Introduction
The successful outcome of an implant is based on the definitive diagnosis and precise, customized treatment plan that is best for the individual. It involves various steps starting with the treatment plan. This phase begins with an initial discussion between the surgeon (Lane-Fall & Fleisher 2018), prosthodontist and periodontist. Preliminary procedures including operative and periodontal procedures should be completed. If oral hygiene is poor, patients may need to make improvements and have to be evaluated over a 6-to-12-month period. In the course of this preparatory phase, some patients may be found to be inappropriate candidates for implant reconstruction. Alternative methods such as a fixed prosthesis, removable partial dentures or full dentures may be indicated (Budtz-Jörgensen 1996)
It is important to consider prosthetic and surgical factors before planning the implant case (Budtz-Jörgensen 1996; Misch & Wang 2008). All the factors have to be incorporated into the treatment plan. They also have to be checked and any alternatives or other procedures have to be considered ahead of time for proper success and the survival of the implant. It is difficult to consider all the factors at once, particularly for undergraduates as they are beginners in implant dentistry. With this in mind, in 2009 the ITI created a tool known as the SAC Assessment Tool (Dawson et al. 2022).
The SAC classification – Straightforward, Advanced Complex – checks various factors and considers all the prosthetic and surgical complications along with the esthetic expectations of patients. This system thus functions as a clinical decision-making system to classify cases. It establishes the degree of complexity of cases and produces a report showing which category the case falls into. The SAC tool ticks all the boxes, especially the various criteria and factors that need to be planned prior to the surgical implant procedure. It also helps in providing a comprehensive treatment plan that takes the bone, soft tissue and the prosthetic factors into consideration (Dawson et al. 2022).
The aim of this study is to assess the accuracy of implant planning using the SAC Assessment Tool with undergraduate students during implant planning.
Materials and methods
100 students were involved in the study . They were given three cases, ranging from straightforward to complex. Each student had to carry out a diagnosis and treatment planning first without and then with an SAC tool assessment. After the test was carried out, the students were given a set of questionnaires to assess their level of competence in diagnosis and treatment planning. The results were tabulated and subjected to statistical analysis.
The three cases covered patients with edentulous sites, one in the esthetic anterior region, and the students evaluated the cases, assigning what they believed to be probable outcomes using the SAC tool.
The results were as follows
PATIENT 1 – STRAIGHTFORWARD CASE
PATIENT 2- ADVANCED CASE
PATIENT 3 – COMPLEX CASE
The above findings were obtained by the observer and were compared with the findings of the undergraduate students. As UG students in our institution do implant cases from the third year of study, they have basic knowledge of how to proceed with cases and carry out a diagnosis.
They were asked to assess the difficulty level of the cases provided based on various factors. The three cases dealt with different sites and clinical scenarios, and each student took around 15 mins (approx.) to assess the case and prepare a proper treatment plan.
The students were then asked to complete a diagnosis for each clinical scenario with the SAC tool . This led them to recognize all the factors which they had not considered while planning for the case in their first assessment.
After the study was done the students were provided with a questionnaire to define how the SAC tool helped them through the diagnosis of the implant planning.
Among them the major questions were :
- Is it easy to use the tool?
- How much did the tool help in analyzing the case?
- Self-evaluation?
