Introduction
One of the most common developmental dental anomalies is tooth agenesis, which can range from absence of a single tooth to absence of the full dentition. Hypodontia describes five or fewer missing teeth (excluding third molars) and has a prevalence ranging from 2.7 to 11.6 %. It varies according to the study populations and geographical area (Celikoglu et al. 2010). Oligodontia is comparatively more rare and is defined as six or more missing permanent teeth. The prevalence is around 1% and it occurs more often in females than in males (Carmichael & Sándor 2008a). Not all teeth are affected with the same frequency: the most commonly affected being mandibular second premolars, maxillary lateral incisors, maxillary second premolars and mandibular central incisors (Raziee et al. 2020). Agenesis of a primary tooth is always associated with congenital absence of the corresponding succedaneous tooth (Mukhopadhyay & Mitra, 2014). The diagnosis of oligodontia can be made by clinical assessment accompanied by radiographs like a dental panoramic radiograph or cone beam tomography (CBCT). The lateral cephalogram is relevant for orthodontic treatment planning and determination of skeletal maturity (Carmichael & Sándor 2008a).
Etiologically, oligodontia is associated with mutations in serval genes (like variants in PAX9, MSX1, AXIN2, EDA, EDAR, and WNT10A) that influence the regulation of odontogenesis (Bonczek et al. 2021). Besides genetics, environmental factors may also play an etiological role in oligodontia (Carmichael & Sándor 2008a). Oligodontia can be accompanied by a syndrome such as ectodermal dysplasia or Down syndrome (Carmichael & Sándor 2008b).
The main clinical findings of oligodontia, besides the reduced number of permanent teeth, are malocclusion with a deep bite, crossbites, spacing, rotations, ectopic eruptions and transpositions, reduced orthodontic anchorage, cone-shaped incisors and canines, ankylosis and submergence of primary teeth. Also, alveolar growth can be limited and attrition with pulp exposure of the primary teeth can occur. Oligodontia can be associated with taurodontism, asymmetry of tooth dimensions and delayed tooth eruption in general (Carmichael & Sándor 2008a).
Patients with oligodontia complain mainly about poor mastication, compromised esthetics, malocclusion and/or spacing. Oral health-related quality of life is influenced by this diagnosis for patients and their parents as well. Raziee et al. (2020) published a prospective study evaluating 35 patients and their parents in which 77 % of the children reported that their lives were adversely affected by their dental condition, and just 43 % of the children were satisfied with the appearance of their teeth. This effect was underestimated by their parents. The findings of the study clearly underline the relevance of appropriate therapy for oligodontia because the mental health of the young patients can be adversely affected in addition to a reduction of masticatory function and esthetics.
Treatment planning should focus on the needs of the patient and take into consideration that definitive prosthodontic rehabilitation generally cannot take place before skeletal maturation. Alternative treatments, depending on the number and location of the missing teeth, can be considered, namely orthodontic space closure or sometimes also non-treatment in terms of preserving the primary dentition for as long as possible. Nevertheless, both options might be associated with disadvantages regarding functional and esthetic outcomes. If the family opts for reconstructive treatment, which means replacing the missing teeth with prosthodontic appliances, invariably a pre-prosthetic orthodontic treatment will be necessary. Aims of orthodontic treatment include establishing a class I occlusion, correct midlines and alignment, optimizing the dimensions of the restorative spaces and separation of the roots adjacent to the edentulous gaps (Carmichael & Sándor 2008a).
Dental implants are a safe and predicable option to replace the missing teeth if removable dentures are unacceptable or fixed tooth-supported bridgework would require an excessive reduction of adjacent tooth structure. The planning and insertion of implants for patients suffering from oligodontia should be realized in accordance with principles of the ITI Treatment Guides. Especially in cases requiring the placement of multiple dental implants, consideration should be given to the use of a digital surgical workflow to optimize precision. A special role might be played by stackable drilling guides that combine the bone reduction and implant insertion guides (Mijiritsky et al. 2021).
