (Puisys et al., 2022). Advances in surgical protocols, digital diagnostics, and implant design have made IIP increasingly predictable, particularly when combined with immediate temporization. However, the clinician must weigh these benefits against the increased technical demands and biological complexities inherent in the procedure. The ITI SAC Classification Tool (Straightforward, Advanced, Complex) helps stratify cases by risk and complexity, thereby guiding appropriate case selection and operator readiness (Morton et al., 2023).


Advantages of immediate implant placement
- Reduced treatment time: Since the implant is placed at the time of tooth extraction, the overall treatment duration is shortened (Puisys et al., 2022).
- Preservation of alveolar bone: Immediate implant placement enables the preservation of the natural contour of the ridge instead of having to reconstruct it (Puisys et al., 2022).
- Improved esthetics: When combined with immediate loading or socket-seal abutments, soft tissue preservation enhances esthetic outcomes, especially in the anterior zone.
- Enhanced patient comfort: Fewer surgical procedures reduce postoperative discomfort and complications. When paired with immediate loading, IIP also eliminates the need for removable provisional prostheses.
Clinical considerations
- Case selection: Ideal conditions are intact alveolar bone, absence of acute infection, healthy adjacent teeth, the ability to achieve correct 3D implant positioning, and anticipated primary stability (Morton et al., 2023).
