Introduction
Hard- and soft-tissue deficiencies resulting from tooth extraction, trauma, and a history of severe periodontitis or peri-implantitis are common issues that can hinder the optimal placement of dental implants in prosthetically guided positions (Chiapasco et al. 2018, Hammerle et al. 2018).
When the available residual bone does not permit implant placement according to an optimal restorative plan, prosthetically guided bone augmentation should be performed either before or during implant placement to restore an optimal bone architecture for implant insertion (Chiapasco-Casentini 2018, Monje et al. 2023).
Nonetheless, it is still very common to observe situations with severely atrophic bone where prosthetically guided bone augmentation has been avoided. As a result, implants are often misplaced according to residual bone availability rather than ideal restorative positioning, leading to a wide variety of vertical and horizontal peri-implant bone defects and peri-implant soft-tissue deficiencies (Berglundh et al. 2018).
These conditions typically lead to low patient-satisfaction, as the prosthetic restoration connected to the improperly placed implant results in compromised functional and esthetic outcomes and restricts their ability to carry out self-performed plaque control measures (Zucchelli et al. 2020, Sanz Martin et al. 2021, Tavelli et al. 2022).
According to the severity of the implant malposition and its impact on the possibility to deliver implant-supported restorations with esthetically adequate and cleansable emergence profiles, treatment of such conditions may consist in: a) pure mucogingival interventions designed to coronally reposition the implant soft-tissue margin, increase its thickness and/or the keratinized tissue width (Anderson et al. 2013, Fickl 2015) ; b) multidisciplinary prosthetic and surgical approaches, where implant-supported supra-structures are either modified or removed to create optimal local conditions for the delivery of a mucogingival surgical intervention (Zucchelli et al. 2013, 2019); c) the complete removal of the malpositioned implant with the subsequent delivery of a bone augmentation procedure and a novel implant-supported rehabilitation (Urban et al. 2021).
Sole mucogingival interventions