Overall, oligodontia is a comparatively rare anomaly, but it has a significant impact on the individuals affected. Its treatment is highly time-dependent and requires a multidisciplinary approach including pedodontics, orthodontics, prosthodontics and oral surgery that may oftentimes be provided advantageously in specialized dental clinics.
In Ontario (Canada), special care has been provided for young people with oligodontia by the dental teams at Holland Bloorview Kids Rehabilitation Hospital and its partner institution The Hospital For Sick Children for more than 30 years. An ongoing research project at these two institutions funded by the ITI qualitatively explores patients’ own view of dental implant treatment, and the impact of this treatment on their lives as well as their parents. The primary study results indicate that difficulties for patients and their parents include diagnosis of oligodontia, understanding the treatment plan and access to appropriate care. Young people are unaware of dental issues in early childhood until emotional challenges start in middle school. Family members are the main support resource over the course of treatment, and both patients and parents reported a high level of satisfaction with the treatment outcome. In brief, the dental implant treatment outcome outweighs the hardships endured over the arduous dental journey by young adult patients with oligodontia and their parents. A treatment guide for patients and their families by experienced multidisciplinary specialists has also been drafted based on the study results and clinical experience at Holland Bloorview.
We would like to present two cases that were treated in the Ontario Cleft Lip and Palate/Craniofacial Dental Program at Holland Bloorview.
Case 1: Oligodontia with seven missing teeth in all four quadrants
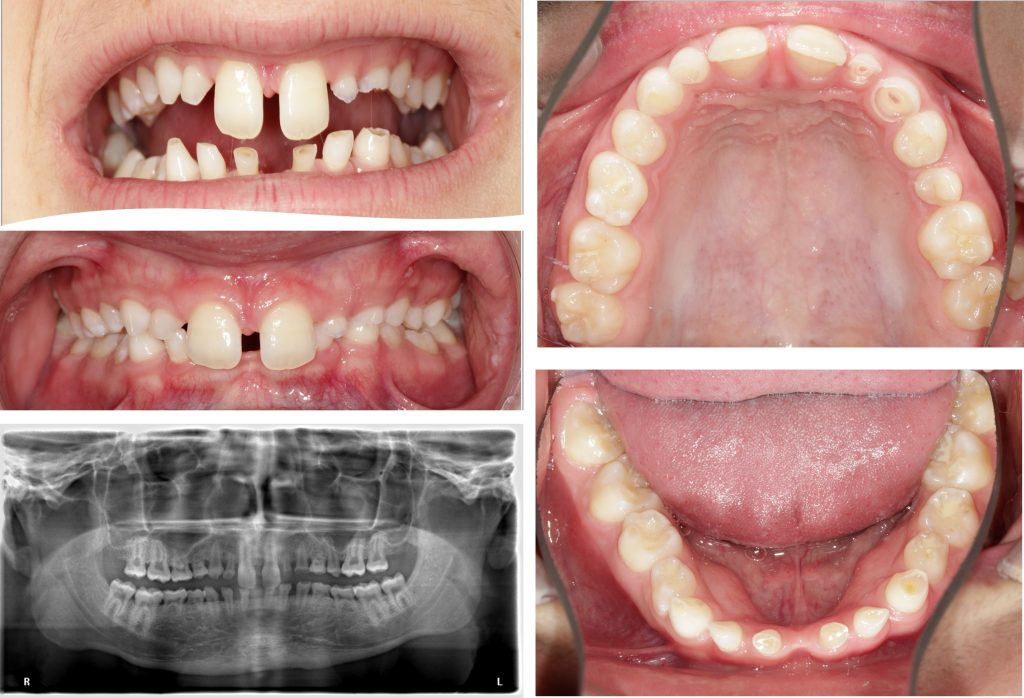
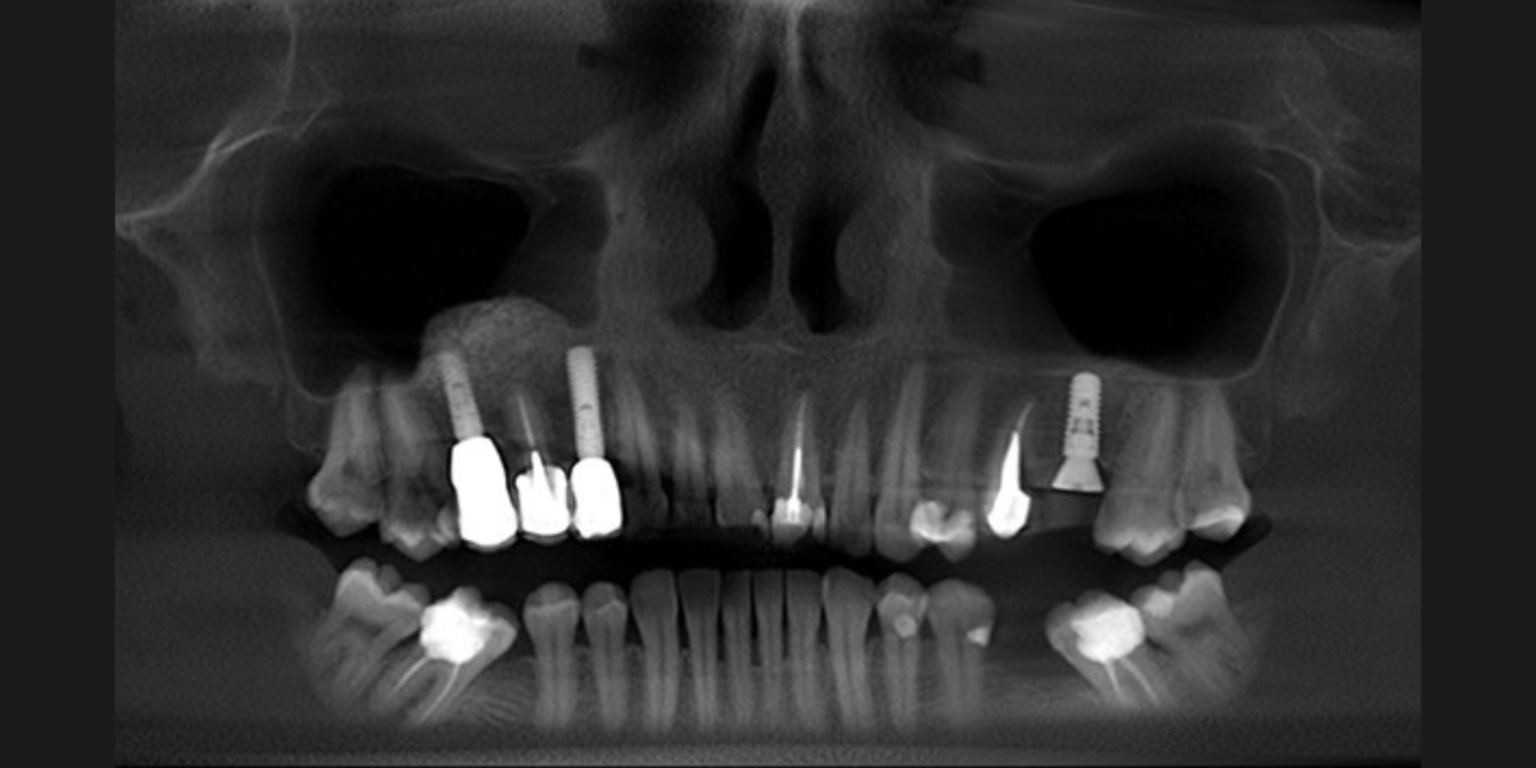
This 12-year-old boy was referred by his family dentist due to retention of primary teeth and a peg-shaped maxillary lateral incisor. The dental panoramic radiograph showed seven missing permanent teeth, transposition of teeth 23 and 24, and absence of wisdom teeth. Besides oligodontia, no other medical issues were reported, and a family history of oligodontia was negative. During adolescence, his dentition was aligned orthodontically (Fig. 1). Tooth 16 developed caries and received endodontic treatment which eventually failed. Serial cephalometric analysis indicated that by age 20 his skeletal growth was largely complete. The family chose to pursue a reconstructive treatment comprising replacement of missing teeth by means of dental implant-supported crowns and bridges (Fig. 1). The treatment plan was formulated on the basis of an interdisciplinary dialogue between orthodontists, prosthodontists and oral and maxillofacial surgeons, as recommended for all complex cases involving oligodontia. The care plan for this young adult was to extract the retained primary teeth 55, 54, 64, 75, 85 and tooth 16, and to insert 7 implants to support a prosthodontic rehabilitation comprising crowns at sites 12, 14, 22, 25, 35 and 45 and a 2-unit cantilevered bridge retained at 16.

