Timing in dental implant treatment and currently available guidelines
In medicine and dentistry, timing, amongst others, is a crucial factor (Rosenberg 1999). When it comes to dental implants, timing will affect our decision-making process at many levels, but especially in terms of the final outcome that we are able to offer our patients (Funato et al. 2007).
Contemporary, evidenced-based medicine and dentistry are gaining ground not only because they are promoted by stakeholders and policy makers for the general good but, primarily, because they are focused on human biology. In other words, the cascade of biological phenomena displayed in the tissues of the oral cavity in health and disease must be respected in order to obtain successful dental implant treatment.
Besides the timing of biological processes, another fundamental aspect that affects the sequence of treatment algorithms (i.e. timing of implant placement and implant loading) reflects the esthetic demands and necessities of the patient (Vafiadis et al. 2017; Gamborena et al. 2021). The former will largely be covered by the restorative component of the treatment. As a consequence, implant treatment planning will be guided decisively by the latter (Garber & Belser 1995).
This notion is also reflected in the publications of scientific organizations such as the International Team for Implantology (ITI). Ιn their Treatment Guides series there are separate guidelines for single implant treatment in the esthetic zone (Buser et al. 2019), and partial tooth loss in the esthetic zone due to the increased risks that we need to consider when undertaking these treatments (Nugent 2013). Non-esthetic zones are considered, by and large, to be of lesser complexity and difficulty.
The present article aims to outline the effects of timing in different levels of treatment planning in the category of partial edentulism based on existing evidence.
Categorization of different aspects of treatment to facilitate planning
In science in general, and also in dentistry, we try to understand natural phenomena (Classification in Biology 1944) and also to execute complex sequences with the aid of classifications (Shima et al. 2007) . In implant dentistry, we have created several categories of different aspects so we can characterize each case and guide our decisions. Among others, we have categorized treatments based on the final prosthetic reconstructions (single/extended/full-arch) (Dawson & Chen 2019), the zone in the oral cavity (esthetic/non-esthetic) (Dawson & Chen 2019) and also types of post-extraction sockets (Chu et al. 2015; El Chaar et al. 2016). In terms of temporal categorization for the sequence of the treatment, the work of Galluci and co-workers (Gallucci et al. 2018) indicates that we need to consider two aspects: the timing of implant placement and also the timing of loading.
The possibilities for dental implant placement include:
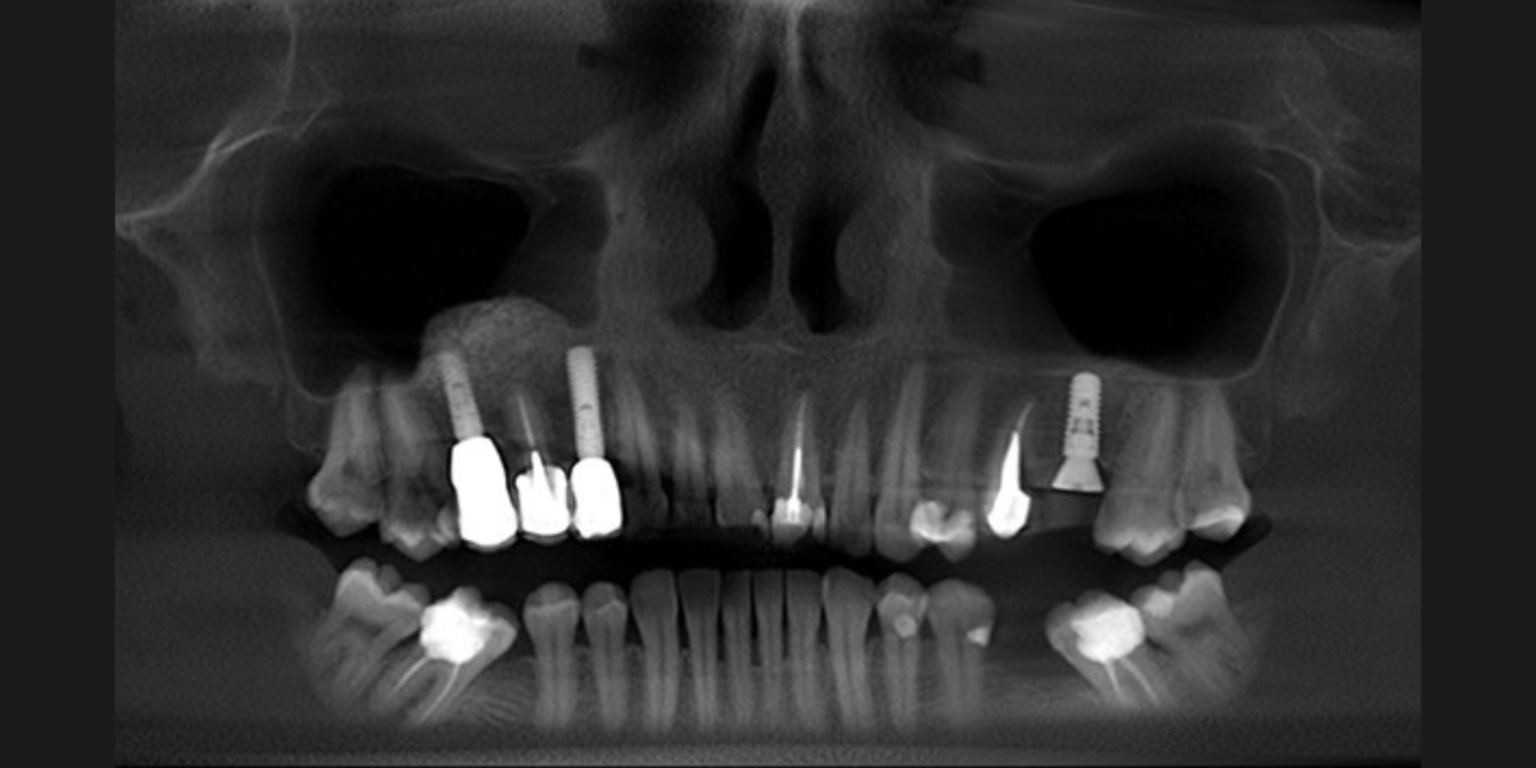
1) Immediate implant placement post-extraction (Figure 1),
2) Early implant placement with soft tissue healing (8-12 weeks, Figure 2)
3) Early implant placement with partial bone healing (12-16 weeks, Figure 3) and finally
4) Late implant placement (more than 6 months post-extraction, Figure 4).
