Introduction
As clinicians we make daily decisions that affect the long-term outcome of treatment. The choice of implant abutment is important as it can have multiple implications for the health, function, and esthetics of the restoration.
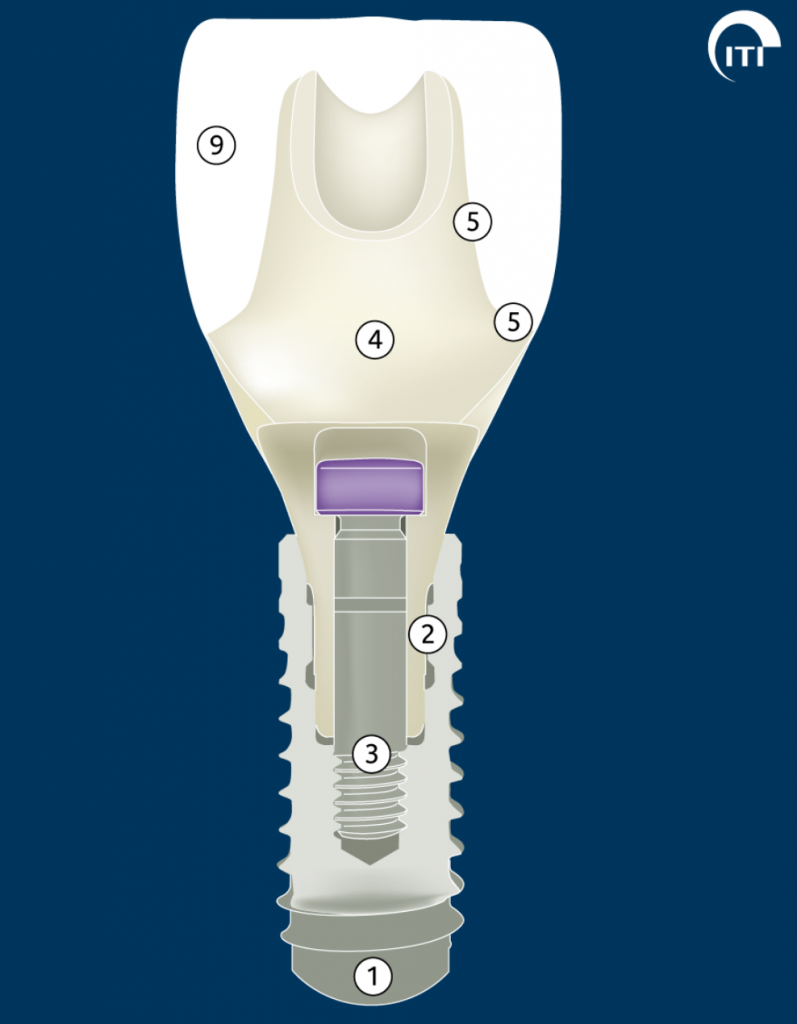
An implant abutment is a component that provides a connection between the implant and the implant restoration (Fig. 1). The ITI Academy Learning Module “Abutment selection for fixed dental prostheses” provides an excellent description of the different types of abutments and their corresponding applications.
These can either be cemented or screw-retained. The considerations and indications for one method of retention or the other with their respective advantages and disadvantages are covered in more detail in the ITI Academy Learning Module “Design Principles for FDPs”.
Clinical and technical considerations
Currently, there are three methods of manufacturing customized abutments: lost wax technique, CAD/CAM, and a two-piece combination of customized and prefabricated parts. The purpose of different abutment designs is to provide flexibility and solutions for any given prosthodontic situation.