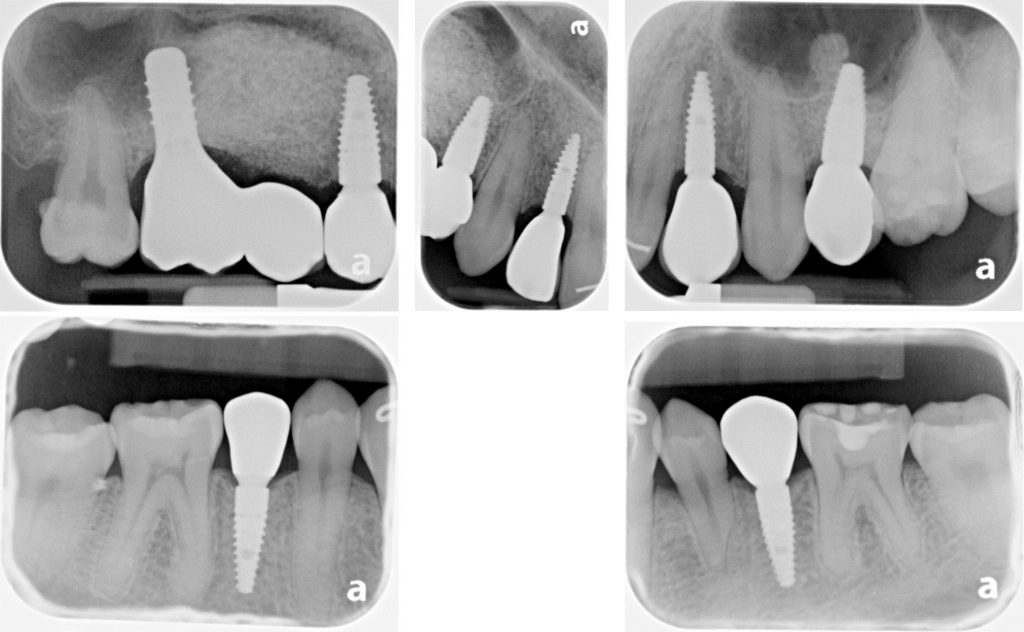
After fabrication of immediate maxillary and mandibular vacuum-formed provisional retainers with resin pontics to replace the missing teeth, the patient underwent extraction of teeth 16, 55, 54 and 64. A CBCT was provided for computer-aided, template-guided implant surgery. Before implant insertion, guided bone regeneration (GBR) using xenogenic and allogenic biomaterials was performed at sites 14 and 16 in addition to an indirect sinus floor elevation with application of a collagen plug and GBR performed at site 25. Implants were inserted 6 months later at sites 16 (Straumann Standard Plus WN), 14, 12, 23, 25, 75, 85 (Straumann BLT). In the maxilla the implants healed while submerged (Fig. 2), whereas in the mandible healing took place in an open fashion.

After 8 months, exposure of implants in the maxilla and connection of healing caps took place. Surgeries were conducted under general anesthesia using naso-tracheal intubation. One month following uncovering of the maxillary implants, digital impressions and bite registration of the dental arches with scan bodies attached to the implants were obtained using an intra-oral scanner (iTero®). Ceramic/zirconia crowns and bridge as described in the care plan above were luted on Variobase abutments (Straumann) using resin cement (ESPE Rely-X Unicem 2), and restorations were installed at 35 Ncm torque with Teflon tape and composite resin placed in screw access channels. The follow-up examinations at 1 and 2 years revealed a satisfied patient, stable occlusion and no signs or symptoms of peri-implantitis, and periapical radiographs demonstrated crestal alveolar bone levels within normal limits at all implants (Figs 3 – 4). Future follow-up will continue annually in parallel with regular care by the patient’s general dentist and dental hygienist.

