Introduction
Dental implants have emerged as the primary solution for replacing teeth with an unfavorable prognosis. However, this treatment is not immune to complications (Pjetursson et al. 2012).
The two main complications encountered are mechanical and biological. Mechanical complications, though typically manageable, can present challenges such as screw deformation/fracture or implant fracture (Fig. 1). On the other hand, biological complications notably peri-implant diseases like mucositis and periimplantitis , pose a more significant threat by inducing resorptive inflammatory processes that compromise the surrounding alveolar bone (Fig. 2). While these diseases exhibit a high prevalence, a standardized long – term curative protocol remains elusive (Rodrigo et al. 2018; Derks & Tomasi 2015). The ITI Treatment Guide 13 emphasizes prevention as the clinician’s paramount objective. Depending on the severity of the disease, surgical or non-surgical therapies are performed to reduce inflammation and prevent implant loss.

Fig. 1: Abutment screw fracture as a mechanical complication. 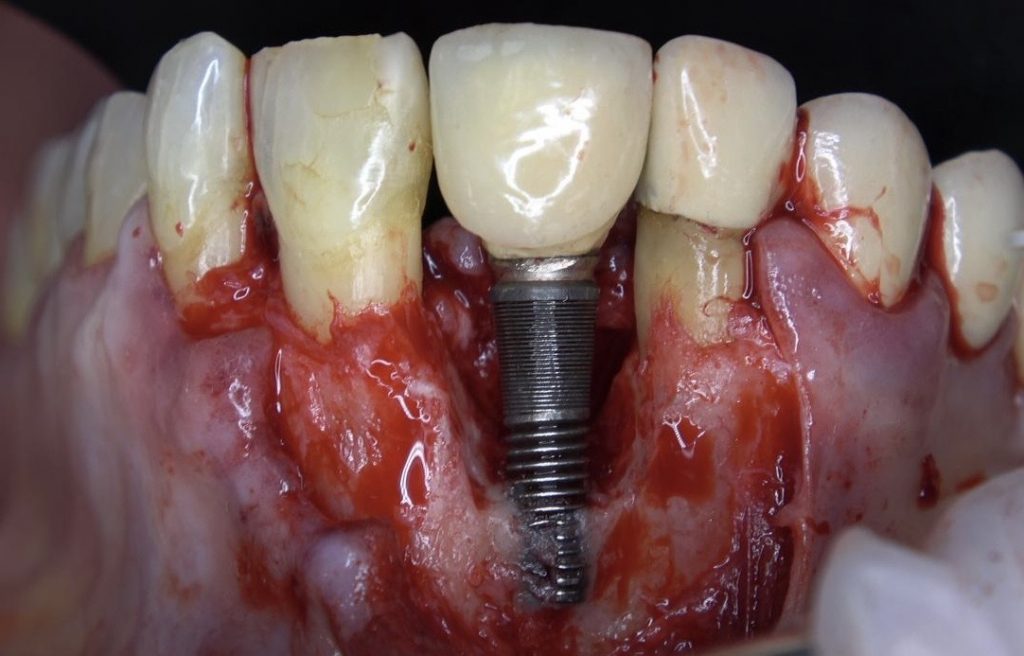
Fig. 2: Biological complications: Peri-implantitis and bone loss.
Correct treatment planning and adequate prosthetic design allowing plaque control are vital towards preventing peri-implant diseases. Emerging evidence indicates a strong relationship between prosthetic design and peri implant tissue health. Although there are indeed patients who are susceptible to peri-implant diseases, the prosthetic design and patient instruction with adequate hygiene guidelines may contain inflammation and avoid progressive bone loss.
An adequate three-dimensional position of the implant and soft and hard tissue stability are all key factors that make the prosthetist´s job infinitely easier, having a better scenario to obtain long term success of the treatment. An incorrect implant 3D position, excessive torque at implant placement and a lack of hard and soft tissues are reported as precipitating factors to early bone loss.
Digital planning
Improved knowledge and advances in dental technology have improved the clinician´s implant planning capacity. The prosthetic and esthetic results are displayed digitally to plan the implant position using the information provided by cone beam computed tomography (CBCT) and the diagnostic wax-up. Digital planning can be very helpful in determining the prosthetic material based on the prosthetic space, prosthetic modality, abutment selection, and surgical approach. Once the clinician has gone through this process as well as a facial analysis, an ideal prosthesis for the patient may be chosen with precision.
A recent paper described a digital workflow for terminal dentition patients. The protocol includes a 3D digital smile design and chairside mock-up restoration that enable a prosthetically driven assessment before implant treatment planning and 3D printing of surgical templates. This can predictably reduce chairside time and adjustments at the surgical and fixed provisionalization appointment (Papaspyridakos et al. 2022) (Fig. 3,4,5 & 6).