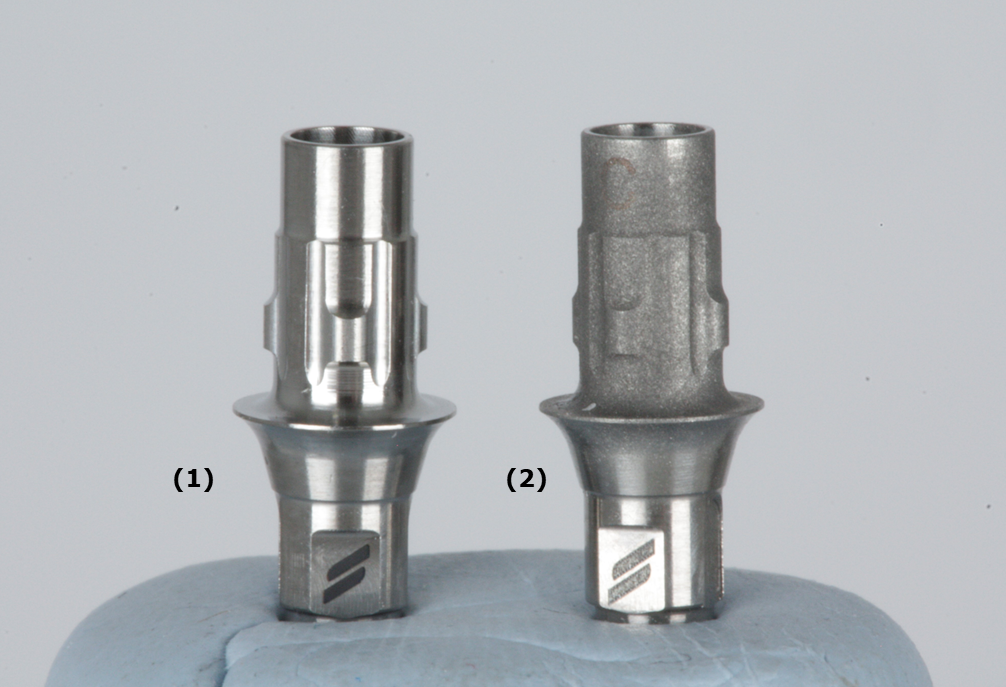
The two-piece design is also known as the hybrid abutment. It consists of a prefabricated titanium base (Ti-base) abutment with retention features that allow for extraoral cementation of the crown. Nowadays, there are two versions of hybrid abutments: the hybrid abutment with a separate crown and the one-piece hybrid-abutment crown.
The hybrid abutment with a separate crown consists of three parts: a customized emergence profile of the restoration cemented extra-orally to a Ti-base and a cemented crown, resulting in two cemented interfaces (Fig. 2).

Hybrid-abutment crowns are a relatively new approach that consists of two components: a one-piece CAD-CAM ceramic crown cemented to a Ti-base abutment to obtain a one-piece screw-retained implant crown restoration (Fig. 3). The advantages of this technique include the customization of the emergence profile and crown in one piece, less clinical and laboratory time, lower laboratory fees, and no risk of residual cement in the peri-implant tissues. These abutments appear promising as they combine a metallic implant connection with a ceramic outer part that can be fabricated in a digital workflow.

This blog article aims to identify the critical clinical and technical factors to consider when selecting the appropriate Ti-base abutment and the restoration material for single implant hybrid-abutment crown restorations to ensure the best possible predictable outcome.
Use an original abutment
The data from the literature indicate that original abutments exhibit lower percentages of torque reduction (Alonso-Pérez et al. 2018). Moreover, original abutments have a perfect internal connection fit allowing for a more homogeneous load distribution between the components which ultimately influences the long-term success of the restorations (Rizvi et al. 2022; Alonso-Pérez et al. 2022; Gigandet et al. 2012).
Peri-implant tissue thickness
Peri-implant tissue thickness should be at least 2 mm to reduce the risk of change in the color appearance of the peri-implant mucosa (Jung et al. 2007; Van Brakel et al. 2011; Lops et al. 2017). If the soft tissue is thinner than 2 mm, it may result in a grayish appearance when a metallic abutment is chosen. Discoloration could also occur when zirconia abutments are used. Moreover, vertical soft tissue thickness influences peri-implant bone stability. The literature suggests having at least 2.5 mm of peri-implant tissue vertically to reduce the risk of losing peri-implant bone (Linkevicius et al. 2018; Blanc et al. 2018)(Fig. 4).
Ti-base abutment selection
Selecting the appropriate abutment is critical to the success of implant treatment. Factors such as implant system, location, and type of restoration should be carefully considered.
