Introduction
Implant overdentures (IOD) are a widely used treatment modality that tends to have a positive impact on patients’ quality of life (Srinivasan et al., 2023). They can be categorized as implant-supported overdentures, where the entire support comes from the dental implants, or as implant-retained, where the support is shared between dental implants and the oral tissue (Layton et al., 2023). Although dental implants improve many characteristics, implant overdentures still follow the basic principles of conventional complete dentures.

Prosthodontic Planning and Procedures
The literature has emphasized the importance of using two implants for mandibular implant overdentures and four for maxillary implant overdentures (Kern et al., 2016; Messias et al., 2021). This results in higher success rates at both the implant level and the prosthesis level as well as high patient satisfaction (Abou-Ayash et al., 2023). The choice of a two-implant overdenture in the mandible (2-IOD) is widely accepted as the standard of care for the edentulous mandible (Feine et al., 2002; Thomason et al., 2009). More recently, the need for more conservative options with reduced patient morbidity has led to the use of implant overdentures with fewer implants or with the use of mini-implants with mixed results (Nogueira et al., 2021; Marcello-Machado et al., 2018). Several systematic reviews have explored implant survival for implant overdenture treatment. In the edentulous maxilla, five-year implant survival can range between 75.4-89.1%, with the higher survival percentage observed when at least four implants with a rough surface are used (Kern et al., 2016; Andreiotelli et al., 2010). In the edentulous mandible, five-year implant survival ranges between 98.8-100% (Kern et al., 2016; Sailer et al., 2022).

Prosthodontic Planning and Procedures
Implant Configurations for Full-Arch Removable Dental Prostheses
For an edentulous arch, a removable implant prosthesis may be chosen over a fixed implant prosthesis for various reasons. These can include:
- Need for facial support by means of an acrylic flange
- Improved hygiene access for patients and carers
- Flexibility in denture design and retention type, easier to “downgrade”
- Reduced initial cost
- Implant malpositioning
- Severe arch discrepancies
(Sadowsky et al., 2015; Muller and Barter 2016; Mericske-Stern et al., 2000)

Prosthodontic Planning and Procedures
Fixed vs. Removable Prosthodontics for Restoring the Edentulous Maxilla
Although implant overdentures are a very good (and often the only) option for patients, with accompanying high satisfaction rates, they are also linked with high rates of complications (Goodacre et al., 2003; Andreiotelli et al., 2010).
Common implant overdenture complications include:
- Loss of retention and need for adjustment
- Need for reline
- Loss of implants (higher rate in maxilla)
- Clip/attachment wear
- Clip/attachment fracture
- Prosthesis wear
- Prosthesis fracture
Favorable implant position, patient compliance, adequate prosthetic space, and metal reinforcement of the overdenture are amongst the factors that play a role in reducing the complication rates of implant overdentures (Papaspyridakos et al., 2012; Trakas et al., 2006).