Results
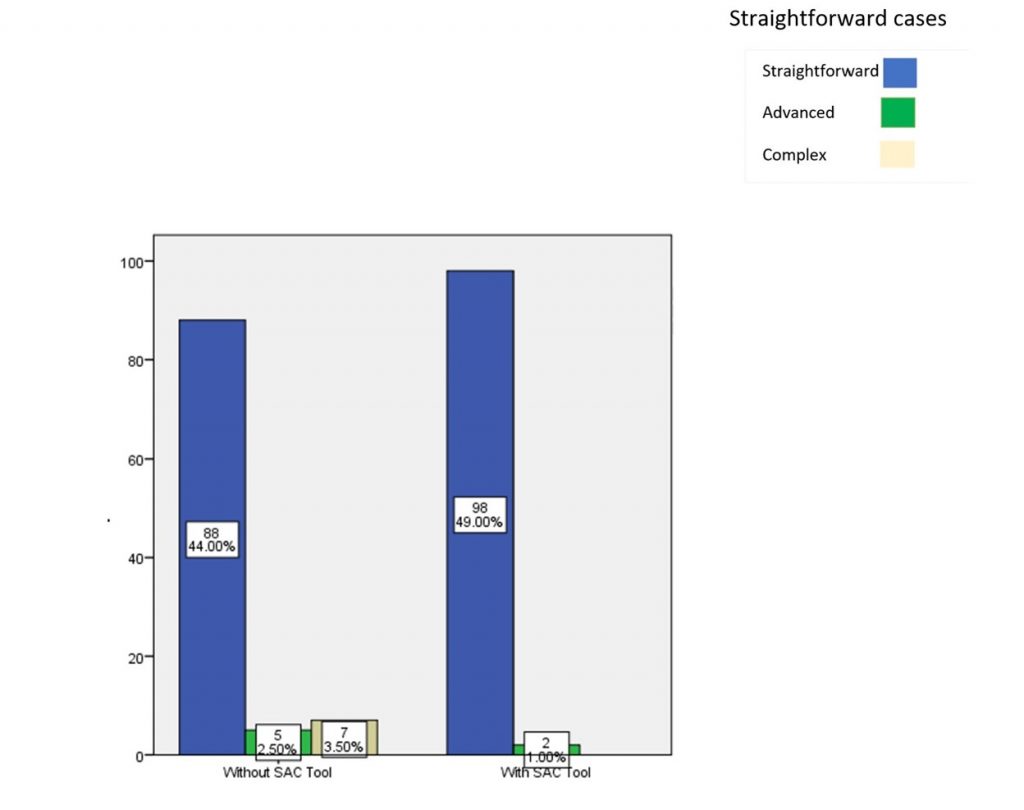
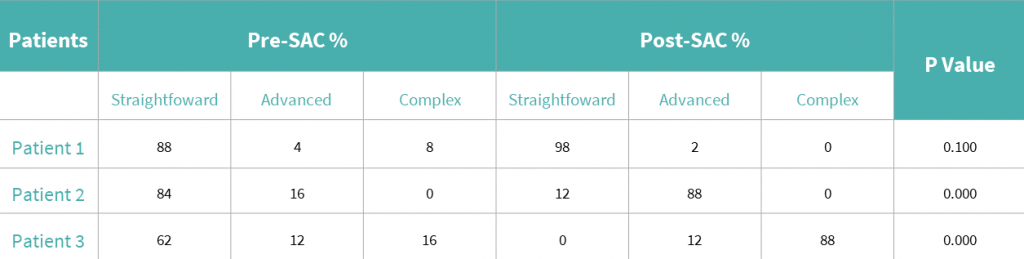
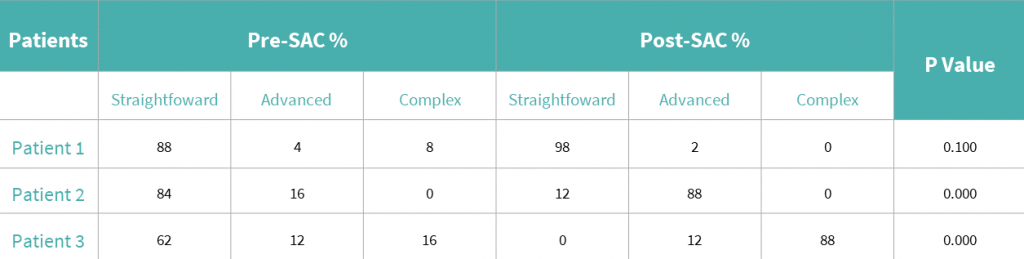
The results for the straightforward case provided are as follows when assessed without SAC tool 88 – straightforward, 5 – advanced, 7 – complex. When they were provided with the SAC tool the results were as follows 98 – straightforward, 2 – advanced, 3 – complex. The straightforward case did not lead to a significant result (graph 1 & table 1).