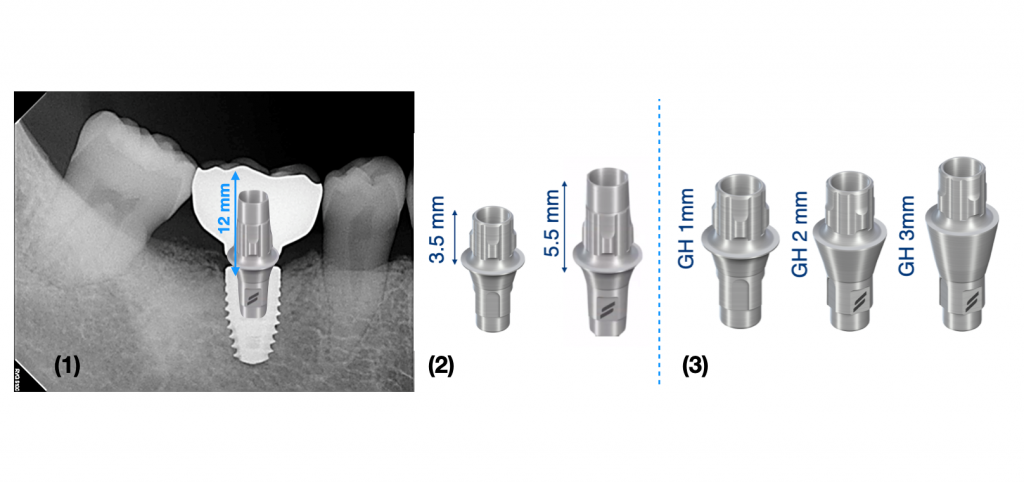
Different Ti-base abutment designs are available for each implant system. It is necessary to know the options offered by the implant system that we plan to restore. When selecting a Straumann Ti-base for single crowns for a bone-level implant with a regular connection it is important to measure the restorative prosthetic space and the vertical peri-implant tissue height. Clinicians must measure the height between the coronal implant platform and the level of the soft tissue, subsequently they can choose from 3 different gingival heights (GH) depending on the depth of the implant (1 mm, 2 mm, 3 mm). Then we can measure the vertical distance between the abutment base and the required occlusal height of the restoration to select the abutment height (3.5 mm or 5.5 mm) (Fig. 5).
We must keep in mind that the selection of a short Ti-base (3.5 mm) for an increased crown-abutment ratio increases the lever arm and the possibility of de-cementation of the crown (Sailer et al. 2018; Pitta et al. 2021; Pjetursson et al. 2022). In a clinical scenario where there is limited space for the taller abutment it is recommended to initially use the tallest abutment and adjust its height as necessary to reduce this risk.
Moreover, cylindrical titanium bases must be preferred to conical ones for single-crowns and implant FDPs to provide a lower percentage of debonding (Calderon et al. 2022).
Definitive restorative material selection
Different biomaterials are available for single-unit implant restorations. The choice of the material depends on various factors like the esthetic demands of the patient, location, patient occlusion, prosthetic space available, opposite dentition, and the different physical, mechanical, and optical properties of the ceramic material.
Although 3Y-TZP zirconia has the best mechanical properties in terms of strength and toughness, it is an opaque framework material and should be veneered with feldspathic porcelain for a better esthetic result (Alammar et al. 2022; Schley et al. 2010; Agustin-Panadero et al. 2014; Zhang & Lawn 2018). However, the contact between the dental porcelain and the peri-implant tissue is much less biocompatible (Linkevicius et al. 2017).
New generations of zirconia were developed by increasing the yttria content from 3 mol% to 4 mol%, and 5 mol%. While this markedly improved translucency, drawbacks are the decrease in strength and toughness (Zhang & Lawn 2018; Ban 2021). Multi-layered zirconia blocks give the technician the possibility to construct monolithic restorations with different translucencies and mechanical properties. These blocks allow the two zirconium-oxide raw materials 3Y-TZP and 5Y-TZP to be combined for their mechanical and optical properties to make implant supra-structures.
When choosing more translucent zirconia, the suitable indication would be for full-contoured monolithic restorations in the anterior and posterior area (Pjetursson et al. 2022; Alammar et al. 2022; Güth et al. 2019). Another material option is lithium disilicate. This can be pressed or milled and used to make monolithic single implant crowns in anterior and posterior areas with good physical and esthetic results (Pitta et al. 2021; Sailer et al. 2015; Joda et al. 2017).
When esthetics are a challenge, lithium disilicate, and zirconia can be micro-veneered (0.8 mm to 1 mm) excluding incisal edges and cusp tips to decrease the risk of chipping (Saponaro et al. 2023). Zirconia shows a high level of biocompatibility, with less plaque formation and reduced inflammatory reaction, which allows stabilization of the surrounding soft tissues in polished zirconia (Nothdurft et al. 2015; Degidi et al. 2006). In-vitro studies report that gingival fibroblasts have adhesion to polished lithium disilicate, showing good biocompatibility (Moretti et al 2022). Therefore, the emergence profile of the restoration that is in contact with the peri-implant tissue should be polished and not glazed.
