Introduction
Peri-implantitis is a widely prevalent condition. The complexity of its treatment, as well as the increased likelihood of recurrence, are challenging. Therefore, preventive measures and early diagnosis are fundamental in implant care, which includes managing risk indicators and factors. This review explores systemic factors associated with peri-implantitis development, focusing on smoking, hyperglycemia, and a history of periodontitis. Evidence from cohort studies indicates that smoking significantly increases the incidence of peri-implantitis, highlighting the dentist’s role in patient education and smoking cessation guidance. Evidence on the influence of hyperglycemia on increased risk of peri-implantitis from retrospective, cross-sectional, and cohort studies suggests an association between the two. While more consistent evidence from cohort studies is needed to establish hyperglycemia as a clear risk factor, the available evidence underscores its relevance as a risk indicator. Thus, dentists play an essential role in informing patients and collaborating with physicians in patient care. A history of periodontitis has also been associated with an increased risk of peri-implantitis, with conflicting evidence necessitating further investigation through cohort studies. Dentists must prioritize effective periodontitis management and control, particularly in patients with existing implants or needing implant procedures.
Why are preventive measures critically important in the realm of peri-implantitis?
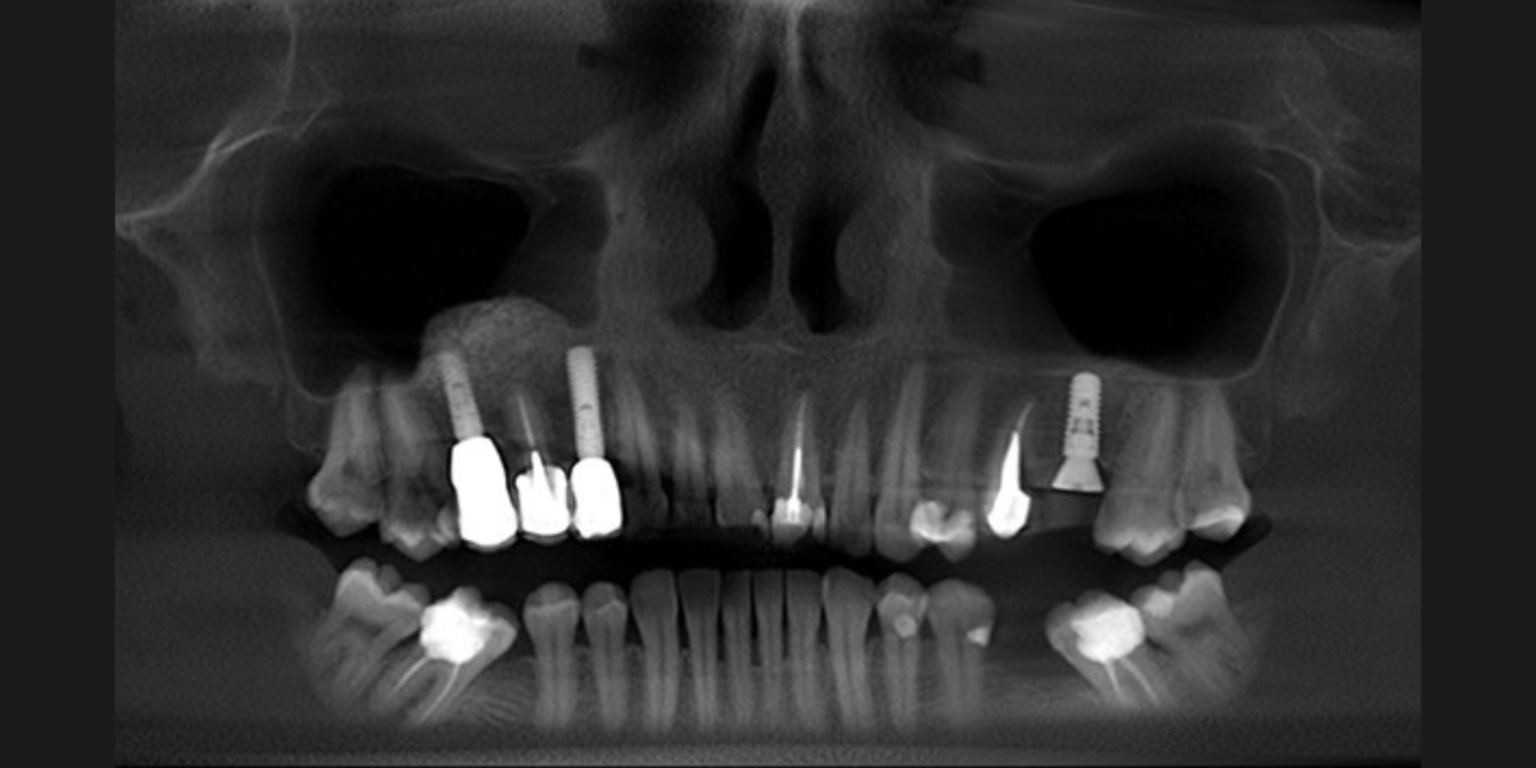
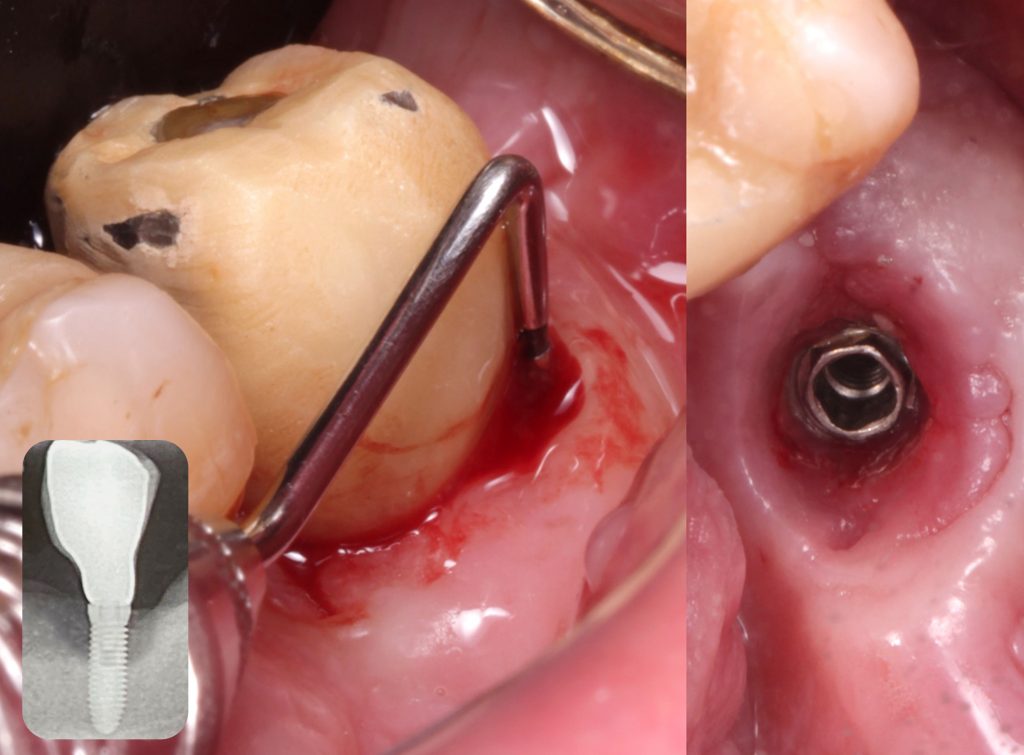
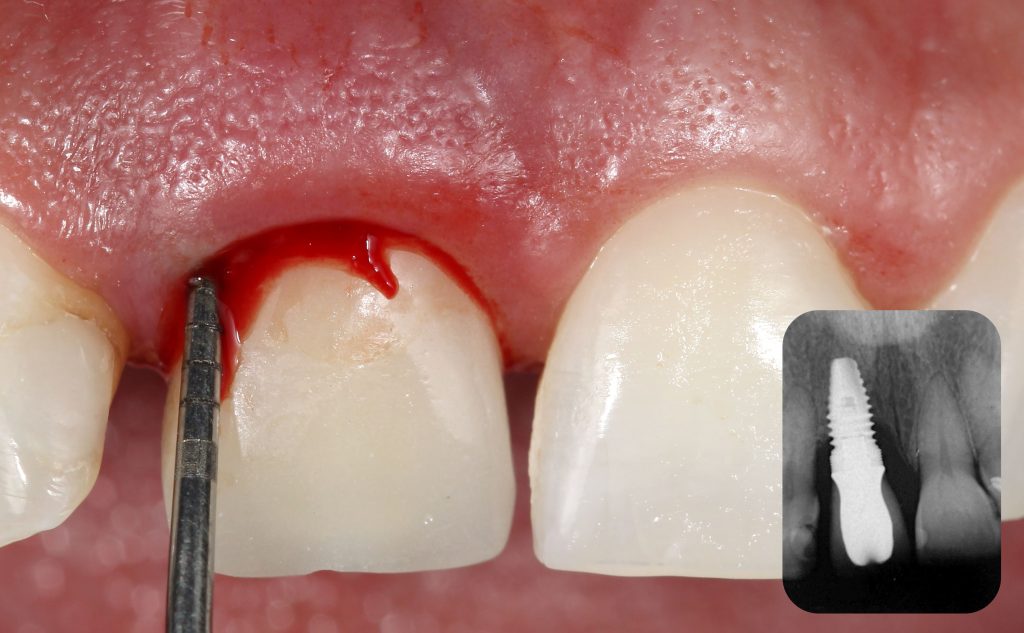
Peri-implantitis is a disease associated with biofilm accumulation, characterized by inflammation in the peri-implant mucosa and loss of supporting bone (Berglundh et al., 2018). Its prevalence is estimated to be 22% (ranging from 1% to 47%) (Derks & Tomasi, 2015). The onset of peri-implantitis often occurs early, typically within three years of function, and its progression follows a non-linear and accelerating pattern (Derks et al., 2016).
Despite its prevalent occurrence, peri-implantitis poses a challenge due to the complex nature of therapeutic interventions and the sometimes limited effectiveness of its treatment (Heitz-Mayfield & Mombelli, 2014). Moreover, systematic reviews have brought attention to high recurrence rates following treatment of peri-implantitis. Investigations spanning three years of follow-up have shown recurrence rates of up to 69.9% for treated implants (Stiesch et al., 2023) and 100% in cases with follow-ups extending beyond one year (Esposito et al., 2012).
In this context, early diagnosis and prevention must be considered crucial aspects of implant dentistry. A preventive strategy involves managing both local and systemic risk factors to prevent the development or progression of peri-implantitis (Herrera et al., 2023; Jepsen et al., 2015; ITI Treatment Guide Volume 13).
Cumulative evidence has shown the association of certain factors with an increased risk of peri-implantitis (Darby, 2022). This article aims to provide evidence-based insights into the systemic factors associated with the development of peri-implantitis.
What defines a risk indicator and a risk factor for a disease?
A risk factor is any attribute, characteristic, or exposure of an individual that increases the likelihood of developing a disease. Risk factors are validated through a temporal sequence, often identified in cohort studies. Conversely, reducing or eliminating these factors often leads to a decreased risk of disease onset or progression (Beck, 1998).