Although observational data have shown that implant malpositioning on the bucco-palatal axis is likely among the most influential factors in the development of peri-implant tissue deficiencies (Sanz Martin et al. 2021), such conditions can also occur around properly positioned implants, where suboptimal hard- or soft-tissue management at the time of implant placement may result in a lack of keratinized tissue width or thickness, or a soft tissue margin located apically to its ideal position (Zucchelli et al. 2019).
In such scenarios where implants have been placed in alignment with the planned prosthetic restoration to ensure emergence of the prosthetic screw located at the central fossa of premolars and molars and 1 mm palatal to the incised edge of incisor teeth (Pedrinaci et al. 2024), treatment can rely solely on mucogingival procedures since the implant position itself does not necessitate corrective interventions. These procedures aim to restore the optimal position of the soft tissue margin, with adequate thickness and keratinized tissue width. This can be achieved through techniques such as free gingival grafts, which aim to restore optimal keratinized tissue width (Fickl 2015, Thoma et al. 2018), or bilaminar techniques using connective tissue grafts to move the peri-implant soft-tissue margin coronally and increase its thickness, thereby providing optimal esthetic camouflage of the underlying implant-supported prosthetic components (Anderson et al. 2013, Burkhardt et al. 2008, Tavelli et al. 2023).
The technical steps of these procedures replicate those of classical mucogingival interventions around natural teeth, with the added complexity of decontaminating the implant surface exposed to the oral cavity from the accumulation of oral biofilm, if present (Figures 1-3) (Cha et al. 2019, Baima et al. 2022).
 Fig. 1: Peri-implant soft tissue deficiency at an implant in a prosthetically driven position with an implant-supported crown inside the buccal contour of the adjacent natural teeth (Class IIb, Zucchelli et al. 2019)
Fig. 1: Peri-implant soft tissue deficiency at an implant in a prosthetically driven position with an implant-supported crown inside the buccal contour of the adjacent natural teeth (Class IIb, Zucchelli et al. 2019)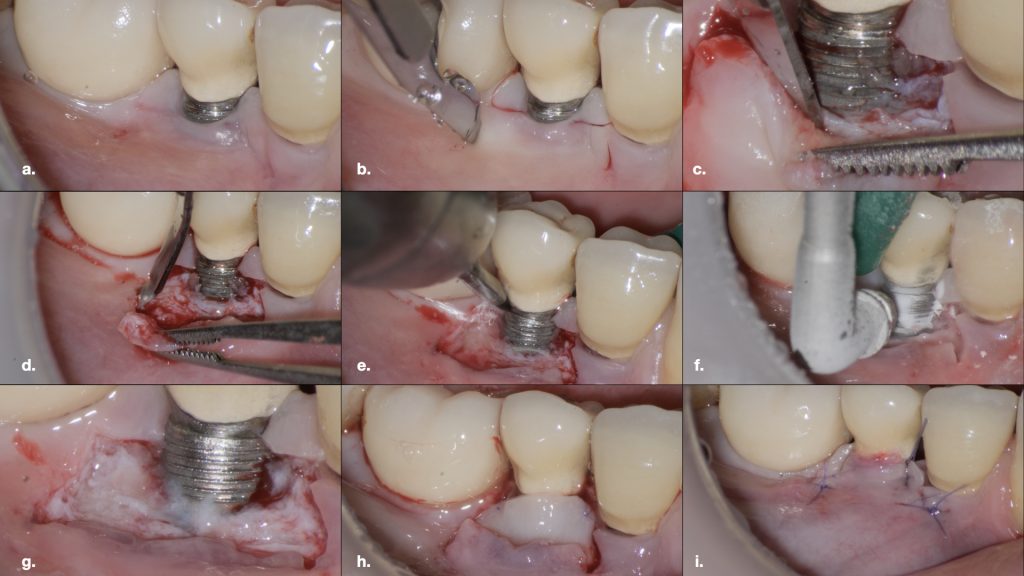 Fig. 2: Treatment of the peri-implant deficiency with a coronally advanced flap with the adjunct use of a connective tissue graft
Fig. 2: Treatment of the peri-implant deficiency with a coronally advanced flap with the adjunct use of a connective tissue graft Fig. 2 a: Trapezoidal flap design
Fig. 2 a: Trapezoidal flap design Fig. 2 b: Technical detail of the first incision line