Case 2: Severe oligodontia of 17 missing teeth and need for pre-implant alveolar bone reduction
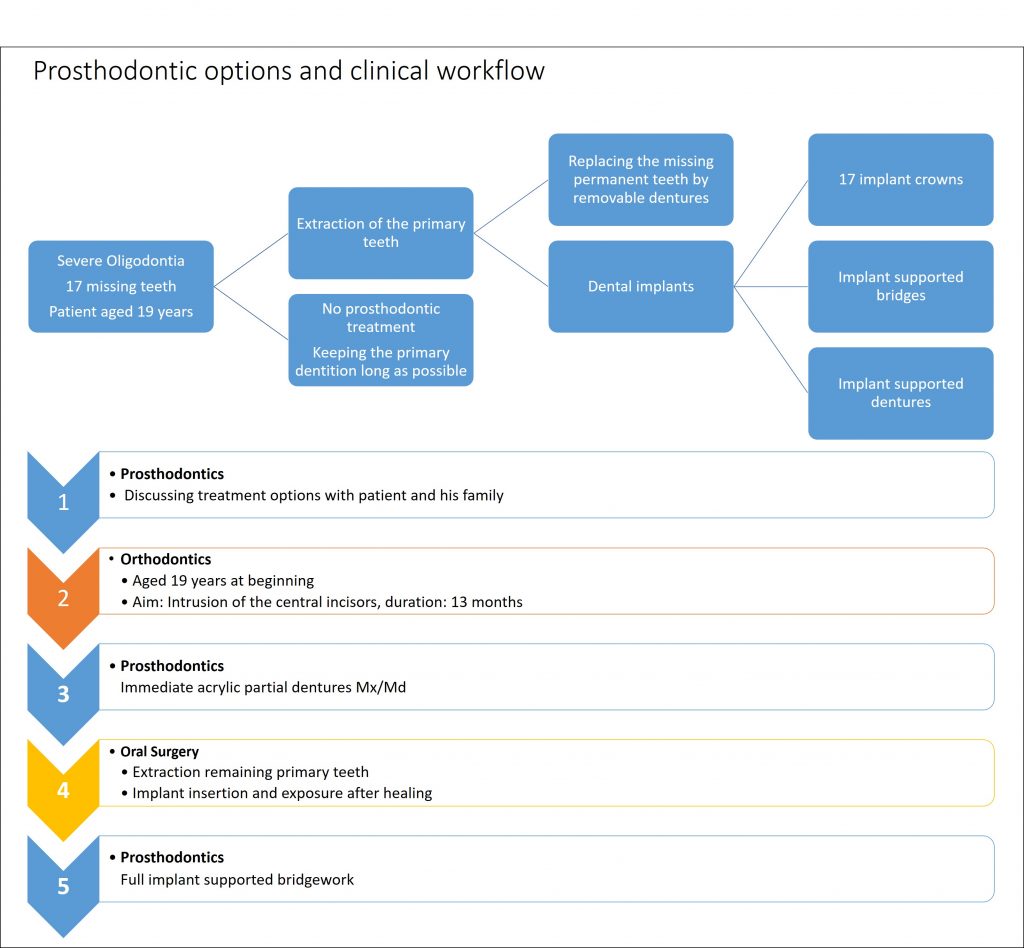
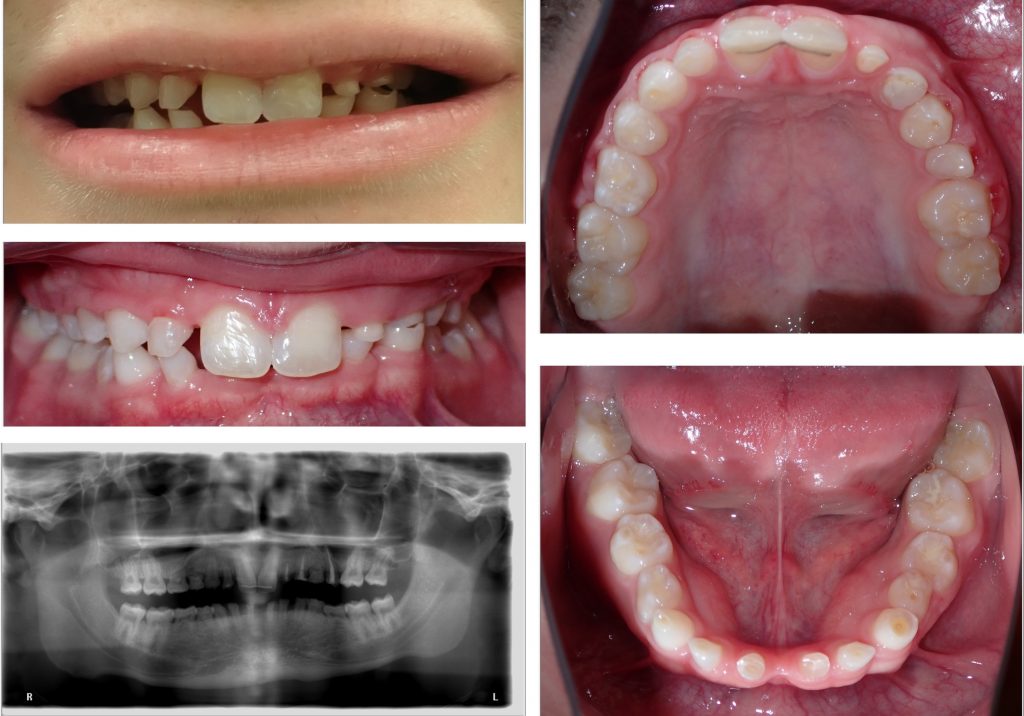
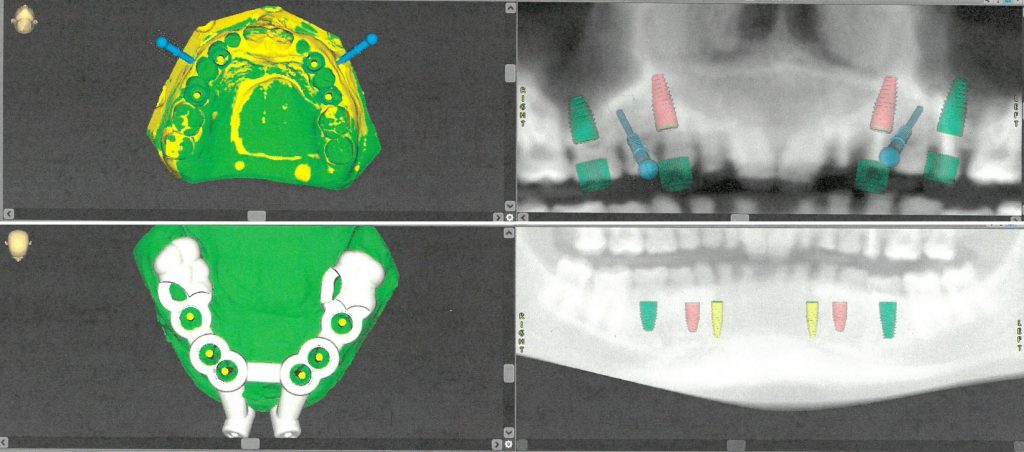
A 14-year-old male was referred by his general dentist due to increased dental attrition and assumed severe oligodontia. He demonstrated a phenotype manifestation, including tooth and hair abnormalities, suggestive of an ectodermal dysplasia. Genetic testing revealed a heterozygous WNT10A gene mutation. Clinically he was in the mixed dentition stage with retained primary teeth 55, 54, 53, 52, 62, 63, 64, 75-85, attrition of many of the retained primary teeth and compensatory eruption of worn teeth, and erupted permanent teeth 17, 16, 11, 21, 25, 26, 27, 36, 37, 46, 47. He demonstrated a class II malocclusion with a retrognathic mandible, 100 % overbite and 5-mm overjet. His