Interventional longitudinal or cohort studies are needed to identify true risk factors for disease, while cross-sectional or retrospective studies may only highlight risk indicators (Schwarz et al., 2018). Causality in humans can be shown through randomized controlled trials, providing balance over potential prognostic factors between experimental and control groups via random assignment (Beck, 1998; Hill, 1949; Lilienfeld & Stolley, 1994). However, it is important to clarify that ethical and risk/benefit considerations restrict human experimentation. For example, it is unethical to assign people randomly to smoking and non-smoking groups to study disease development. Subjecting a patient to harm for the purpose of gathering evidence is not ethically defensible. For this reason, human experimental evidence is frequently unavailable to ascertain whether a factor causes disease. Interventional studies typically aim to demonstrate whether an intervention reduces disease incidence rather than increases disease occurrence rates (Beck, 1998; Hill, 1949; Lilienfeld & Stolley, 1994). Consequently, assessing the risk for disease is frequently conducted through prospective observational studies, such as cohort studies.
In the 2017 World Workshop for the classification of peri-implant diseases, potential risk factors and indicators for peri-implantitis were discussed. Among systemic risk factors and indicators, conditions such as smoking, diabetes, a history of periodontitis, genetic factors, cardiovascular disease, rheumatoid arthritis, osteoporosis, osteopenia, thyroid disease, hepatitis, body mass index, radiation, and chemotherapy were mentioned. However, smoking, diabetes, and a history of periodontitis were highlighted as having more robust evidence (Schwarz et al. 2018). The present article offers an updated perspective, focusing particularly on smoking, diabetes, and a history of periodontitis, which have more substantial evidence, incorporating new insights that have emerged.
Smoking
Despite worldwide health authorities’ extensive efforts to reduce smoking, the global number of smokers has actually increased (GBD Tobacco Collaborators et al., 2019). This implies that the number of smokers in dental offices is still rising. Additionally, new forms of smoking are emerging and being adopted by the population. Substantial evidence supports smoking as a significant risk factor for periodontitis and periodontitis-associated tooth loss (Carvalho et al., 2021; Leite et al., 2019).
Moreover, smoking significantly affects the peri-implant environment in several ways. It shifts the microbiome towards a state associated with disease (Pimentel et al., 2018; Tsigarida et al., 2015), induces vasoconstriction of gingival blood vessels, and hampers leukocyte function, increasing susceptibility to infection (Archana et al., 2015). Additionally, smoking disrupts the gene expression profile of mesenchymal stem cells, resulting in decreased osteogenic markers and an increase in pro-inflammatory genes, compromising bone metabolism (Cyprus et al., 2018). The inhalation of carbon monoxide diminishes hemoglobin’s oxygen-carrying capacity, potentially impeding healing and overall tissue health (Javed et al., 2019). Importantly, smoking triggers a cascade of systemic and local processes adversely affecting osteogenesis, bone metabolism, and the integrity of the bone-implant interface (Bezerra Ferreira et al., 2016; Pereira et al., 2010; Sayardoust et al., 2017).
Regarding the impact of smoking on the incidence of peri-implantitis, a recent systematic review and meta-analysis by Reis et al. revealed a significant increase in peri-implantitis rates among smokers (Reis et al., 2023). Compared to non-smokers, smokers faced twice the risk of developing peri-implantitis at the implant (RR: 2.04, 95% CI: 1.46–1.85) and at the patient level (RR: 2.08, 95% CI: 1.17–3.71). Importantly, this systematic review relied exclusively on cohort studies, allowing for the assessment of peri-implantitis development from the time of implant placement until the follow-up. The certainty of evidence, evaluated through the GRADE approach, was moderate for both patient and implant-level analyses, indicating a strong likelihood that the observed effects in the meta-analyses closely reflect the true impact (Reis et al., 2023).
The findings of this review contrast with those of previous reviews. Notably, this is the first to include only prospective cohort studies, while others encompassed cross-sectional and retrospective studies (Dreyer et al., 2018; Sgolastra et al., 2015; Turri et al., 2016).
The elevated risk of peri-implantitis in smokers (Reis et al., 2023) highlights the important role of dental professionals in informing patients with planned or existing dental implants about this relevant association. Additionally, it emphasizes the importance of providing guidance to encourage smoking cessation, thereby preventing possible biological complications.