Fig. 2 b: Technical detail of the first incision line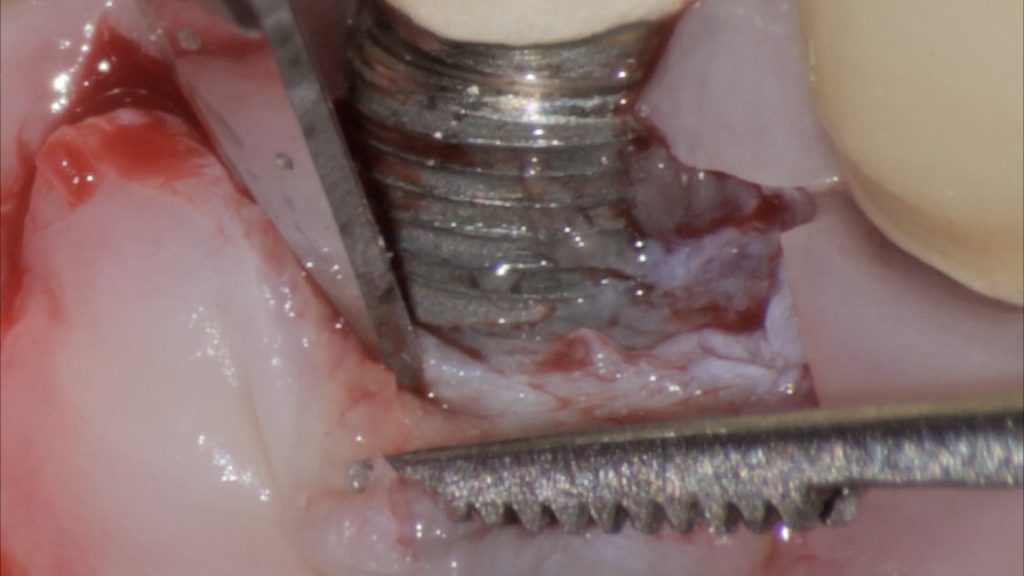 Fig. 2 c: Sharp dissection of the flap from the dehiscent implant surface
Fig. 2 c: Sharp dissection of the flap from the dehiscent implant surface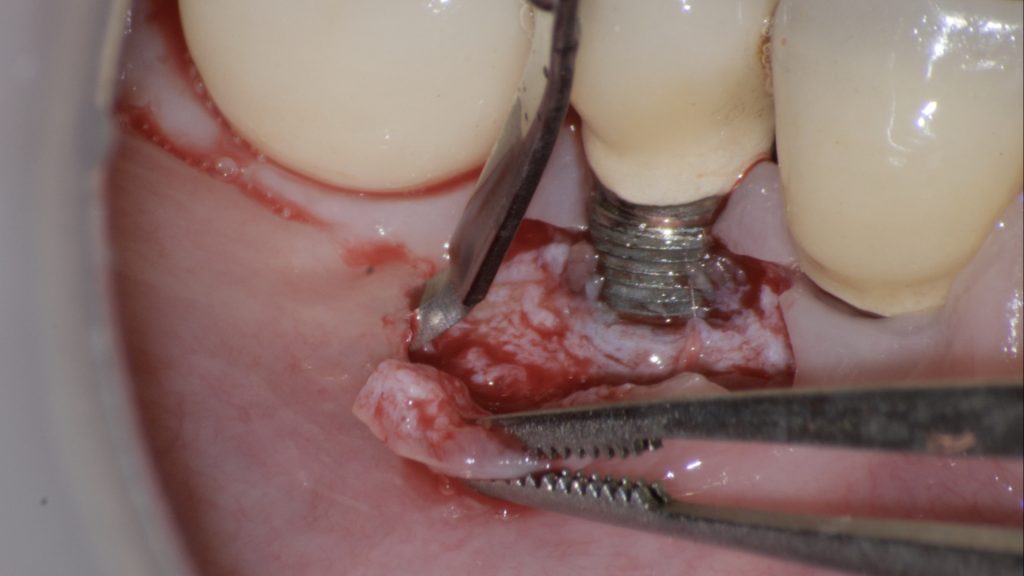 Fig. 2 d: Split thickness dissection of the flap to achieve adequate passivation and isolation of the alveolar mucosa from its muscular plane; d) Decontamination of the exposed implant surface with a titanium brush
Fig. 2 d: Split thickness dissection of the flap to achieve adequate passivation and isolation of the alveolar mucosa from its muscular plane; d) Decontamination of the exposed implant surface with a titanium brush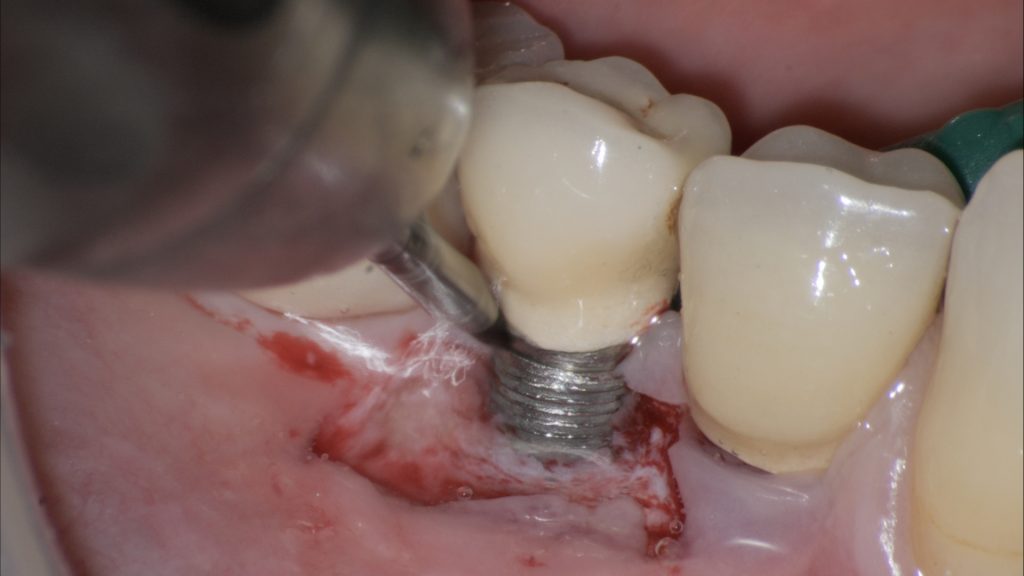 Fig. 2 e: Decontamination of the exposed implant surface with a titanium brush
Fig. 2 e: Decontamination of the exposed implant surface with a titanium brush Fig. 2 f: Decontamination of the exposed implant with erythritol-based air abrasive powders
Fig. 2 f: Decontamination of the exposed implant with erythritol-based air abrasive powders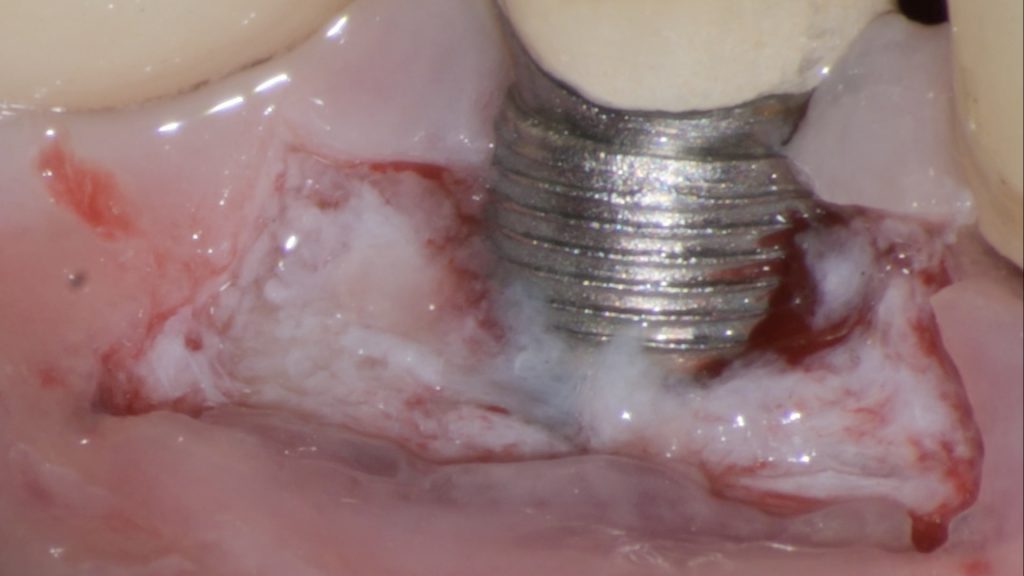 Fig. 2 g: Assessment of the decontaminated implant surface at high magnification with the help of a surgical microscope
Fig. 2 g: Assessment of the decontaminated implant surface at high magnification with the help of a surgical microscope Fig. 2 h: Stabilization of a connective tissue graft at the base of the de-epithelialized papillae
Fig. 2 h: Stabilization of a connective tissue graft at the base of the de-epithelialized papillae Fig. 2 i: Final flap position after suturing
Fig. 2 i: Final flap position after suturing Fig. 3: One-year follow-up after the surgical intervention. Satisfactory phenotype modification and coronal advancement of the peri-implant soft tissue margin have been achieved
Fig. 3: One-year follow-up after the surgical intervention. Satisfactory phenotype modification and coronal advancement of the peri-implant soft tissue margin have been achieved
Combined prosthetic-mucogingival interventions
When dealing with peri-implant tissue deficiencies associated with implants malpositioned on the bucco-palatal or mesio-distal aspect, a preliminary prosthetic correction of the implant malposition should be performed, if feasible, before any mucogingival intervention. This correction aims to restore a prosthetic emergence profile that facilitates the surgical procedure and is compatible with maintaining stable and cleansable peri-implant tissues (Zucchelli et al. 2013, 2019).