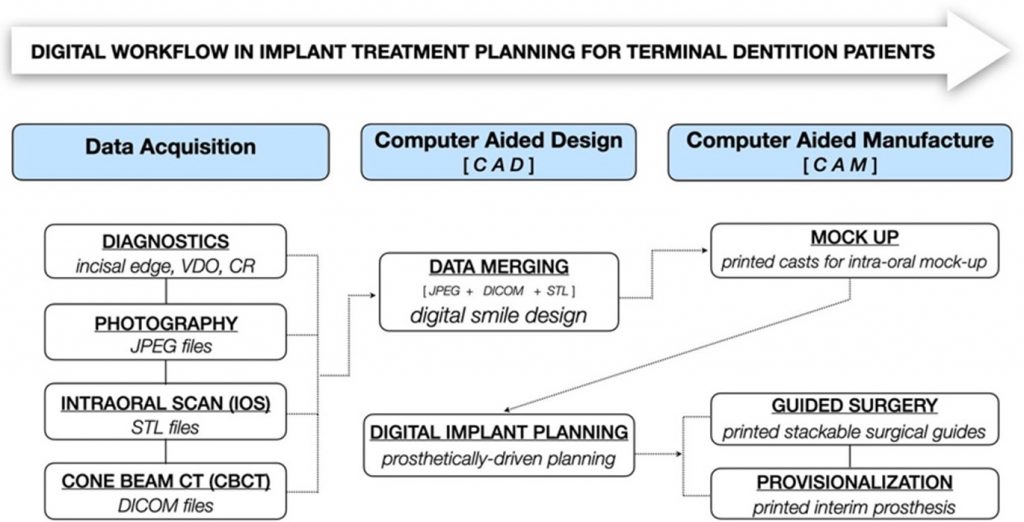
Fig. 3: Digital workflow for terminal dentition 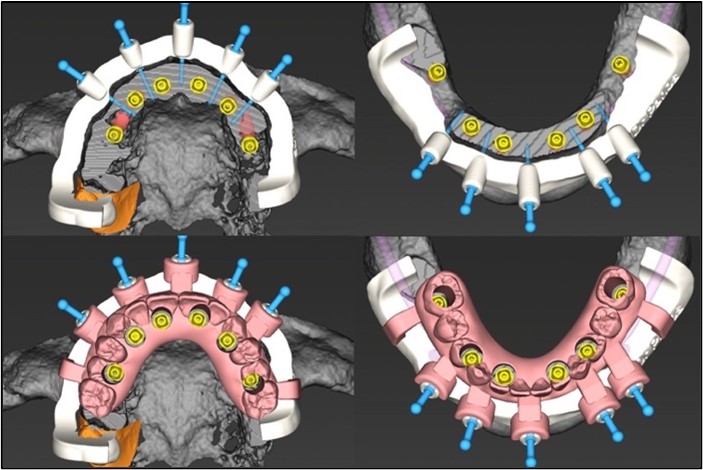
Fig. 4: Digital workflow for terminal dentition 
Fig. 5: Digital workflow for terminal dentition 
Fig. 6: Digital workflow for terminal dentition
Prosthetic Designs
Implant choice
Internal-hex implants have become the gold standard as external-hex implants have demonstrated excessive bone remodeling which is a risk factor for peri-implant diseases (Zipprich et al. 2007).
Most contemporary internal-hex implant designs can be divided into two groups: tissue-level and bone-level implants.
Although both tissue-level and bone-level implants appear to be suitable for the rehabilitation of edentulous arches, tissue-level implants showed a greater risk of implant collar exposure (Menini et al. 2022).
Conical and platform switched connections have reported good stability, better mechanical properties and a reduced pumping effect of bacteria.
Cement retained versus screw retained implant supported prosthesis
- Screw-retained restorations
Screw-retained restorations are considered to be the gold standard, since they allow the prosthesis to be removed which is a great advantage, considering the high prevalence rates of peri-implant disease that were previously mentioned (Rodrigo et al. 2018; Derks & Tomasi 2015). Whenever possible, screw-retained prostheses should be applied. If the screw access represents more than 40% of the occlusal area, cemented restorations should be considered to prevent mechanical complications. - Cement retained restorations
Cement-retained restorations have excellent mechanical properties and have been widely used in cases where the angulation of the implants is unfavorable, making the screw-retained option difficult. Among the disadvantages, is that not only can the prosthesis not be removed by the clinician when required, but there is also a risk of excess cement remnants that are challenging to identify. (Wilson et al). The complications derived from this approach occur as a result of incorrect cementing technique not from the approach itself. On a prospective study performed by Wilson et al the relation between excess cement and peri-implantitis was analyzed and the results obtained were that subgingival cement migration was the cause of peri-implantitis in 85% of the implants. - Screw-cement retained prosthesis
Also known as the hybrid abutment technique. This trend has developed widely over recent years and presents the advantages of both techniques. It is cemented on a Ti-base abutment that never enters an oven, so it does not change dimensionally, thus avoiding lack of fit or gaps. This approach combines the biomechanical advantages of both the cemented and screwed technique. Cementation can be carried out extra or intraorally, with the possibility to remove the crown and polish it, making this a safer procedure.