Antagonist enamel wear is also a concern. Zirconia and lithium disilicate should be polished after adjustment to reduce the rough surface to decrease the risk of ceramic fracture and wear on opposing teeth/material (Güth et al. 2019; Moretti et al 2022; Janyavula et al. 2013).
Cement selection
Currently, there is no universal cement that can be used with all types of ceramics when cementing to Ti-bases. It has been documented that cement shade influences the shade outcomes of lithium disilicate crowns (Lops et al. 2017) resulting in a gray restoration. One notable resin cement, Multilink HO 0, is able to mask the gray color of the Ti-base (Liu et al. 2020).
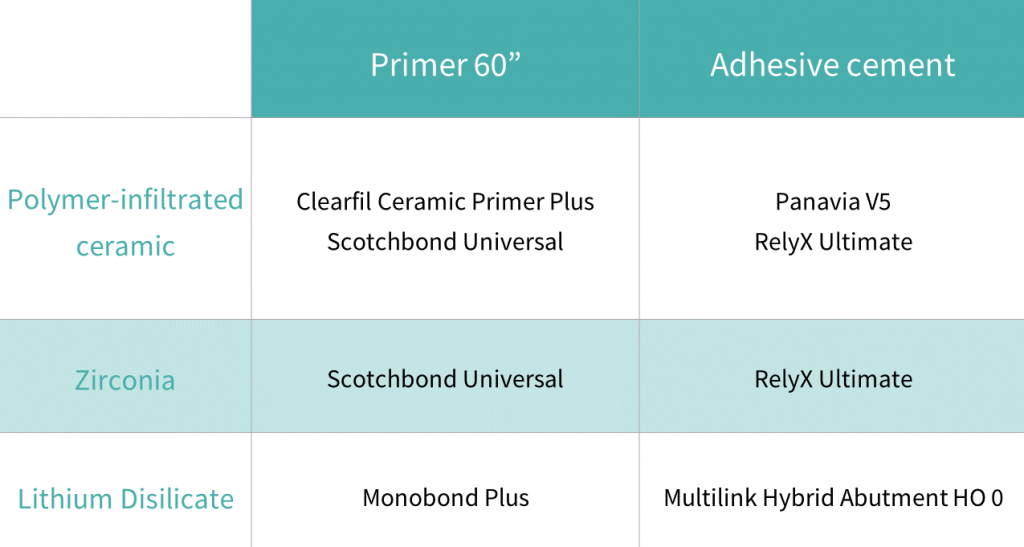
A specific bonding protocol is recommended for each restorative material (Burkhardt et al. 2022). The protocol is as follows:
- Sandblast the titanium base with 50μm Al2O3 at 2.5 bar air pressure with 45-degree angle of incidence for 10 seconds.
- Clean and etch ( HF 5% 20s) the intaglio surface of the lithium disilicate crowns and sandblast the intaglio of zirconia-based crowns (50 μm Al2O3 at 2.5 bar for 10 seconds).
- Clean and dry de titanium-base and the the ceramic with 70% ethanol alcohol in an ultrasonic bath for 4 minutes and dry with oil-free air.
- Finally apply the specific primer and cement according to this table (Burkhardt et al. 2022). (Fig. 6).
