Introduction
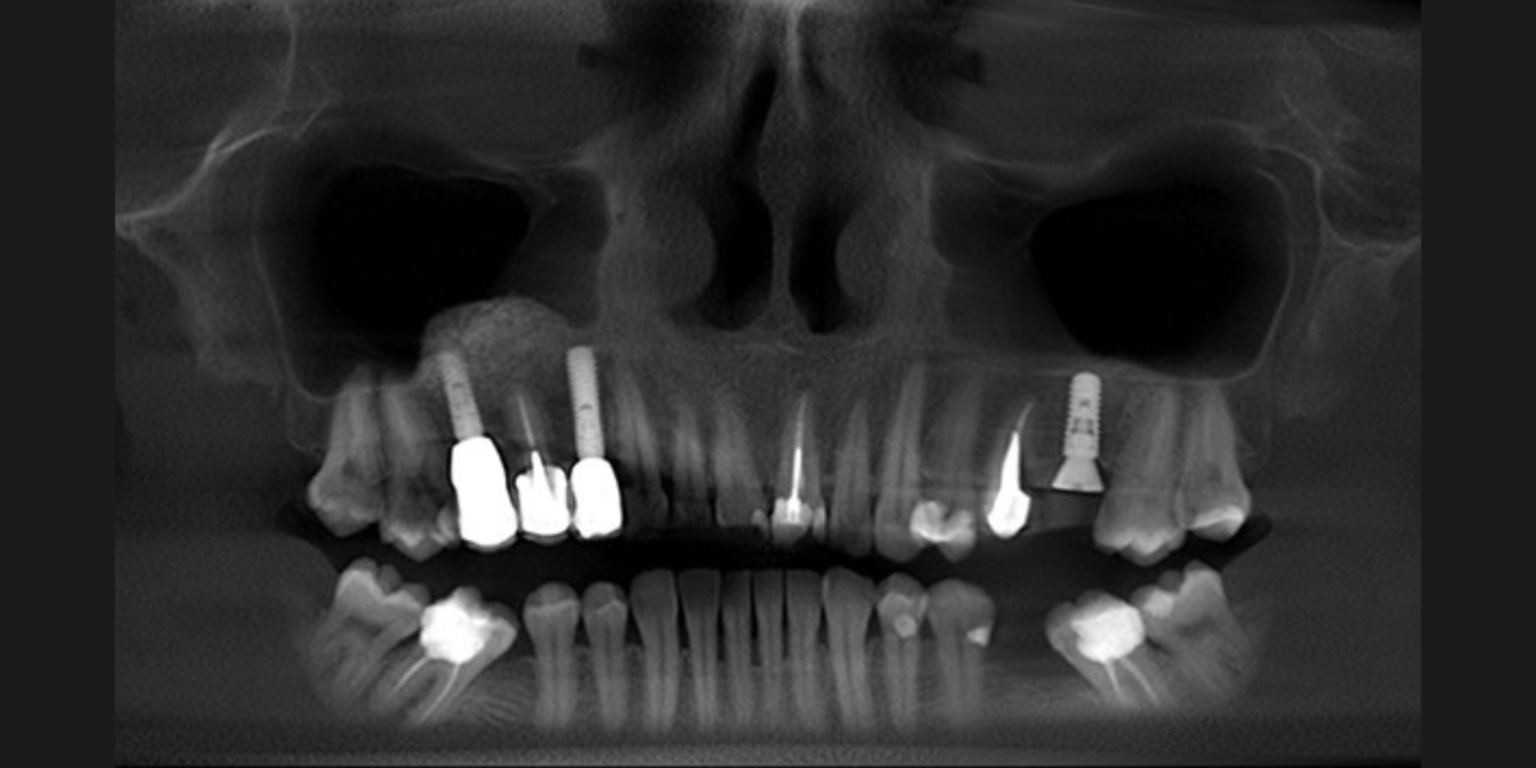
Partial edentulism of the distal molars is a prevalent and critical clinical condition that often requires dental implant treatment. Ensuring precise implant placement in posterior regions is crucial to avoid significant complications. Incorrect implant placement in these areas can lead to problems such as damage or perforation of critical anatomical structures like the maxillary sinus and the inferior alveolar canal. These complications can result in issues such as compromised osseointegration, peri-implantitis, esthetic concerns, and an elevated risk of long-term failures. Several studies have highlighted the importance of accurate placement to mitigate these risks (Do et al., 2020; Ribas et al., 2020). The introduction of static guided implant surgery (sGIS) has proven to be beneficial in facilitating and optimizing implant planning and positioning, especially in cases where anatomical structures are adjacent (Jorba-García et al., 2021; Mistry et al., 2021).