oral hygiene was good, and caries lesions were not detected. He exhibited a wide maxillary diastema and excessive show of the maxillary incisors (Fig. 5). The dental panoramic radiograph demonstrated 17 missing permanent teeth (12, 13, 14, 15, 22, 23, 24 and 35-45) and absence of wisdom teeth. Obturated root canals were identified in teeth 62, 63 and 25, and tooth 25 exhibited periapical rarefaction. The prosthetic options were presented to the family as set out in Fig. 6, and a decision was made to proceed with implant-supported bridges in the maxilla (12-15 and 22-25) as well as mandible (35-45). The initial aim was to orthodontically align his dentition including intrusion of the maxillary central incisors using fixed orthodontic appliances (Fig. 7). Following the conclusion of orthodontic therapy, a CBCT was obtained, and computer-aided, template-guided implant surgical planning was performed virtually using CoDiagnostiX 10.2 software (Dental Wings, Montreal, Canada) (Fig. 8).
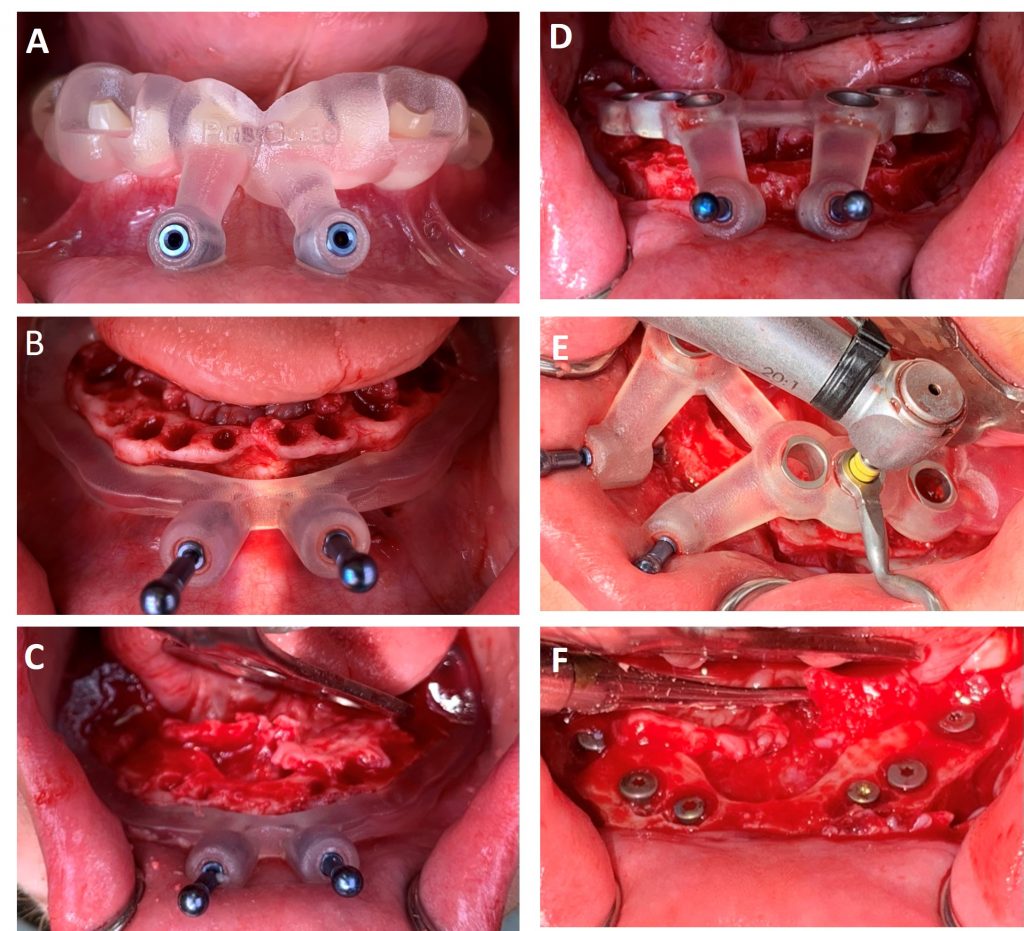
Digital surgical planning revealed the need for sinus floor elevation and contour augmentation on both the right and left sides of the maxilla. The planning also predicted that, as a result of the compensatory eruption of the mandibular dento-alveolar process secondary to attrition of retained primary teeth, the resulting restorative space following primary tooth removal would be insufficient to accommodate prosthetic hardware and to provide for an esthetic outcome. Consequently, the need for crestal alveolar bone reduction was determined. Thus, in addition to fabricating a maxillary implant drilling guide, a stackable surgical guide was fabricated for the mandible incorporating an anchor-pin drilling guide, a bone-reduction guide, and an implant drilling guide.