Depending on the severity of the implant malposition, the prosthetic correction may vary. In less severe cases, where the implant body is located within the buccal contour of the natural mesial and distal roots (Class III peri-implant deficiencies – Zucchelli et al. 2019), the correction can be limited to a direct modification of the crown’s emergence profile. In more severe cases, where the implant is positioned outside the buccal contour of the natural mesial and distal roots (Class IV peri-implant deficiencies – Zucchelli et al. 2019), a novel implant-supported restoration may be required to correct the malposition, using a customized, angled abutment. (Figures 4-6)
 Fig. 4: Combined prosthetic-surgical approach for the treatment of an isolated Class IIIa peri-implant tissue deficiency (Zucchelli et al. 2019): a) Baseline view showing the presence of a provisional implant-supported crown with over-contoured emergence profile
Fig. 4: Combined prosthetic-surgical approach for the treatment of an isolated Class IIIa peri-implant tissue deficiency (Zucchelli et al. 2019): a) Baseline view showing the presence of a provisional implant-supported crown with over-contoured emergence profile Fig. 4 b: of a provisional implant-supported crown with over-contoured emergence profile; b) Placement of a customized angled and narrow abutment which corrects the implant malposition
Fig. 4 b: of a provisional implant-supported crown with over-contoured emergence profile; b) Placement of a customized angled and narrow abutment which corrects the implant malposition Fig. 4 c: Cementation of an intentionally short provisional crown, which leaves abundant mesio-distal space for interproximal soft-tissue maturation
Fig. 4 c: Cementation of an intentionally short provisional crown, which leaves abundant mesio-distal space for interproximal soft-tissue maturation Fig. 4 d: Soft-tissue maturation one month later
Fig. 4 d: Soft-tissue maturation one month later Fig. 5: Surgical procedure following preoperative prosthetic tissue conditioning using a coronally advanced flap with the adjunct use of a connective tissue graft: a) Trapezoidal flap elevation
Fig. 5: Surgical procedure following preoperative prosthetic tissue conditioning using a coronally advanced flap with the adjunct use of a connective tissue graft: a) Trapezoidal flap elevation Fig. 5 b: De-epithelialization of the anatomical papillae
Fig. 5 b: De-epithelialization of the anatomical papillae Fig. 5 c: Stabilization of the connective tissue graft at the base of the anatomic papillae
Fig. 5 c: Stabilization of the connective tissue graft at the base of the anatomic papillae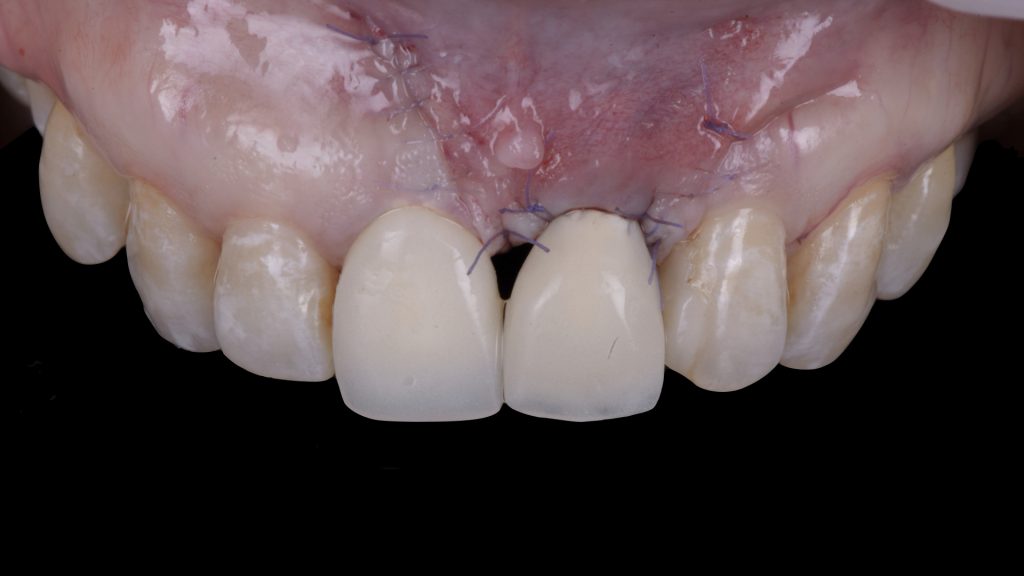 Fig. 5 d: Flap suturing
Fig. 5 d: Flap suturing Fig. 6: Eighteen-month follow-up after the surgical intervention. Satisfactory phenotype modification and coronal advancement of the peri-implant soft tissue margin have been achieved
Fig. 6: Eighteen-month follow-up after the surgical intervention. Satisfactory phenotype modification and coronal advancement of the peri-implant soft tissue margin have been achieved
The use of customized abutments can also represent a highly effective strategy to improve the peri-implant papillae before the mucogingival intervention, further facilitating the surgical procedure. Indeed, placing extremely narrow, customized abutments combined with intentionally short, cemented provisional crowns that leave part of the abutment surface exposed to the oral cavity creates an optimal environment for interproximal soft-tissue creeping and maturation in the weeks preceding the mucogingival surgery (Zucchelli et al. 2013, Mazzotti et al. 2018).
Once optimal soft tissue maturation is achieved, a simplified mucogingival intervention can be performed directly on the customized abutment, replicating once again the technical steps of mucogingival interventions around natural teeth, combined with the intraoperative decontamination of the exposed implant surface (Cha et al. 2019, Baima et al. 2022).
Implant submergence
When managing severe peri-implant deficiencies associated with the complete loss of the peri-implant papillae, a vertical soft tissue augmentation procedure is indicated.
As the reconstruction of missing interproximal tissues is challenging and often unpredictable (Tarnow et al. 1992, Chow et al. 2010), this procedure can greatly benefit from the temporary or permanent removal of the implant suprastructure, placement of an implant closure cap, and submergence of the implant platform (Lai et al. 2010, Chu & Tarnow 2013). A vertical soft tissue augmentation is then performed over the submerged implant, using multiple connective tissue grafts, to restore optimal vertical soft-tissue height at the edentulous site (Figures 7-9) (Stefanini et al. 2020, Tavelli et al. 2021).