This restorative approach gained popularity after wear problems were observed in cases of zirconia directly connected to implants. In these cases, the implants released titanium particles that could lead to peri-implant diseases due to the body’s inability to absorb them (Suárez-López del Amo et al). This technique has great prosthetic versatility, as it is compatible with a wide range of restorative materials and the new Ti-base designs have different angulations and heights (Fig. 7).

Fig. 7: Variobase for screw-cemented technique (hybrid abutment crown)
Choice of Abutments
Abutments are a significant aspect of the prosthesis design as they influence how the occlusal forces are transferred and therefore, in the mechanical stability.
The direct-to-implant approach may be reasonable for single-implant crowns. However, in cases where multiple implants are present and with different angulations, it is difficult to achieve passive fit if an implant level impression was taken. For this reason, multiunit abutments should be used in such cases providing a passive fit prosthesis even with significant divergence of placed implant axes. The use of multiunit abutments not only ensures a secure fit for the prosthesis but also addresses concerns about soft tissue integrity, a critical factor in maintaining bone levels around the implant. In traditional implant protocols, frequent unscrewing of healing or temporary abutments can disrupt the biological width of the soft tissue, leading to a weakening of the hemidesmosomal attachment around the implant. This repeated disruption can result in a less robust and narrower soft tissue connection, potentially contributing to bone resorption, particularly in patients with thin mucosa biotypes. By minimizing the need for such manipulations below the bone level, multiunit abutments help preserve the integrity of the soft tissues and promote a healthier, more stable peri-implant environment.
The most widely used recourse for multiple implants is multi-unit abutments, which provide different benefits. At a biomechanical level, it is easier to achieve passive fit. At a biological level, when multi-unit abutments are used in a bone-level implant, it becomes a tissue-level design. In a 1-year randomized clinical trial Blanco et al demonstrated that almost no initial bone loss occured when multi units with a height of more than 2mm were used.
Inadequate subcrestal implant placement can lead to bone resorption. When implants are placed deeper than 6 mm without an intermediate abutment the risk of peri-implant inflammation increases exponentially.
Zirconia abutments have demonstrated less bacterial adhesion when compared to titanium abutments in a recent in vitro study (Ozer et al. 2022)
Implant Supported Temporary Prosthesis
During the healing stage, the implant supported provisional prosthesis plays a crucial role in achieving both esthetic and functional outcomes while also modeling the tissues to create an optimal environment for the final prosthesis. Recent trends emphasize the importance of provisional prosthetic designs closely resembling the definitive rehabilitation to minimize tissue disturbance due to constant variations.
A well-designed provisional prosthesis offers a good opportunity to assess the patient’s ability to maintain oral hygiene, especially if there are changes in the restorative profile =. A poorly fitting provisional, that does not adequately seal the surgical area or is insufficiently polished can lead to adverse effects such as bone resorption. bone resorption. If the implant suffers an initial bone loss above 0.5mm before the final prosthesis stage, the risk of peri-implantitis increases (Galindo-Moreno et al. 2022). For this reason, current provisional prostheses are based on critical and subcritical contour principles. In the subcritical zone the aim is to provide space for the soft tissues to obtain the greatest possible volume to seal the entire area. However, a convex design must be conferred to the critical zone to provide tissue support (Su et al. 2010).
The stackable guides concept can be very useful to obtain tissue stability from the start of the treatment. Surgeries are planned with multiple guides to generate the least possible trauma to the tissues and guide healing with a provisional prosthesis. Not only do patients go through less invasive surgeries and obtain adequate esthetic results but also multiple adjustments between the provisional phase and the final restoration are avoided. Furthermore, the provisional prosthesis is placed precisely based on the planning (Norré & Att 2022) (Fig. 8,9,10 and 11).