Implant overdenture attachment types
Implant overdentures generally have two types of implant attachment that provide retention, support, and stability. These are free-standing implant attachments and bars, and they present advantages and disadvantages (Table 1).
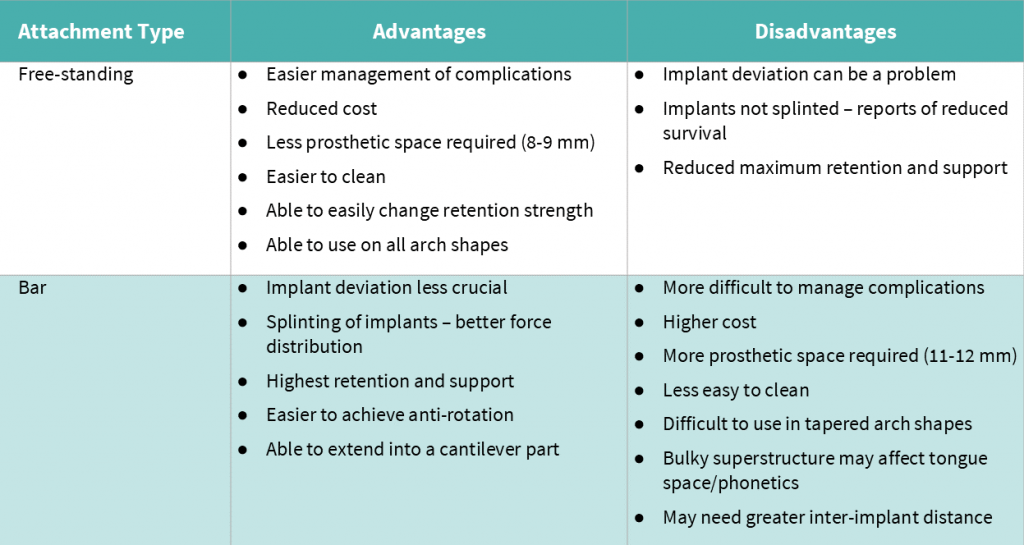
Several factors contribute to the final choice of attachment type. Among them are the patient preference, clinician preference, prosthetic space, and implant position.
In terms of the patient preference, the recent ITI Consensus Conference reported that there is no difference between the use of a bar or free-standing attachment-retained overdentures in patient-reported outcomes, when two implants in the mandible or four implants in the maxilla are used (Abou-Ayash et al., 2023).
Some clinicians prefer to splint implants when possible, using overdenture bars as this leads to better force distribution. However, a number of systematic reviews have shown that there is no difference in implant survival between splinted and non-splinted overdenture design (Kern et al., 2016, Leão et al., 2018, Di Francesco et al., 2019). In a systematic review, Anas El-Wegoud et al., (2018) concluded that there is insufficient evidence to support any of these treatment modalities. Free-standing attachments seem to be a more popular choice among dentists (Sailer et al., 2022).
Ahuja and Cagna (2011) classified the available prosthetic space (from the soft tissue crest to the proposed occlusal space) for implant overdentures into four categories: Class 1 is equal or greater to 15 mm, Class 2 is between 12 and 14 mm, Class 3 is between 9 and 11 mm, and Class 4 is less than 9 mm. Classes 3 and 4 may not provide adequate space for a bar unless changes in the occlusal vertical dimension, occlusal plane position, or alveolar anatomy are performed.
Malpositioned implants pose a challenge for implant overdentures. If standard free-standing attachments are used then the path of insertion of the female insert may mean that it can be difficult or impossible to seat the denture. In such cases the alternatives are to:
- use a bar
- use free-standing attachments with angle correction
- use transmucosal multi-unit abutments with angle correction
The advantages of using free standing attachments with angle correction are that a single component can be used, which can be torqued once and then not removed again, thus ensuring the soft tissue attachment is not disturbed. There are several options for such abutments on the market.
The case report below outlines a step-by-step approach for the choice of such abutments, and the eventual rehabilitation with an implant-retained maxillary overdenture.
Case report
A 28-year-old man attended the clinic seeking restoration of his previously placed implants. He had a history of oligodontia and was edentulous by the age of 23 years. He had six implants placed in the maxilla, following an iliac crest bone graft, and six implants in the mandible. He was using a complete maxillary denture only and had not had any implant restorations as he moved to a different city after the surgeries. His main concern was to have the implants restored and have some teeth, with as little intervention as possible.