The surgery was performed under general anesthesia as an outpatient procedure (Fig. 9). Firstly, tooth-supported anchor pin guides were seated and drilling pin osteotomies were created in both arches. Secondly, all retained primary teeth (55, 54, 53, 53, 62, 63, 64, 75-85) and tooth 25 were extracted. Thirdly, a sinus floor elevation and augmentation of both maxillary sites was performed. Fourthly, an implant drilling guide was inserted into the maxilla using the previously drilled pin osteotomies to place two temporary pins for precise and stable fixation. Implants (Straumann Bone Level Tapered Roxolid® SLA®) were then inserted at sites 13 and 23, whereas the insertion of 15 and 25 were postponed following sinus floor augmentation. Fifthly, in the mandible, a full muco-periosteal flap was created and the bone reduction guide was seated using two anterior pins and the posterior molars. The alveolar bone height was reduced as planned pre-surgically per the bone reduction guide. Sixthly, following removal of the bone reduction guide, the implant drilling guide was fixed using the same drilling pin osteotomies and posterior teeth. Implants at sites 36, 34, 33, 43, 44 and 46 (Straumann Bone Level Tapered Roxolid ® SLA ®) were inserted and all wounds closed by suturing (Fig. 10). Immediate acrylic resin provisional partial upper and lower dentures, fabricated in advance, were inserted and worn for the next six months until the final implants could be inserted at sites 15 and 25. The prosthetic workflow will follow the steps outlined in Case 1 above.

Summary
Oligodontia describes six or more missing permanent teeth and belongs to the developmental dental anomalies in humans. Typically, clinical main findings are retained primary teeth, and the diagnosis can be derived from a radiological analysis of dental panoramic radiographs. Due to the rarity of the condition, treatment in specialized, multidisciplinary centers might be advantageous. Usually, patients need interdisciplinary dental care involving prosthodontics, orthodontics, pedodontic dentistry and oral and maxillofacial surgery. In this way funding programs like the “Ontario Cleft Lip Palate Craniofacial Program” are an excellent example how the treatment quality of patients and their oral-related quality of life can be improved.
A primary challenge is the aspect of growth because permanent prosthodontic rehabilitation cannot be done before the patient finishes growing. Depending on the location of the missing teeth, this can affect the wellbeing and social life of the patients. Often temporary prosthodontic solutions are required during adolescence. Dental implants are an integral part of permanent oral rehabilitation because they enable the stable fixation of crowns or bridges without sacrificing tooth structure on the adjacent teeth. Additionally, young patients are usually not affected by diseases that have a limiting effect on the implant survival rate, and most of them are highly motivated to maintain their implants. This leads to a high long-term success rate of dental implants in patients suffering from oligodontia. The implementation of a digital implant planning workflow is advantageous due to the increased precision of implant placement and its predictability. Tools like a digitally designed guide for alveolar bone reduction are valuable options and an example of the continuously developing treatment concept for oligodontia.