 Fig. 7: Severe peri-implant soft-tissue deficiency with absence of interproximal peri-implant soft tissues (Class IIIc – Zucchelli et al. 2019) combined with a RT3 A- gingival recession on the adjacent natural lateral incisor
Fig. 7: Severe peri-implant soft-tissue deficiency with absence of interproximal peri-implant soft tissues (Class IIIc – Zucchelli et al. 2019) combined with a RT3 A- gingival recession on the adjacent natural lateral incisor Fig. 8: Combined prosthetic and surgical treatment sequence for implant submergence and vertical soft-tissue augmentation; a) Placement of a submerged implant cap and prosthetic preparation of the adjacent natural tooth for the delivery of a tooth-supported bridge
Fig. 8: Combined prosthetic and surgical treatment sequence for implant submergence and vertical soft-tissue augmentation; a) Placement of a submerged implant cap and prosthetic preparation of the adjacent natural tooth for the delivery of a tooth-supported bridge Fig. 8 b: Soft tissue phenotype modification achieved after repeated vertical soft-tissue augmentation and prosthetic conditioning using an ovate pontic
Fig. 8 b: Soft tissue phenotype modification achieved after repeated vertical soft-tissue augmentation and prosthetic conditioning using an ovate pontic Fig. 8 c: Baseline occlusal view after removal of the implant-supported crown
Fig. 8 c: Baseline occlusal view after removal of the implant-supported crown Fig. 8 d: Occlusal view after repeated vertical soft tissue augmentation and prosthetic conditioning (Prosthetics: Dr. Tommaso Mascetti, Milano, Italy; ODT: Stefano Rota, Bergamo, Italy)
Fig. 8 d: Occlusal view after repeated vertical soft tissue augmentation and prosthetic conditioning (Prosthetics: Dr. Tommaso Mascetti, Milano, Italy; ODT: Stefano Rota, Bergamo, Italy) Fig. 9: Three-year follow-up after prosthetic finalization. Satisfactory phenotype modification, white and pink esthetics have been achieved
Fig. 9: Three-year follow-up after prosthetic finalization. Satisfactory phenotype modification, white and pink esthetics have been achieved