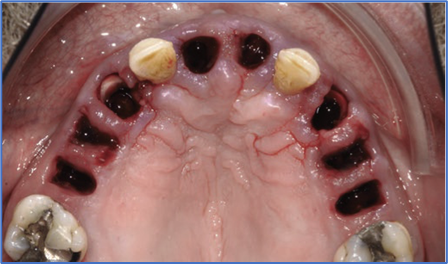
Fig. 8: Stackable guide protocol 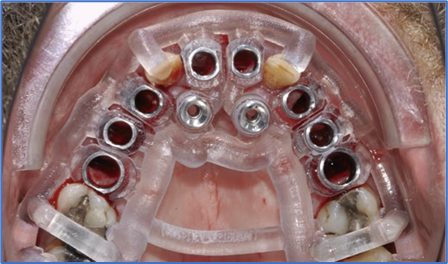
Fig. 9: Stackable guide protocol 
Fig. 10: Stackable guide protocol 
Fig. 11: Stackable guide protocol
Definitive Prosthesis
It is necessary to carry out an adequate planning when deciding on the appropriate material, not only based on the needs of the patient (age, occlusal pattern, esthetic requirements…) but also, on the interocclusal space that the patient presents.
Materials
The selection of the restorative material is a key point for long-term success. In recent years, alternatives to the classic metal-ceramic and metal-acrylic materials have been developed, to avoid complications such as plaque accumulation and fractures. Zirconia has emerged and gone through a great evolution. Although monolithic zirconia was initially not very esthetic, its properties were improved following the high rate of fractures that occurred when placing ceramic veneers. Currently monolithic multilayered zirconia has been developed, presenting higher translucency.
Regardless of its esthetic characteristics, it has been demonstrated to have a biocompatibility far superior to any material used before, even achieving fibroblast attachment (Linkevicius & Vaitelis 2015). Ultra-polished zirconia leads to less plaque accumulation when compared to polished zirconia (Valantijiene et al. 2023).
In a multicenter study of 337 implants with a follow-up of up to 12 years, the implant survival was over 98% and no zirconia fractures were experienced demonstrating that it can be a reliable restorative material despite its lack of flexibility when adequate planning is done.
Other materials are proving to be suitable as an alternative to classic materials. The mechanical properties of reinforced polymers are being enhanced their mechanical properties and, given their low weight and biocompatibility, they could be an interesting alternative, but clinical studies are required. PMMA has become an essential tool for clinicians when making provisional prostheses. The mechanical properties of this material have improved, especially when they are monolithical and milled. In the author’s experience, PMMA can be used as a definitive restorative material, however, a correct selection of the patient and technique are vital for treatment success. In a recent study the feasibility of using PMMA as a definitive prosthetic material to restore completely edentulous patients was analyzed with no mechanical or esthetic complications after two years. Patients should be warned that when certain wear limits are reached, the prosthesis must be removed to mill a new one. It is necessary to carry out long-term research to determine its capacity as a definitive material.
Single Implant Supported Restorations
The design of single implant crowns must always be concave, and the emergence profile must never exceed 30 degrees. Emergence profiles above 30 degrees with convex contours increase the risk of recession by almost 40% and of peri-implantitis in bone level implants. Above 40 degrees bone loss happens during the first year after prosthesis placement (Siegenthaler et al. 2022) (Fig 12).
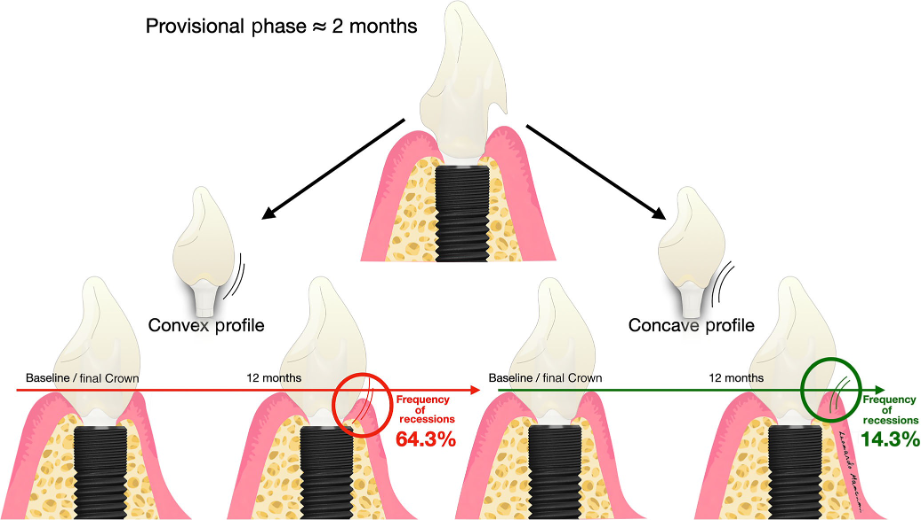
Fig. 12: Recession frequency depending on crown profile design (Siegenthaler et al 2022)
Implant Bridges
In implant bridges, hygienic designs that allow for correct plaque control must be installed. The clinician must take into account that whenever there is an implant next to a natural tooth, the contact areas tend to open over time. This situation, which can create inflammation in the peri-implant tissues due to food accumulation, can lead to the appearance of subgingival caries in the medium/long term. It is very important that radiographic examinations are done during maintenance appointments to control these complications.