The treatment plan included:
- Oral hygiene instructions
- Explantation of the UL3 implant, non-surgical peri-implant treatment
- Maxillary implant-retained overdenture using angle-corrected free-standing attachments
- Mandibular metal-acrylic fixed prosthesis
- Lifelong maintenance
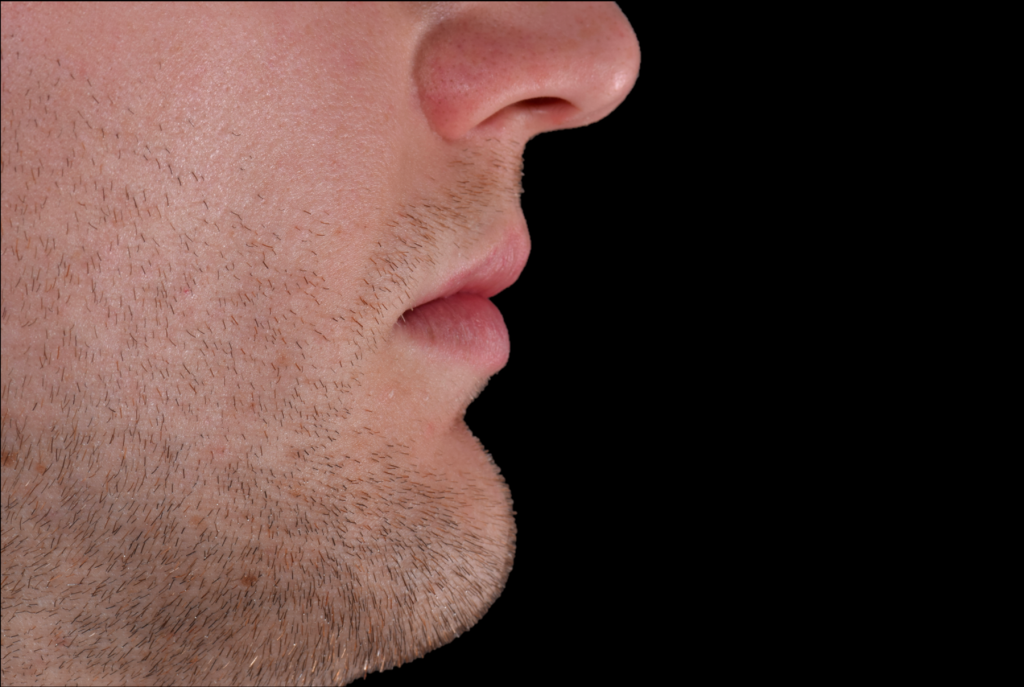
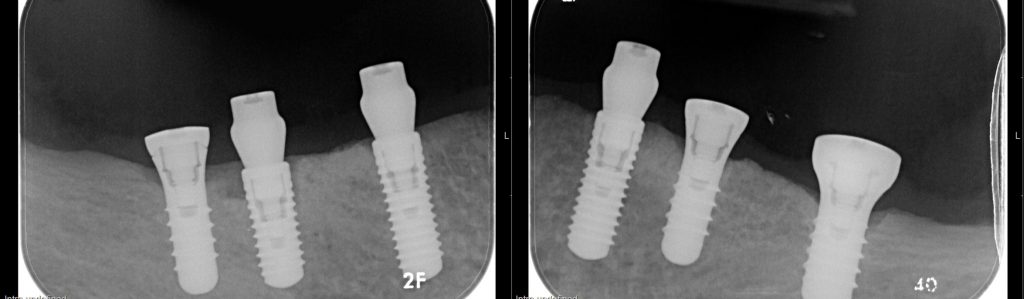
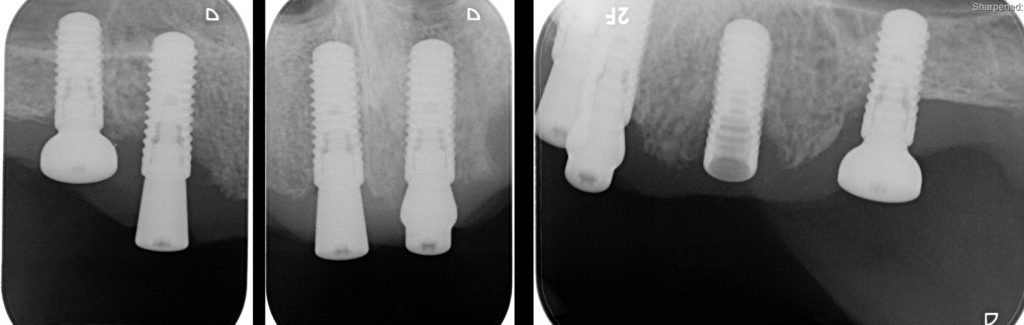
The iliac crest grafts can resorb unpredictably (Donos et al.,, 2008) and this, together with the suboptimal position of several maxillary implants made treatment challenging (Buser et al.,, 2004). The need for facial support necessitated the choice of a removable prosthesis for the maxilla (Fig. 2.2). The UL3 implant was removed due to its position (Fig. 3). The UR3 implant was left in situ and covered with a healing abutment in line with the patient’s wish for the least intervention possible and based on the fact that it would not alter the treatment plan. Non-surgical peri-implant treatment was performed, and although the UL5 had distal bone loss, peri-implant tissue stability was achieved (Berglundh et al., 2017).