Depending on the case characteristics, the submerged implant can be subsequently restored with a second-stage surgery combined with the connection of an angled, customized abutment. Alternatively, the implant may remain submerged if, once an optimal soft-tissue architecture been achieved, a tooth-supported prosthetic solution satisfactorily meets the patient’s esthetic demands (Palombo et al. 2024).
Implant extraction and vertical bone augmentation
In cases of extreme peri-implant malpositioning that are incompatible with prosthetic correction using customized abutments (implant platform located outside the anatomical contour of the adjacent natural teeth – Class 4 peri-implant tissue deficiency – Zucchelli et al. 2019), or when treating malpositioned implants affected by severe peri-implantitis, a common therapeutic strategy involves removing the malpositioned implant and performing a vertical bone augmentation procedure.
Although vertical bone augmentation is a complex, technique-sensitive intervention, with documented risks of intra- or post-operative complications (Rocchietta et al. 2008, Urban et al. 2019, 2023a, 2023b) , it provides the great benefit of re-establishing optimal anatomical conditions for the placement of a new implant in a prosthetically guided position and delivery of an implant-supported restoration with optimal emergence profile, esthetics, and cleansability (Chiapasco et al. 2018).
Due to the severity of the baseline tissue deficiency often associated with such malpositioned implants, it is advisable to perform a preliminary soft-tissue augmentation at the time of implant removal. This creates a thick soft-tissue phenotype in the edentulous crest, facilitating both the surgical intervention and maintenance of primary intention wound closure after the surgical reconstruction.
Once the bone augmentation procedure and the new implant placement are completed, one or multiple soft-tissue augmentation procedures are often required to increase the supra-crestal soft tissue volume. This compensates for the coronal displacement of the mucogingival line caused by the previous vertical ridge augmentation procedure (Figures 10-15) (Urban et al. 2021).