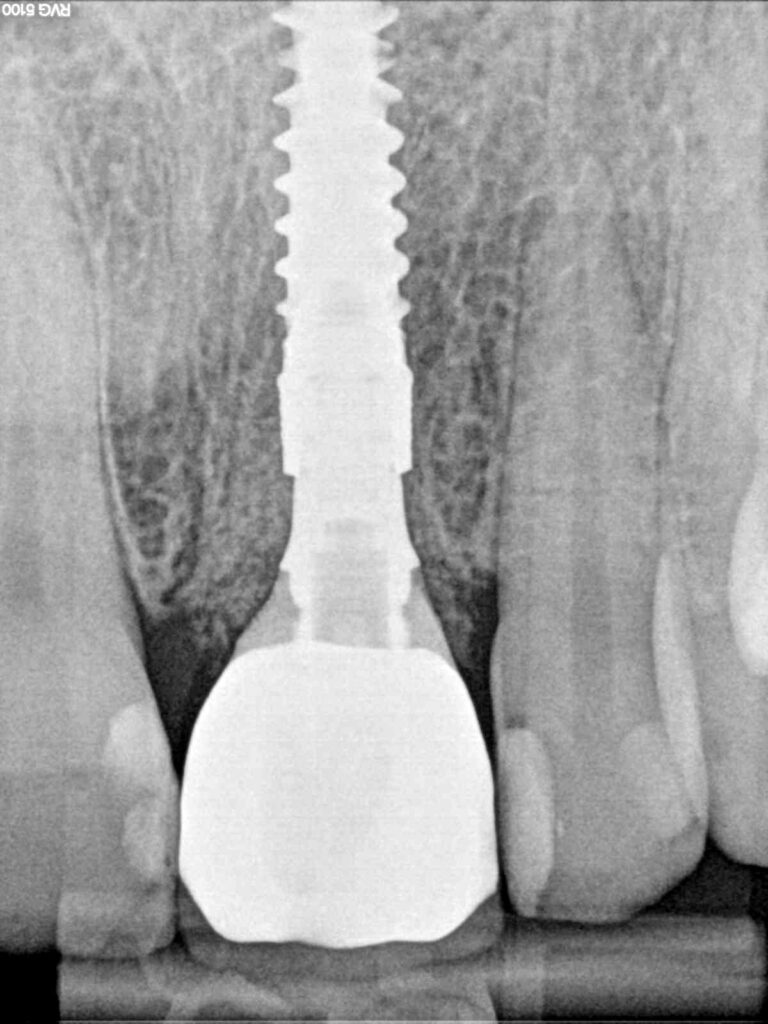
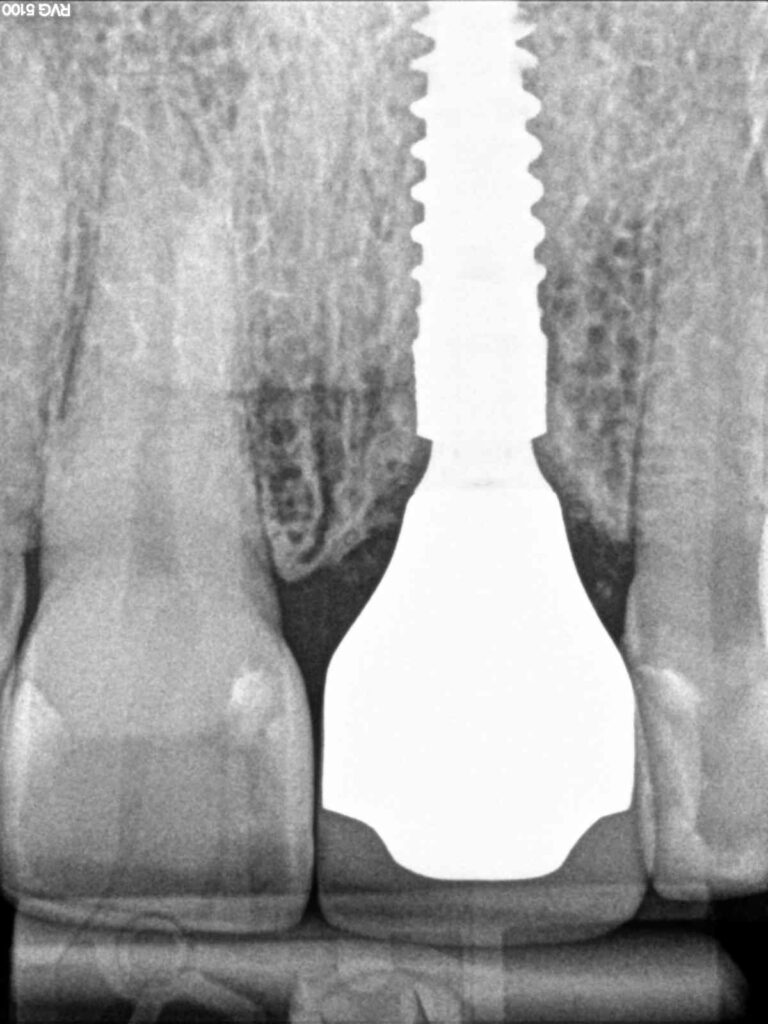
- Primary stability: Achieving primary stability is crucial. This may require implants with aggressive thread designs or extended lengths to engage in the apical bone.
- Gap management: Proper gap dimensions of at least 2 mm between the implant and the facial bone and the use of bone grafting materials (xenograft or allograft) have been shown to increase implant survival and support the stability of the buccal bone dimensions (Morton et al., 2023; Levine et al., 2022; Hamilton et al., 2023). Grafting of the gap was also associated with improved pink esthetic scores (Morton et al., 2023; Wittneben et al., 2023).
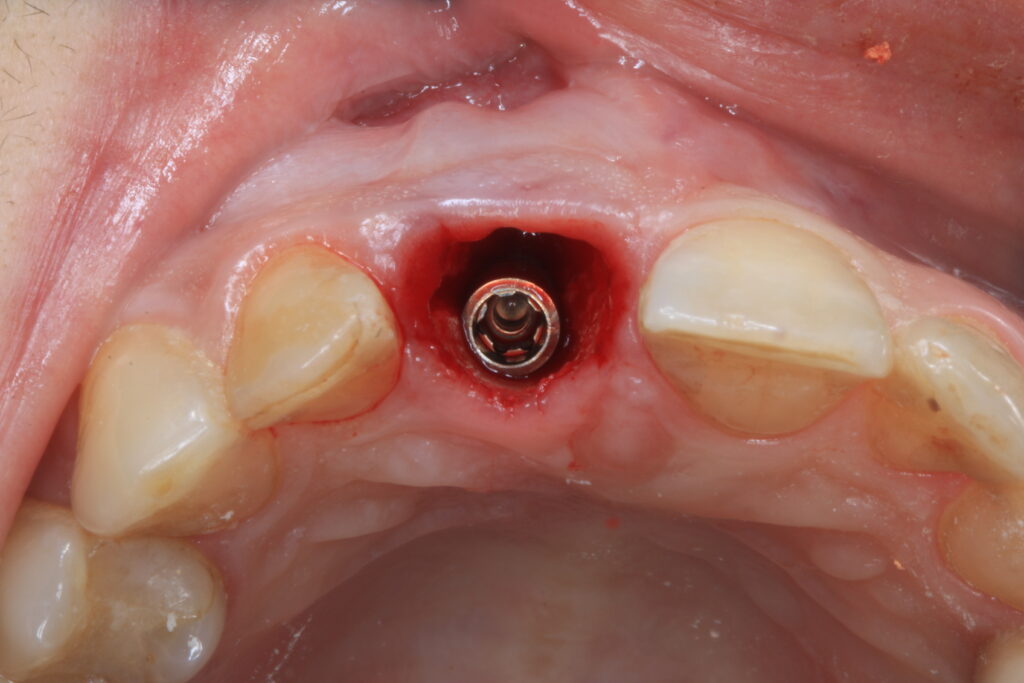
- Soft tissue management: Soft tissue management with a connective tissue graft (CTG) is a key strategy in immediate implant placement, especially in the esthetic zone or cases with a thin biotype. The CTG, typically harvested from the palate, is used to augment soft tissue thickness, enhance mucosal stability, and reduce the risk of midfacial recession and papilla loss. It can be placed using either a flapless tunneling approach or a traditional flapped technique, depending on the clinical scenario (Puisys et al., 2022; Seyssens et al., 2021; van Nimwegen et al., 2018) (Figure 3). A flapless approach is associated with greater buccal bone preservation (Pitman et al., 2023) and good esthetic outcomes (Morton et al., 2023; Wittneben et al., 2023).