Through sGIS, the optimal selection and positioning of implants can now be digitally designed by integrating cone-beam data and intra-oral or dental cast scan data. This virtual planning process allows for the precise transfer of implant positions intraoperatively using a surgical guide. Surgical guides utilized in computer-assisted implant surgery are classified based on their supporting structure and tailored to specific clinical needs. Tooth-supported templates are relatively rigid and are favored for their precision in guiding dental implant placement (Ku et al., 2022; Putra et al., 2022; Vercruyssen et al., 2015).
However, in cases of partial tooth loss, particularly in distal free-end situations where neighboring teeth are absent, the stability of the surgical guide may be compromised. This lack of distal support can result in issues like bending or tilting, primarily affecting the distal portion of the guide and consequently impacting implant placement accuracy. In vitro studies assessing the impact of surgical guide support and implant positioning in partially edentulous typodonts revealed that the number and location of supporting teeth, along with the presence of distal extensions, significantly influence surgical accuracy (El Kholy et al., 2019; Wu et al., 2022). Additionally, guided implant placement demonstrates greater precision in bounded edentulous spaces, with angular deviations as low as 1.36° ± 0.41°, while free-end situations show increased deviations, ranging from 2.00° ± 0.68° for single-tooth spaces to 2.71° ± 1.20° for three-tooth spans, emphasizing the importance of guide stabilization in such cases (Ganzman, 2022).
In pursuit of improving the accuracy of static sGIS in distal extension scenarios, researchers have explored various practical approaches. Recent studies have primarily focused on investigating factors associated with surgical guide parameters, including their extension, type of support, design, fixation, and fabrication methods. By closely examining these elements, researchers aim to elucidate their influence on the precision of dental implant placement in free-end situations when utilizing surgical guides (Putra et al., 2022). The findings derived from current research will provide dental practitioners with valuable insights, enabling them to implement sGIS more effectively within the appropriate parameters. Additionally, this knowledge will aid in selecting optimal planning strategies to achieve enhanced accuracy in dental implant procedures.
Extension of the surgical guide/number of implants
In addressing the impact of surgical guide parameters, particularly guide extension, on accuracy in partial distal edentulism, a significant finding emerges: an increase in the span of the free-end edentulous space for additional planned implants (≥2) substantially decreases the accuracy of placement. This pivotal observation underscores the importance of carefully considering the extent of the edentulous space when evaluating cases for sGIS.
Bounded edentulous spaces generally exhibit higher accuracy compared to unbounded free-end edentulous spaces. However, this difference was not statistically significant in cases of single-tooth distal edentulism as it was with two-teeth and three-teeth unbounded distal edentulous spaces. Consequently, greater challenges are anticipated in cases of two- or three-teeth distal edentulism, where angular deviations are more pronounced, leading to reduced precision in implant placement.
The solution lies in good case selection, knowing that one-tooth partial edentulous spaces demonstrate higher trueness and precision in implant placement, which is not significantly different from that of bounded edentulous spaces. This indicates a closer adherence to planned positions, suggesting that careful consideration of the specific anatomical characteristics of the edentulous space can mitigate challenges associated with free-end situations (Ganzman, 2022; Megaly et al., 2024).
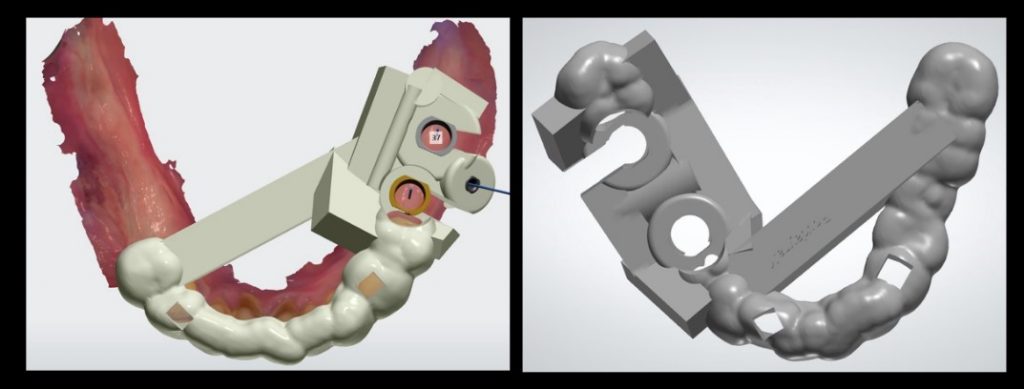
Support and design of the surgical guide
When comparing precision between distal extension scenarios and a single tooth gap using tooth-supported guides, a notable challenge arises: significant deviation is observed among implant sites in the bucco-lingual direction at the implant platform, particularly accentuated in the distal extension position. This discrepancy underscores the challenge posed by the lack of distal guide support.