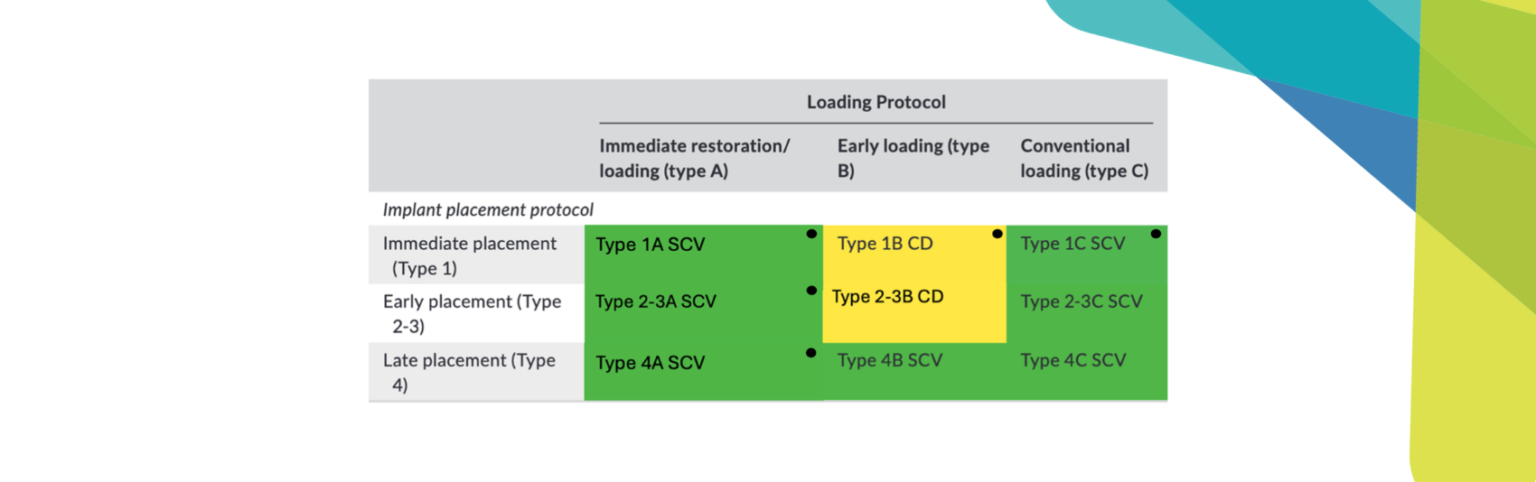
Clinical Case Discussion – Type 1C (immediate placement + conventional loading)
A healthy 65-year-old female patient came to our clinic with a non-restorable tooth #15 (Fig. 7). A minimally traumatic extraction using a fine periotome was done, a BLT 3.3 x 10 mm Straumann implant was immediately placed, and a healing cap was screwed on. The socket gap was filled with a xenograft (BIO-Oss, Geistlich), covered with a resorbable collagen wound dressing (Novatape, Novabone products), and was stabilized with a horizontal mattress suture to close the socket space around the healing cap.
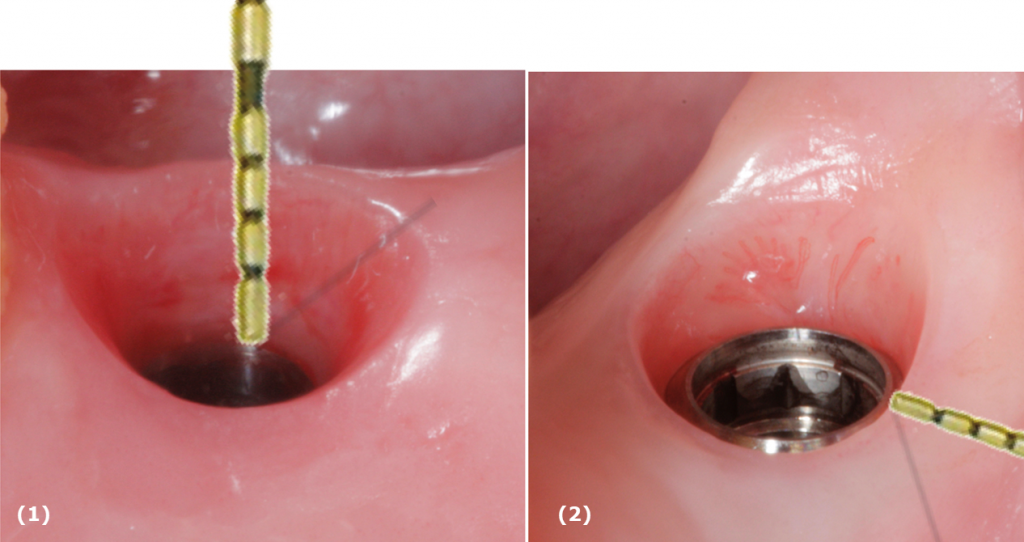
Three months later, a conventional impression was made using an individualized light cure open impression tray and a VPS as impression material. In the same appointment, the peri-implant tissue height was measured with a millimeter periodontal probe to select the correct gingival height of the Ti-base.