- Temporization: In the anterior or premolar region, when primary stability is achieved (insertion torque >35Ncm or implant stability quotient >70), occlusal forces are either absent, minimal, or with shared guidance, and there are no signs of parafunction, immediate loading of the implant with a screw-retained, implant-supported provisional crown can be considered (Lambert et al., 2023). This eliminates the need for a removable provisional, supports soft tissue preservation, and helps prevent apical migration of the soft tissue level (Pitman et al., 2022) (Figures 4, 5). Contraindications for immediate implant placement with immediate loading are mostly related to intraoperative procedural events or a lack of primary stability (Morton et al., 2023; Hamilton et al., 2023).

The provisional restoration can be picked up intraorally after implant placement to ensure proper fit according to the implant position. Alternatively, advances in digital technology enable pre-design and fabrication of the implant-supported provisional crown based on the digitally planned implant position. This crown can be extra-orally cemented to a previously selected titanium base abutment and delivered immediately after implant insertion. However, it is crucial to trial-fit the temporary restoration with the abutment after implant placement and before final cementation to verify proper alignment. While guided surgeries provide higher accuracy than freehand procedures, they are still prone to errors. Any deviation in implant timing, depth, or angulation can prevent proper seating of the provisional crown. Such inaccuracies may arise from errors in the 3D printing of the surgical guide or temporary restoration, inaccuracies in the execution of guided surgery related to operator experience or case difficulty, or drill deflection caused by anatomical variations as the drill tends to go to the least resistant region in immediate cases.
A carefully designed emergence profile is a key element of implant-supported restorations (Gonzalez-Martin et al., 2020) and should already be considered when selecting the correct implant position (Puisys et al., 2023). When designing the emergence profile of an implant-supported restoration in immediate scenarios, attention to the critical and subcritical contours is essential for optimal soft tissue outcomes. The critical contour, located just below the gingival margin, supports the free gingiva and defines the esthetic emergence of the crown. It should be flat to slightly convex to maintain gingival architecture without exerting excessive pressure. The subcritical contour, which extends from the implant platform up to the critical contour, should be concave to create space for soft tissue healing, enhance vascularization, and accommodate connective tissue grafts. Together, these contours guide soft tissue shaping, promote biological integration, and ensure long-term esthetic stability, with digital tools now enabling their precise customization during prosthetic planning (Gonzalez-Martin et al., 2020). This approach significantly shortens intraoperative time by eliminating the need for provisional pick-up, chairside design of emergence profile and finishing. When connective tissue grafts are necessary in immediate implant placement protocols with a thin biotype, the provisional crown should be designed to allow space for the graft, facilitating optimal soft tissue healing and integration. This immediate provisional is replaced with the final implant-supported restoration after the healing period (Figures 6, 7).

Challenges and limitations
- Risk of implant failure: Insufficient primary stability or presence of infection can compromise outcomes. However, the presence of a chronic periapical infection of the tooth being extracted does not present a contraindication for immediate implant placement per se, as long as there is no fistula the infection can be fully debrided and there is still sufficient bone to achieve primary stability of the implant after tooth extraction and proper cleaning of the infected area (Morton et al., 2023; Hamilton et al., 2023).
- Bone resorption: Despite immediate placement, physiological bone remodeling is inevitable. The most pronounced changes occur in sites with a thin facial bone plate, often leading to resorption and soft tissue recession (Araujo et al., 2019) (Ferrus et al., 2010). Use of bone substitutes and tissue grafting can mitigate, but not eliminate, this effect.
- Technique sensitivity: IIP is a complex and technique-sensitive procedure requiring advanced implant and soft tissue surgery, CBCT-based planning, experience with digital tools and guided surgery, and a close integration of surgical and prosthetic disciplines (Dawson et al., 2022).
Conclusion
Immediate implant placement is a powerful technique that can significantly reduce treatment time, preserve bone structure, and improve esthetic outcomes. When paired with immediate loading, it also maintains soft tissue architecture and removes the need for removable provisionals. However, it is classified as a complex treatment requiring expertise in implant and prosthetic treatments (Dawson et al., 2022). Its success hinges on careful case selection, meticulous surgical execution, and strategic prosthetic planning.