The possibilities for dental implant loading include:
A) Immediate loading/provisionalization (< 48 hours)
B) Delayed loading (1 – 8 weeks) and
C) Conventional loading (> 8 weeks) after placement.
The two aspects can be combined in 12 ways and only some of them were considered scientifically and clinically validated. To this effect, specific criteria were used to assess the degree of validity of each protocol based on findings from the same group (Gallucci et al. 2009) and produced the combinations as follows:
1) Scientifically and clinically validated (SCV)
2) Clinically well documented (CWD)
3) Clinically documented (CD)
4) Clinically insufficiently documented (CID)
The protocols that received a “green” level (SCV) of documentation were
• immediate placement – conventional loading (1C);
• early placement – conventional loading (2-3C);
• late placement – delayed loading (4B) and
• late placement – conventional loading (4C).
The effects of the selection of one of the these combinations may lead to certain technical and biological outcomes which seem to be generally acceptable. The knowledge of the gravity and prevalence of the possible complications as well as the quantification of biological outcomes can help the clinician to avoid failure.
State of the art: effect of timing on biological outcomes in partial edentulism
In view of the European Association of Osseointegration (EAO) congress (10-12 February 2021), the review of the literature on the topic regarding the biological outcomes of implant treatment on extended edentulism was assigned to the ITI group at the Medical University of Graz (Austria). With this aim a review was designed based on the Gallucci framework. The main biological outcomes included were: radiographic bone loss, bleeding on probing, peri-implant probing depth, suppuration, prevalence of peri-implant mucositis/peri-implantitis and implant survival rate. This particular systematic review (unpublished) prepared for the European Association of Osseointegration (EAO) consensus workshop excluded single-implant and full-arch restorations due to the substantial differences at the level of both technical and biological outcomes. Importantly, and unlike in the work of Galluci and co-workers, the selection criteria mandated a minimum follow-up period of 3 years post-implant-placement.
In spite of the fact that indirect comparisons (between-study) of combined protocols are weaker compared to head-to-head comparisons, the group gathered all the available evidence by March 2020 and included both direct (within-study) and indirect (between-study) comparisons. They then used a systematic approach to grading the certainty of the evidence derived from these reports.
The most commonly reported protocols were
• late placement & immediate loading—4A: (5 randomized controlled trials, 3 prospective cohort studies, 2 prospective case series) and
• late placement & conventional loading—4C: (3 randomized controlled trials, 1 prospective cohort study, 1 retrospective cohort study, 1 retrospective case series).
allowing for direct (within-study) and indirect (between-study) comparison.
The fact that only those 2 combinations were prevalent implies that medium to long-term (> 3 years) data on biological outcomes seem to exist mostly for implants on healed sites. The protocols that contributed fewer reports included immediate placement & immediate loading—1A (one prospective cohort), immediate placement & early loading–1B one prospective cohort and late placement & early loading—4B (1 prospective cohort).
Within these limitations (high uncertainty) and the few possible (direct and indirect) protocol comparisons, the following was shown per comparison
a) late placement & immediate loading—4A vs. late placement & conventional loading—4C: protocol 4A may slightly prevent marginal bone loss (< 0.5 mm), it may not improve bleeding on probing while no major discrepancies exist in terms of peri-implant mucositis, peri-implantitis and survival rates.
b) immediate placement & immediate loading—1A vs. late placement & conventional loading—4C: protocol 1A may exhibit decreased bleeding on probing and lower survival rates.
c) late placement & early loading—4B vs. late placement & conventional loading—4C: protocol 4B may show decreased marginal bone loss, while no major discrepancies were found in terms of survival rates.
d) immediate placement & early loading—1B vs. late placement & conventional loading—4C: protocol 1B may show a moderate decrease in marginal bone loss (> 1 mm) and no major discrepancies in survival rates.
As a general comment, after late implant placement the loading protocol did not seem to affect the outcomes.
Assuming the above-mentioned conditions in terms of follow-up period (i.e., minimum 3 years), the evidence may in most cases be of very low certainty which warrants the need for well-designed comparative studies with long-term follow-ups.