To select the appropriate abutment height of the titanium-base, the space between the platform of the implant and the antagonist occlusal surface was measured. In this case, the distance measured was 12 mm, resulting in the selection of a Ti-base height of 5.5 mm with a gingival height of 2 mm. A monolithic zirconia crown was chosen as the restorative material.
Prior to try-in, the crown was temporarily cemented to the Ti-base using Temp-bond. To ensure that the restoration was in place, the patient was asked to bite on a cotton roll for 3 to 5 minutes. Once the occlusion, contact points, shape, and color of the restoration had been evaluated, the restoration was disinfected and then placed in the ultrasonic tank with 70% ethanol alcohol for 4 minutes to ensure easy de-cementation. The definitive cementation was conducted following this protocol:
- Protect the connection and the gingival height of the Ti-base with a Teflon tape
- Sandblast the bonding surface of the Ti-base with 50 μm Al2O3 at 2.5 bar for 10 seconds, the result will be a matte-colored surface. (Fig. 8)
- Place the Ti-base in a 70% ethanol ultrasonic-assisted bath for 4 minutes and dry with oil-free air.
- Sandblast the internal surface of the bonding surface of the zirconia crown with 50 μm Al2O3 at 2.5 bar at a 10 mm distance at 45º for 10 seconds and place the crown in the ultrasound bath with 70% ethanol alcohol for 4 minutes and dry with oil-free air.
- Apply primer (Scotchbond Universal) with a micro brush to the Ti-base surface and the bonding surface of the zirconia crown for 60 seconds.
- Block the screw access with autoclaved Teflon tape to avoid getting cement inside the channel.
- Apply one layer of resin cement (RelyX Ultimate) to the Ti-base surface in the shoulder of the restoration to avoid gaps in this area, then carefully put the crown in place on the Ti-base wait for a couple of seconds and gently remove the cement excess with a micro brush.
- Wait for 6 minutes as indicated by the manufacturer for the complete polymerization of the cement.
- Polish with an appropriate silicon polisher for zirconia.
- Remove the Teflon tape from the screw access hole, clean the restoration with the steam machine, or, if you don’t have a steam machine, it can be cleaned in an ultrasound bath with alcohol for 4 minutes. Now the hybrid-abutment crown is ready to be delivered (Fig. 9).


The hybrid abutment crown was securely tightened at 35 Ncm, following the manufacturer’s guidelines. To ensure the protection of the screw, the screw access hole was then carefully sealed using autoclaved Teflon tape. This process left a 2 mm space to allow for the insertion of filling material. A layered composite was applied to fill the access hole. Afterwards, the occlusion was thoroughly checked, and the restoration was polished. In addition to the treatment, the patient was provided with comprehensive oral hygiene instructions to maintain the longevity and health of the restoration. The patient was very pleased with the efficient implant placement and the esthetics of the hybrid abutment-crown (Fig 10-11).


In my opinion, the hybrid abutment-crown restoration represents an ideal blend of mechanical
stability provided by a metallic implant connection and the functional and aesthetic benefits offered
by a ceramic restoration. This approach results in a one-piece screw-retained restoration that
achieves both durability and pleasing esthetics.
Summary
- Use an original component to reduce mechanical failures.
- Peri-implant tissue thickness should be at least 2 mm to reduce the risk of change in color appearance.
- Select the higher Ti-base abutment when possible.
- Limit micro-veneering materials to the buccal surface.
- Stained and glazed monolithic lithium-disilicate/zirconia are the ceramic options for single-unit anterior or posterior regions.
- The part of the emergence profile of the restoration that is in contact with the peri-implant tissue should be polished only and not glazed.
- Select a cylindrical and taller Ti-base abutment to reduce debonding risk.
- Sandblast the Ti-base with 50 µm aluminum oxide at 2.5 bar at 45º 10 seconds to improve bonding.
- Etch the lithium-disilicate according to the manufacturer’s instructions.
- Clean the restoration with ethanol alcohol at 70% in an ultrasonic bath for 4 minutes and dry with oil-free air.
- Cement lithium-disilicate restorations with Multilink Hybrid Abutment HO 0 and use Monobond Plus as a primer.
- Cement polymer-infiltrated ceramics network using Panavia V5 with Clearfil Ceramic Primer or RelyX Ultimate with Scotchbond Universal as a primer
- Cement zirconia restorations with RelyX Ultimate and use Scotchbond Universal as a primer.