Full Arch
Dividing implant restorations into sections rather than opting for a single-piece bridge is highly recommended from a clinical standpoint. This approach offers significant advantages, particularly in managing peri-implant inflammation and implant loss scenarios. By employing sectional designs, the necessity to remove the entire prosthesis is obviated in cases where localized issue arise.This approach also ensures that in the event of implant loss, the entire structure need not be sacrificed , thereby preserving functional integrity.
In mandibular cases, this sectional design is even more critical due to mandibular flexion, which is often responsible for unwanted bone loss in distal full arch rehabilitations.
Compensation for skeletal discrepancies in fixed implant rehabilitations may also lead to large bucco-lingual prosthesis widths with extensive horizontal tissue contours that enables patients to achieve hygiene in certain areas (Yi et al. 2020).
Vestibular flanks that may compromise the patient’s ability to carry out cleaning should be avoided. Plaque accumulation occurs in poorly contoured prostheses, which is why the basal areas of the prostheses must always be expulsive, with a convex contour and made of highly biocompatible materials (Fig. 13).

Fig. 13: Full arch prosthesis
Tips
The clinician should always use original screws and abutments to achieve a perfect fit. Non-original screws may have a compatible, but not a perfect fit, and this gap may induce bacterial accumulation. Non-original screws have demonstrated a higher rate of loosening after cyclic loading. In addition, the metal alloys normally used are very rigid, increasing fracture risk (Alonso-Pérez et al).
Occlusal instability and lack of passivity of the structures are factors that can cause bone resorption, which can evolve to peri-implantitis over the long term. Cantilevers and high stress areas are unfavorable towards obtaining successful long-lasting implant treatments. Passivity should always be tested, a verification jig must be used when bridges and full arch structures are designed. CAD-CAM techniques have improved during the last decade and currently we can obtain a digitally designed milled verification jig with high accuracy (Sinada et al). Milled bars used as an infrastructure under the prosthetic material can be a wise strategy to avoid direct stress to the implants, improve the distribution of occlusal forces and obtain a passive fit (Fig 14).
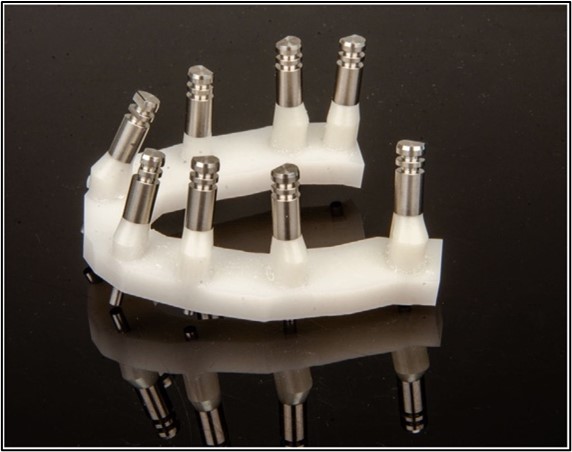
Fig. 14: Milled Verification Jig
Once the prosthesis is delivered and the occlusion has been checked, hygiene guidelines should be given so patients understand the importance of biofilm removal, and adequate plaque control. If the patient progresses adequately, they will be told how often their maintenance protocol should be performed.
Discussion
In a recent study by Tapia et al 48 patients were treated. The selection criteria were unfavorable prosthetic designs that made biofilm removal complicated. In a first session all of the patients underwent periodontal treatment and were stabilized. The control group, 24 of these patients, received no further treatment. While the test group received hygiene instructions and the prostheses were adapted so that correct plaque control could be achieved. After 6 months almost every patient in the control group presented inflammation and pathological probing, while almost the entire test group was stable.
This paper demonstrates that if adequate hygiene instructions had been given and the prosthetic design had been correct patients would have been able to carry out good dental hygiene from the initial phase of the treatment, preventing peri-implant inflammation.
Conclusion
Most of the complications which are faced in the dental office are a consequence of inappropriate planning. To avoid most of the complications derived from an incorrect prosthetic design, it is recommended to take these factors into consideration.