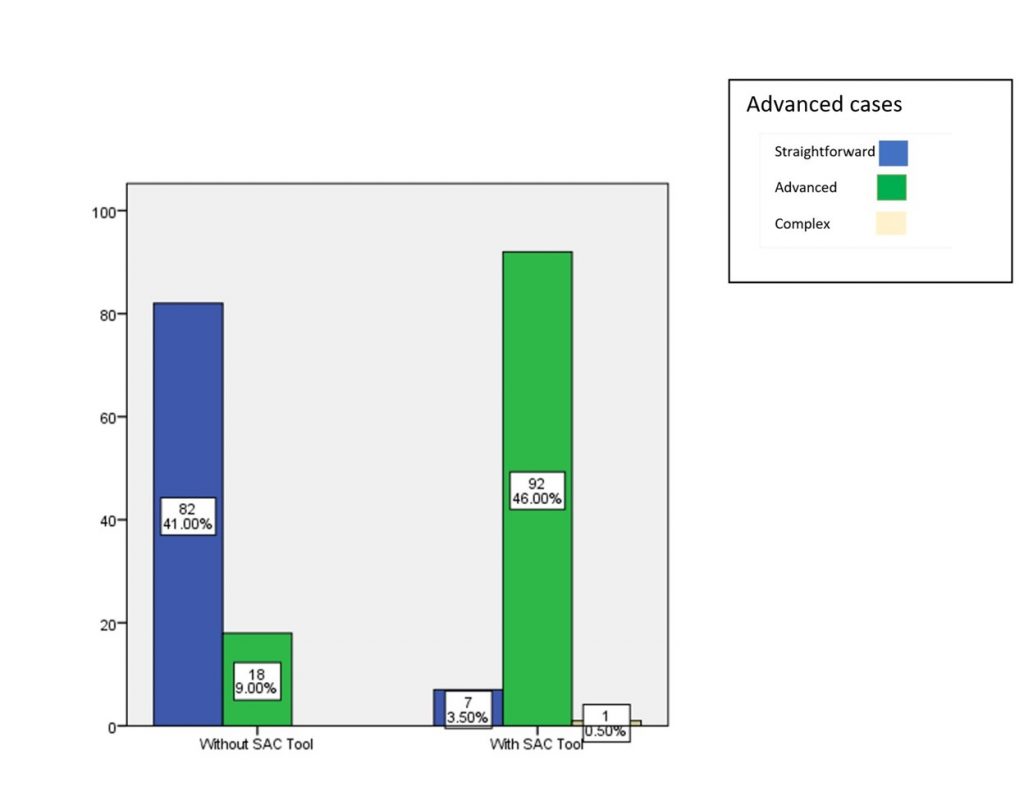
The results for the advanced case when assessed without SAC tool were 82 – straightforward, 18 – advanced, 0 – complex When they were provided with the SAC tool the results were as follows 7 – straightforward, 92 – advanced, 1 – complex. There was a significant result for the advanced case (graph 2 & table 1).
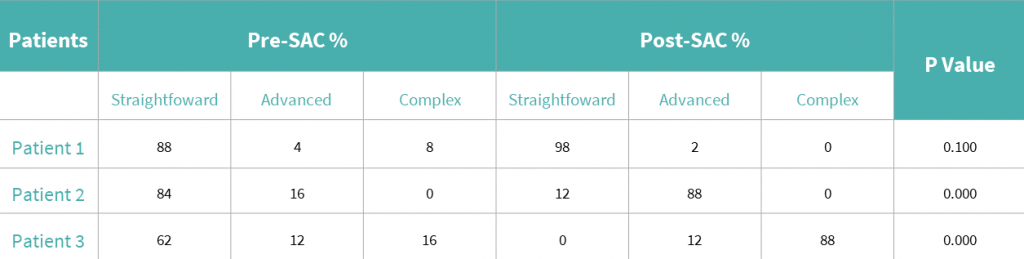
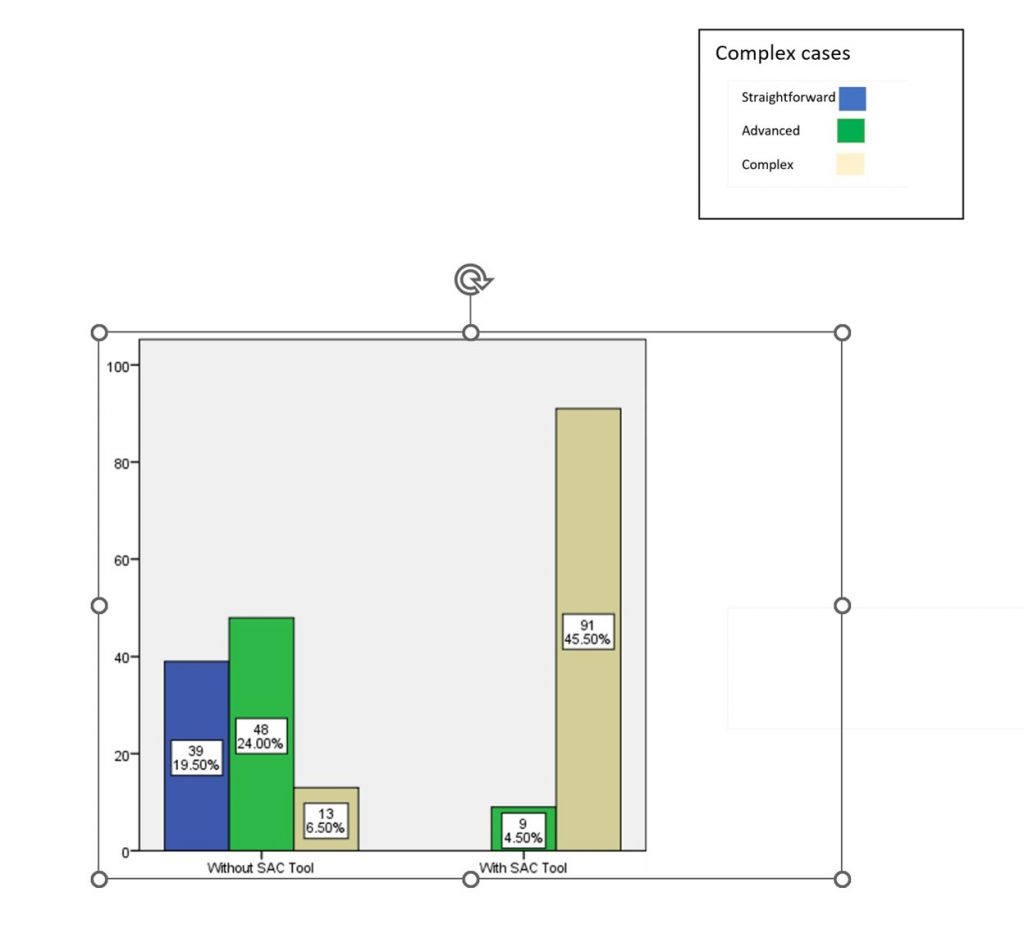
The results for the complex case provided when assessed without the SAC tool were 39 – straightforward, 48 – advanced, 13 – complex. When they were provided with the SAC tool the results were 0 – straightforward, 9 – advanced, 91 – complex. The result was significant for the complex case (graph 3 & table 1).
Discussion
The success rate and the clinical survival of the prosthetic rehabilitation with dental implants for fully or partially edentulous areas are high (Misch & Wang 2008). The SAC classification system acts as a tool to support the clinical decision by systematizing the risk factors of a rehabilitation with dental implants (Correia et al. 2020). All the patients were selected from the institution only.
The SAC Assessment Tool takes users through each step necessary to identify the degree of complexity and potential risk involved in individual implant dentistry cases in an easy-to-use process. This tool makes use of the ITI’s highly regarded classification system referred to as SAC: Straightforward, Advanced, Complex. It reflects the normative guidelines developed by the ITI for various types of restorative and surgical cases. The tool is based on the book entitled “The SAC Classification in Implant Dentistry 2nd Edition”, published by the ITI in cooperation with Quintessence Publishing Group.
The success rate and clinical survival of prosthetic rehabilitation with dental implants for fully and partially edentulous areas are high (Correia et al. 2020; Dhingra 2012). However, it is necessary to be aware of the risks and complications inherent in this type of treatment in order to avoid failures associated with diagnostic errors and to design the best treatment plan for the patient. The SAC classification system acts as a tool to support clinical decision-making by systematizing the risk factor of rehabilitation with dental implants.