Building on this discussion, it is important to note that the definition of a smoker can vary. However, even in studies where patients smoked fewer than 10 cigarettes daily, a notable incidence of peri-implantitis was observed in smokers. Therefore, it is advisable to use the Center for Disease Control and Prevention’s (CDC) definition of a smoker. According to this definition, current smokers are adults who have smoked 100 cigarettes in their lifetime and currently smoke every day or some days (CDC, 2017).
Diabetes/Hyperglycemia
An estimated 451 million people worldwide, aged 18-99 years, were living with diabetes in 2017. Projections indicate a substantial increase, with the global diabetic population expected to grow by approximately 242 million from 2017 to 2045. As a result, the projected total is set to reach 693 million by 2045 (Cho et al., 2018).
Epidemiological findings demonstrate a higher prevalence and severity of periodontitis in individuals with poorly controlled diabetes mellitus in contrast to healthy individuals. This link has prompted the consideration of periodontitis as a diabetes-associated complication, often referred to as “the sixth complication in diabetic patients” (Löe, 1993; Nibali et al., 2022).
Some mechanisms may explain the detrimental effects of hyperglycemia and diabetes on peri-implant tissues. Hyperglycemia induces hyper-inflammatory responses, resulting in increased tissue damage. Elevated blood glucose levels generate advanced glycation end products (AGEs). These AGEs activate the expression of receptors for AGEs (RAGEs), further impairing the repair of periodontal tissues. This impairment is exacerbated by the sustained inflammation induced by the bacterial biofilm (Lalla & Papapanou, 2011).
A systematic review and meta-analysis (Monje et al., 2017) investigated the potential association of diabetes and hyperglycemia with peri-implantitis. Seven studies had undergone quantitative analysis and the resulting meta-analyses indicated that the risk of peri-implantitis is roughly 50% higher in individuals with poorly controlled diabetes compared to those without diabetes (RR = 1.46; 95% CI: 1.21–1.77 and OR = 1.89; 95% CI: 1.31–2.46; z = 5.98; p < .001). Notably, among non-smokers, those with diabetes and hyperglycemia exhibited a 3.39-fold higher risk of peri-implantitis compared to those with normoglycemia (95% CI: 1.06–10.81). This systematic review suggests an association between diabetes mellitus/hyperglycemia and an increased risk of peri-implantitis, independently of smoking. In addition, the results suggest that the higher the glycemic level (i.e. poor glycemic control such as HbA1c >8%) at baseline, the greater prevalence of peri-implantitis (Monje et al., 2017). However, the review included retrospective, cross-sectional, and cohort studies and only two studies in the meta-analyses had a prospective design.
While valuable insights emerge, it is essential to acknowledge that including retrospective and cross-sectional studies precludes establishing a causal relationship due to the absence of a clear temporal connection. Despite the limitations, the findings of this review suggest an association between hyperglycemia and an increased risk of peri-implantitis.
In this context, dentists engaged in implant procedures should educate patients about the potential connection between poorly controlled diabetes and peri-implantitis. Furthermore, for individuals with poorly controlled diabetes, implant placement is associated with an unpredictable prognosis, delayed osseointegration, and a higher risk of failure (Tan et al. 2021). Open communication between dentists and physicians is crucial to ensure comprehensive care, considering diabetes management at every stage, from implant planning to maintenance. It is recommended to maintain an HbA1c level of <7.0–8.0% for diabetes control, depending on the patient’s systemic condition (Nathan et al. 2008).

History of periodontitis
A systematic review estimated the global prevalence of severe periodontitis in 2010 to have reached 10.8% (95% confidence interval: 10.1–11.6%). This condition affected 743 million people worldwide, ranking it as the sixth most widespread health issue (Kassebaum et al., 2014). Periodontitis is one of the main causes of tooth loss (Al-Shammari et al., 2005; Carvalho et al., 2021), indicating that a significant proportion of patients opting for dental implant placement after tooth loss will have a history of periodontitis.