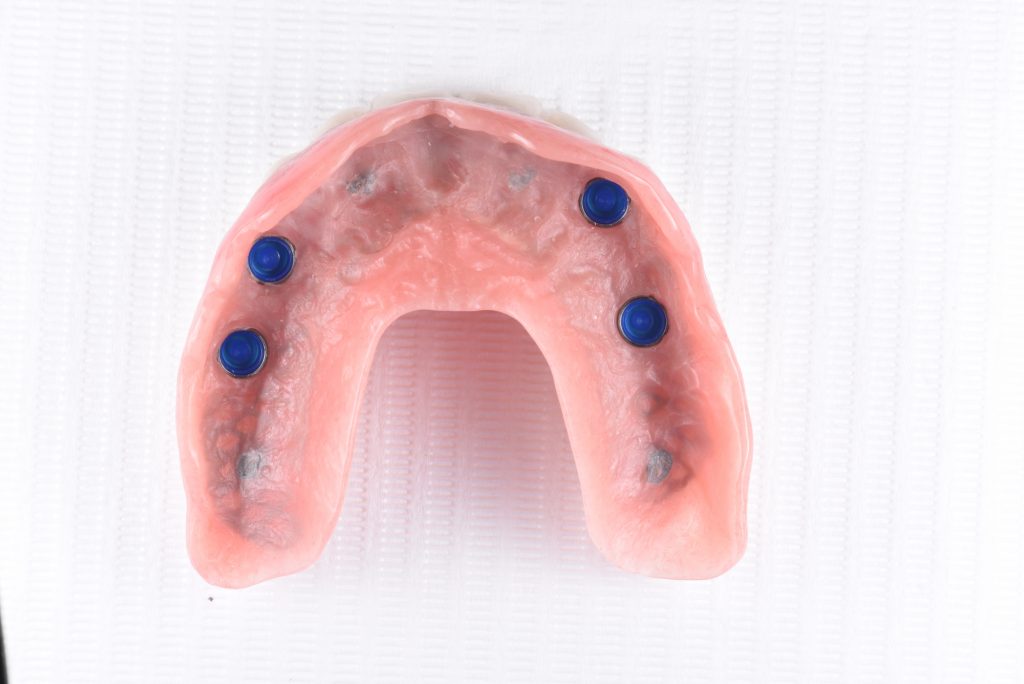
Implant-level impressions were made for the maxilla and the mandible (Fig. 4.1), after which an assessment of the prosthetic space and the implant angulation could be made, based on the ideal tooth position (Fig. 4.2).



Based on the prosthetic space, free-standing attachments for the maxillary overdenture were chosen. The suboptimal implant position meant that 15-degree angulated free-standing attachments (Novaloc®) would have to be used for three of the implants in order to achieve a relatively parallel insertion path. Trial abutments can be used intraorally or on the cast so the correct height and angulation can be chosen prior to ordering the final Novaloc abutments.




Following the choice of the appropriate free-standing abutments, they were torqued to the implants and their position could be picked up (Fig. 5.1-5.4). At this stage, a maxillary acrylic base plate with the final tooth set-up and adequate space for the forming matrices were used. A medium-body silicone wash impression was done with a closed mouth technique against the mandibular tooth try-in (Fig. 5.5).





The final prostheses were delivered, restoring the patient’s vertical dimension of occlusion and facial support (Fig. 6.1-6.4).