In cases of partial distal edentulism, surgical guides often rely solely on tooth support, which can lead to discrepancies in implant placement due to distal forces that dislodge the sleeve during the osteotomy and implant placement. Incorporating additional support, such as mucosa or bone support, has been shown to significantly enhance the accuracy of static guided implant surgery (sGIS), especially in unbounded posterior edentulous sites. Research suggests that utilizing a posterior rest on attached keratinized soft tissues for mucosa support provides improved stability, though this approach requires a minimum of 3 mm of attached keratinized soft tissue mucosa in the posterior areas to avoid challenges from mobile alveolar mucosa. Alternatively, adding a bone-supported strut to the distal part of the surgical guide or employing a combination tooth-and-bone supported guide has demonstrated comparable accuracy to bilaterally tooth-supported guides, making these strategies promising solutions for distal extension scenarios involving missing mandibular molars (Azevedo et al., 2024; Lin et al., 2020).
However, these tooth-and-bone supported guides necessitate the opening of a full-thickness flap, thereby diminishing one of the advantages of performing sGIS surgery with a flapless approach. Another challenge emerges when placing the second distal implant via the same surgical guide. A notably larger bucco-lingual deviation at the implant platform is observed compared to the first distal implant. Remarkably, most bucco-lingual deviations of the second distal implant tend toward the lingual side, indicating a left-sided bending of the surgical guide during simulation surgery conducted by right-handed surgeons. Interestingly, depth deviations of the distal extension situation sites do not significantly differ from bilaterally tooth-supported sites (El Kholy et al., 2019; Lin et al., 2020; Song et al., 2024).
Fixation of the surgical guide
When addressing guide fixation, the primary challenge lies in ensuring stability during implant surgery. Surgical guides used without fixation pins often result in implants following the path of least resistance within the bone, leading to deviations from the intended guide orientation.
Recent research aiming to assess the accuracy of sGIS in implant placement, specifically focused on tooth-supported free-end cases. These studies examined cases involving the placement of three implants in the distal edentulous region of the maxilla using either solely tooth-supported guides or guides supplemented with three additional fixation pins. Statistical analysis highlighted a significant discrepancy in implant position accuracy, particularly concerning horizontal apical and depth deviations, when fixation pins were not used in the procedure. Notably, implants positioned in distal extensions showed greater improvement with the use of fixation pins, likely due to their proximity to adjacent teeth. Hence, adding fixation pins to the surgical guide during implant surgery in partially edentulous patients may minimize movement, thereby offering a potential solution and enhancing procedural precision. However, this additional step introduces potential challenges. In cases where the surgical template is not fully seated, deviations may accumulate, ultimately impacting the final implant position. Furthermore, employing fixation pins away from the edentulous site may increase procedural invasiveness, necessitating anesthesia of additional areas, drilling through alveolar mucosa, and posing a risk of proximity to vital anatomical structures.
Another in vitro study proposed a possible solution to enhance surgical guide stability during implant placement in sGIS by employing posterior anchor micro screws. These micro screws were suggested to increase guide stability by reducing mobility during seating and the drilling process. Unlike previous fixation pin systems, the anchor cap was connected to the micro screw, providing both fixation and retrievability of the guide template.
However, implementing this technique clinically presents challenges, including patient acceptance, increased surgical costs, and greater invasiveness. Additionally, inserting micro screws requires an additional minor surgical procedure and subsequent removal under local anesthesia, further complicating the process.
Despite these challenges, both fixation pins and anchor micro screws offer potential solutions to enhance the stability of implant guide templates in sGIS procedures. However, careful consideration of the associated complexities and challenges in their implementation is essential (Chen et al., 2023; Chrabieh et al., 2024; Mai and Lee, 2020; Pessoa et al., 2022).
Fabrication of the surgical guide
In vitro studies investigating the factors influencing the accuracy of surgical implant guides in free-end situations have identified several key variables. One challenge arises in cases involving milled guides, where accuracy is primarily determined by the position of the tooth. Notably, implants replacing second molars exhibit stronger deviations compared to those replacing first molars. Conversely, in scenarios utilizing printed guides, multiple factors come into play. Alongside tooth position, sleeve height and supporting length also significantly impact accuracy. One solution to enhance accuracy in printed guides is the optimization of sleeve height and extending tooth support. Specifically, smaller sleeve heights and extended tooth support are associated with improved accuracy in implant placement. Overall, milled guides demonstrate superior accuracy in free-end situations lacking distal tooth support compared to 3D-printed guides. These findings underscore the importance of considering various factors, including manufacturing methods and guide design, to optimize the precision of implant placement in such scenarios (Kessler et al., 2021).
Conclusions
Implant placement in partial distal edentulism cases is challenging to avoid complications such as damage to anatomical structures and long-term implant failures. sGIS has proven potential in optimizing implant positioning, but its accuracy can be compromised in free-end situations due to the lack of distal support. Overall, improving the accuracy of sGIS in partial distal edentulism involves a multi-faceted approach, integrating optimal guide design, support, and fixation techniques alongside careful case selection to ensure precise implant placement and minimize complications.