 Fig. 10: Severe peri-implant soft-tissue deficiency at two adjacent implants presenting their platforms outside the anatomical contours of the adjacent natural teeth (Class IVb – Zucchelli et al. 2019), with the comorbidity of severe peri-implantitis at both fixtures
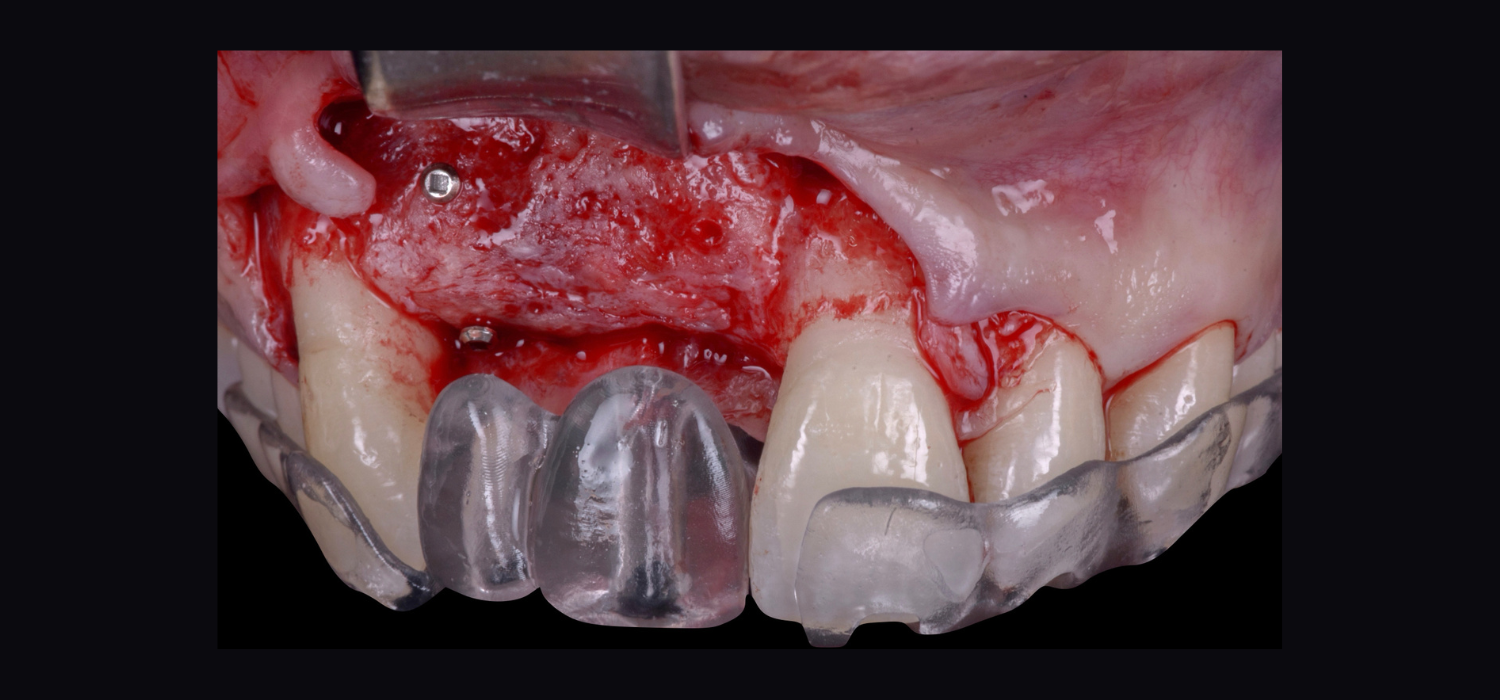
Fig. 10: Severe peri-implant soft-tissue deficiency at two adjacent implants presenting their platforms outside the anatomical contours of the adjacent natural teeth (Class IVb – Zucchelli et al. 2019), with the comorbidity of severe peri-implantitis at both fixtures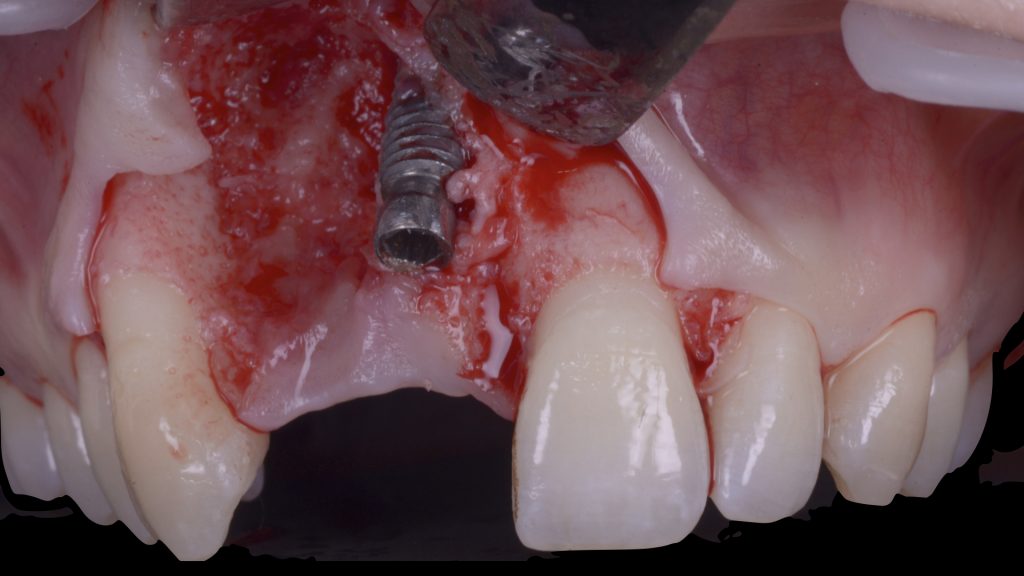 Fig. 11: First surgical procedure aiming to: a) remove the failed implants
Fig. 11: First surgical procedure aiming to: a) remove the failed implants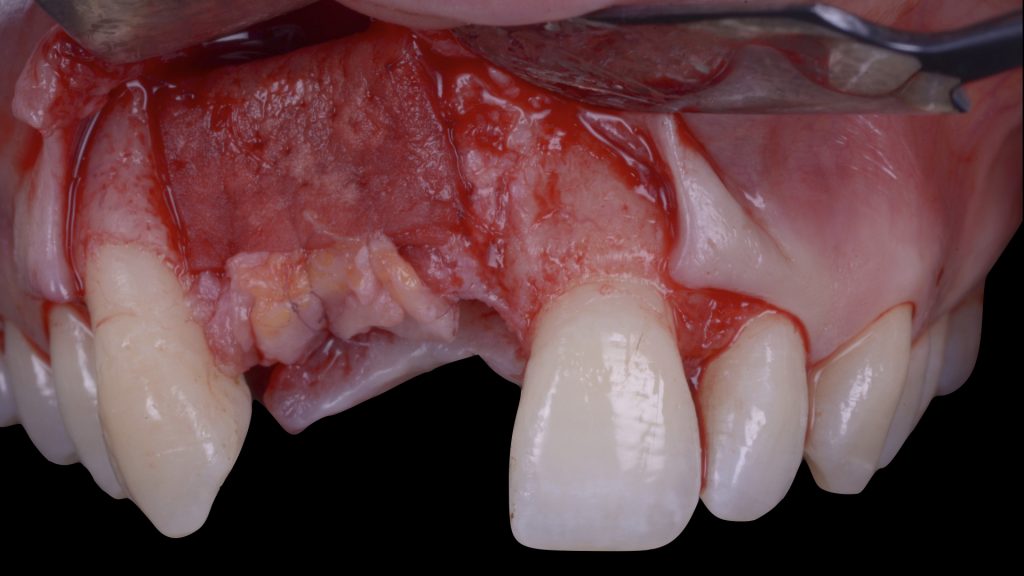 Fig. 11 b: increase the soft-tissue phenotype right after the extractions and defect degranulation using an autogenous connective tissue graft combined with a xenogeneic collagen matrix in order to facilitate flap management in the following surgical steps
Fig. 11 b: increase the soft-tissue phenotype right after the extractions and defect degranulation using an autogenous connective tissue graft combined with a xenogeneic collagen matrix in order to facilitate flap management in the following surgical steps Fig. 12: Vertical ridge augmentation (VRA) of the edentulous site: a) Flap elevation and defect degranulation
Fig. 12: Vertical ridge augmentation (VRA) of the edentulous site: a) Flap elevation and defect degranulation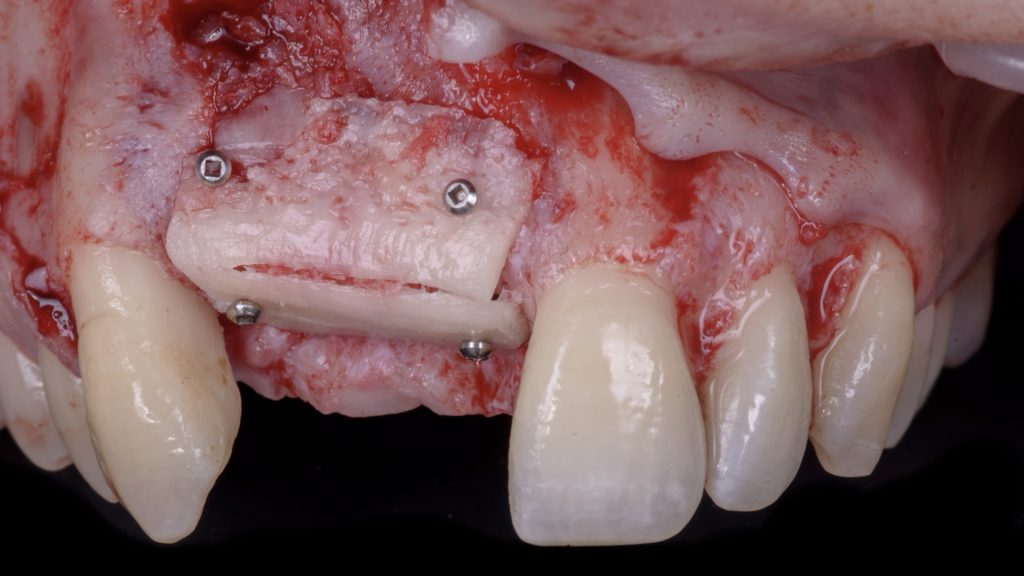 Fig. 12 b: Vertical and horizontal reconstruction using the shell bone block technique (SBBT) with pure autogenous bone harvested from the left mandibular external oblique line
Fig. 12 b: Vertical and horizontal reconstruction using the shell bone block technique (SBBT) with pure autogenous bone harvested from the left mandibular external oblique line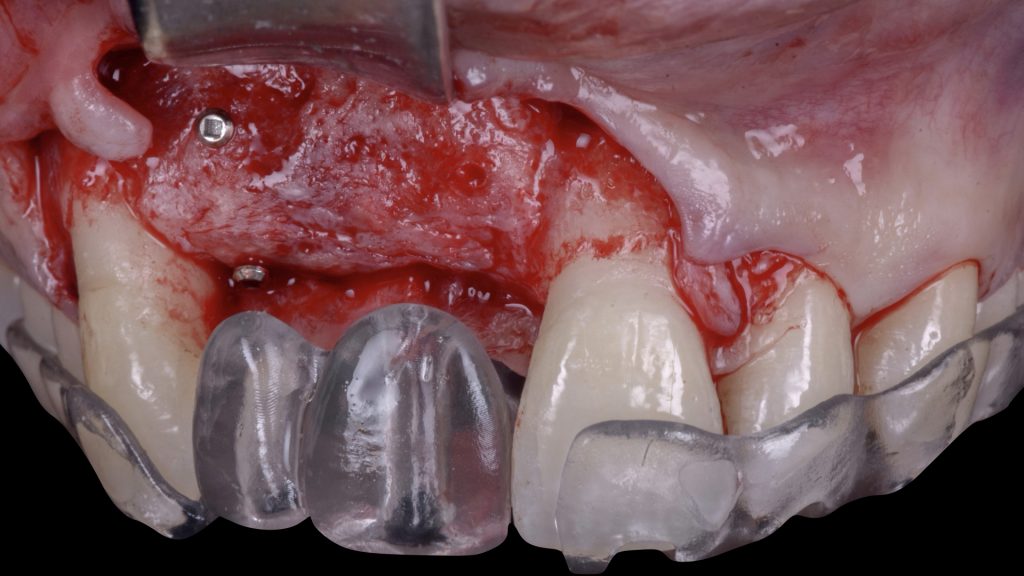 Fig. 13: Surgical re-entry 4 months after VRA: a) Flap elevation and placement of a prosthetic stent to orient the implant placement