Mattheos et al. reported that it is necessary to introduce some uniformity among the oral implantology programs (Correia et al. 2020; Mattheos et al. 2014). For example, the EAO certification/diploma in implant dentistry and the ITI Curriculum are educational programs that may lead to a more standardized approach to implant dentistry education of higher quality, which is very important for increasing clinical success rates and to promote the scientific domain in implant dentistry.
A previous study was about the agreement level of the treatment plan provided by the SAC tool with different users (Dhingra 2012; Mattheos et al. 2014). This is the first study to include undergraduates that also aims to create awareness among dentists at a beginner level about the parameters that have to be evaluated for successful implant treatment planning. This study made undergraduate students consider many other factors that they previously left out when creating their treatment plan for a particular case. Therefore, this particularly helps implant dentists at a beginner level and it also potentially considerably improves the treatment given to the patient. More cases for each category should be included in future studies.
Conclusion
Within the limitations of our study, although there were no significant results for straightforward cases, the SAC tool gives significant results for complex and advanced cases (p<0.05). It can therefore be considered a valid and efficient way to educate dentists with less experience in implant dentistry and ultimately improve patient care.
Acknowledgement
We would like to thank all the participants who took part in the study. We also thank Saveetha dental college and hospitals for their continuous help and support.
Author contribution
First author (S. Karthickraj) performed the analysis and interpretation and wrote the manuscript. Second author (R. Subhashree) contributed to the concept, data design, analysis, and interpretation, and also critically revised the manuscript. Third author (N. Thiyaneswaran) critically reviewed the manuscript. All the authors discussed the results and revised the manuscript.