A systematic review and meta-analysis analyzed the association between a history of periodontitis and peri-implantitis. Five studies were part of the meta-analysis, indicating that periodontally compromised patients had an increased risk of peri-implantitis compared to those without a history of periodontitis (RR: 2.21, 95% CI: 1.42–3.43, P=0.0004), with moderate but not significant heterogeneity (P=0.12;I2=46%). However, it is noteworthy that only one of the studies included in this analysis was prospective, while the others adopted a cross-sectional design (Sgolastra et al., 2015a).
A 10-year prospective study found a 6% peri-implantitis incidence (defined as PD ≥ 5 mm, BOP+, and annual bone loss >0.2 mm) in the non-periodontitis group at implant level, contrasting with a 29% incidence in individuals exhibiting a history of periodontitis (Karoussis et al., 2003). Costa et al. reported significantly higher odds of developing peri-implantitis in individuals with periodontitis (OR 9). During the investigated 5-year follow-up, 21 out of 27 patients with peri-implantitis had developed the condition. Six out of 7 in the group participating in regular maintenance appointments and 15 of 18 in the group enrolled in a regular maintenance program (Costa et al., 2012). Furthermore, a recent prospective study with a 20-year follow-up reported a significantly increased risk of peri-implantitis in patients with a history of periodontitis (40.3%) compared to periodontally healthy patients (13.6%) (p=0.025) (Roccuzzo et al. 2023). These cohort studies build upon previous follow-ups by Roccuzzo et al. (2010, 2012) that were included in the 2017 World Workshop review by Schwarz et al. This concluded that there is strong evidence supporting a history of periodontitis as a risk factor/indicator for peri-implantitis.
More recently, a systematic review and meta-analysis examined the influence of periodontitis on peri-implantitis development and found contrasting results (Ferreira et al., 2018). The review showed an association between the presence or history of periodontitis and peri-implantitis based on implant and patient-based data, with a 2.15 higher chance of developing peri-implantitis (95% CI: 1.10; 3.21). Nevertheless, this association was not replicated in the meta-analysis of cohort studies (N = 5) for patient-based or implant-based data (Ferreira et al., 2018). Additionally, more recently, a systematic review focusing solely on cohort studies (N = 5) found that the incidence of peri-implantitis was 4.09 times higher (95% CI: 1.93–8.58) in periodontally compromised patients compared to periodontally healthy patients at the implant level, with a follow-up period ranging from 5 to 20 years (Serroni et al., 2024).
However, the variability in diagnostic criteria for periodontitis and peri-implantitis in terms of defining form, severity, and extent complicated accurate evaluation in both reviews, hindering comparisons between studies. Moreover, different approaches to assessing periodontitis history may have introduced biases, potentially favoring patients with an “active” periodontitis history over those undergoing regular periodontal maintenance therapy. Studies comparing patients with a history of periodontitis to those with “active” disease are needed to discern potential disparities. Given the limited inclusion of only two cohort studies, caution is advised in interpreting the results until additional cohort studies are conducted.
While additional cohort studies are necessary for further validation, the current focus should remain on proactive treatment and control of periodontitis to reduce the risk of peri-implantitis. Given that the history of periodontitis is an immutable aspect in patients, the primary focus for dentists should always be the effective management and control of the disease. It is imperative to prioritize periodontal health in patients with an ongoing disease or with a history of periodontitis, not only during the maintenance phase but even more so before implant placement.
Conclusion
In conclusion, prevention, and management of peri-implantitis should address the control of its risk indicators/factors, such as smoking, hyperglycemia, and history of periodontitis. The ongoing challenge of peri-implantitis, coupled with its high prevalence and recurrence rates, reinforces the need for continuous research on its risk factors, as well as updated strategies in both prevention and treatment to ensure peri-implant health.