Fig. 13: Surgical re-entry 4 months after VRA: a) Flap elevation and placement of a prosthetic stent to orient the implant placement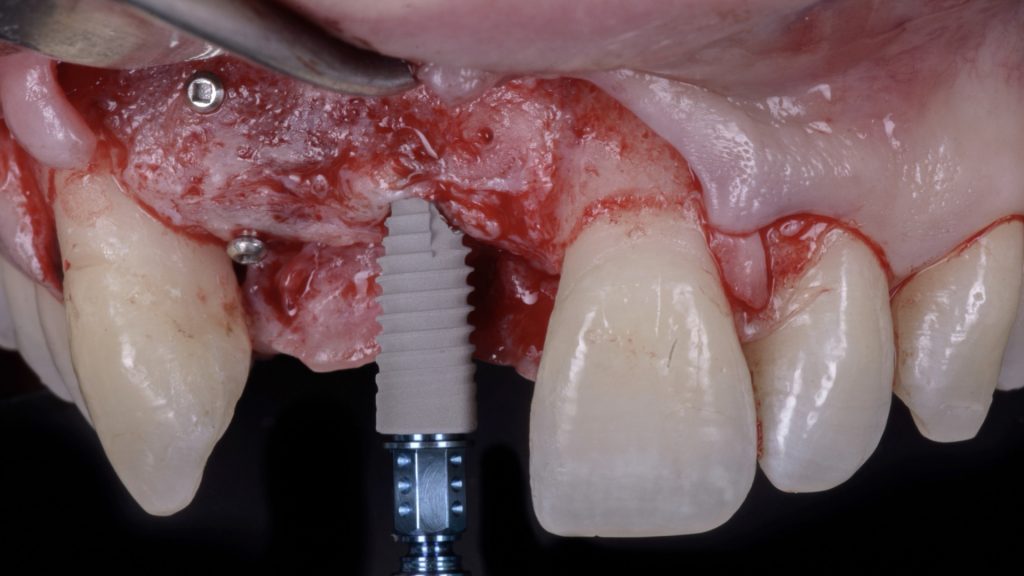 Fig. 13 b: Placement of a bone level implant at site 2.1, in a prosthetically driven position
Fig. 13 b: Placement of a bone level implant at site 2.1, in a prosthetically driven position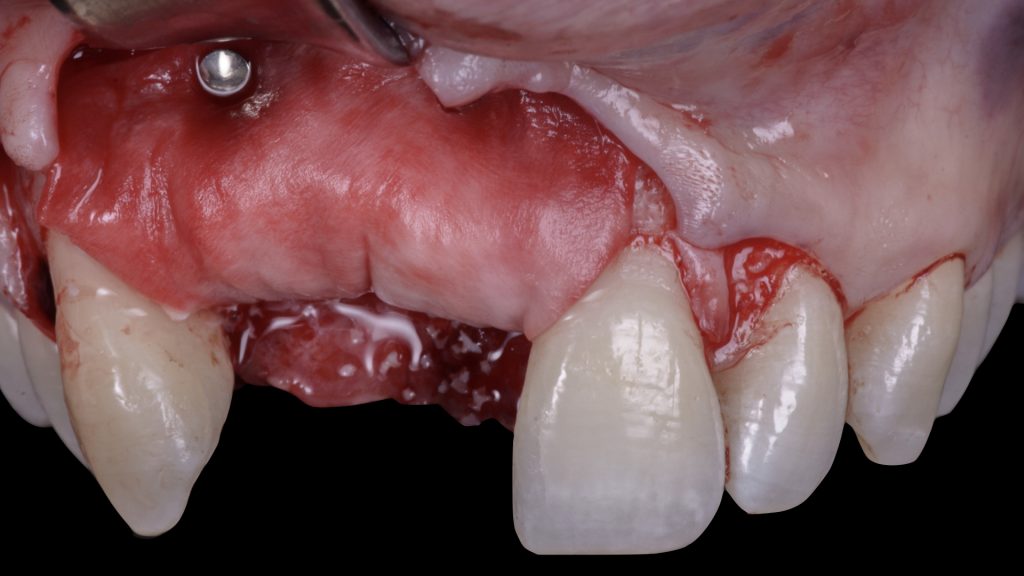 Fig. 13 c: Horizontal relining of the vertical bone augmentation using bovine bone mineral and a resorbable collagen membrane
Fig. 13 c: Horizontal relining of the vertical bone augmentation using bovine bone mineral and a resorbable collagen membrane Fig. 14: Implant second stage surgery and vestibuloplasty using a free gingival graft, 4 months after implant placement
Fig. 14: Implant second stage surgery and vestibuloplasty using a free gingival graft, 4 months after implant placement Fig. 15: One-year follow-up after implant provisionalization and beginning of orthodontic treatment. Satisfactory phenotype modification, white and pink esthetics were achieved before moving to prosthetic finalization
Fig. 15: One-year follow-up after implant provisionalization and beginning of orthodontic treatment. Satisfactory phenotype modification, white and pink esthetics were achieved before moving to prosthetic finalization
Conclusion
Peri-implant tissue deficiencies are prevalent conditions that present diagnostic and treatment challenges due to their multifactorial nature.
These conditions require a prosthetically oriented, multidisciplinary diagnostic and therapeutic approach to deliver targeted corrective interventions, facilitating surgical procedures and creating a local environment conducive to the long-term stability of peri-implant tissues. The majority of available knowledge is derived from small case series from a limited group of experts in this field. There is a clear need for comparative evidence from randomized clinical trials in diverse clinical settings to properly establish the indications and effectiveness of different therapeutic approaches.