Introduction
Digital imaging systems and computer-aided design and computer-aided manufacturing (CAD-CAM) techniques are powerful resources capable of simplifying the diagnosis, treatment planning, and execution of surgical procedures (Wismeijer et al., 2018). By virtue of these technologies, occlusally-compromised and esthetically demanding clinical scenarios have been managed predictably with custom-made surgical templates, pre-surgical diagnostic casts, and treatment prostheses designed to simplify the visualization of the projected prosthetic outcome, in addition to serving as an aid during implant placement. (Azpiazu-Flores et al., 2022; Azpiazu-Flores et al., 2023; Chackartchi et al., 2022). Consequently, when combined with thorough treatment planning, most patients treated with these techniques usually report favorable post-surgical outcomes such as improved satisfaction, decreased pain, and uneventful recovery. (Youk et al., 2014)
This brief clinical report presents the rehabilitation of a partially edentulous female treated with a Straumann SLActive Bone Level Tapered dental implant. The diagnostic stage, planning, and implant placement surgery were aided by contemporary digital imaging techniques, 3D modeling, advanced implant planning, and digital light processing (DLP) 3-dimensional (3D) printing. Implementing these techniques allowed the definition of the most prosthetically favorable implant position, permitted selection of the best implant design for the clinical scenario, and facilitated ordering of all the components involved in the surgical procedure, saving laboratory and chairside time.
Clinical report
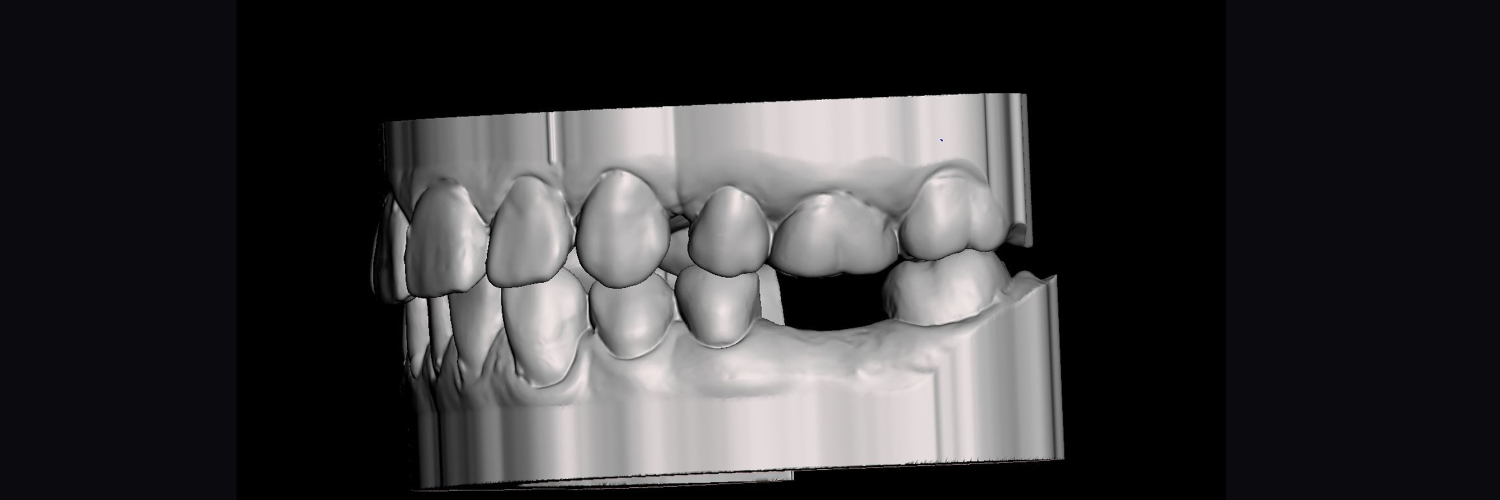
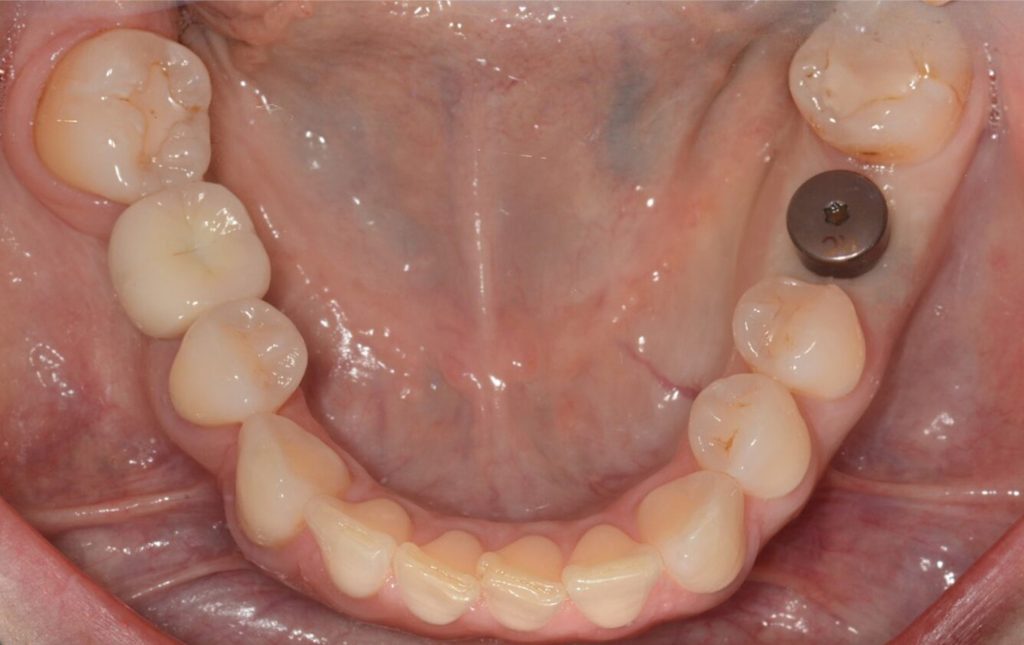
A 41-year-old female presented to the Center for Implant, Esthetic and Innovative Dentistry at Indiana University School of Dentistry. Her medical history was uneventful and her left mandibular first molar had been extracted one year before. The maxillary and mandibular teeth appeared structurally and periodontally stable, and the tissues of the edentulous area appeared healthy (Figure 1). At the end of the appointment, maxillary and mandibular diagnostic intraoral scans were completed, and the maximal intercuspal position (MIP) was recorded digitally with an intraoral scanner (Trios 4 Wireless; Straumann Digital Solutions, 3Shape) (Figure 2). A cone beam computerized tomography (CBCT) scan was also performed for diagnostic and planning purposes.

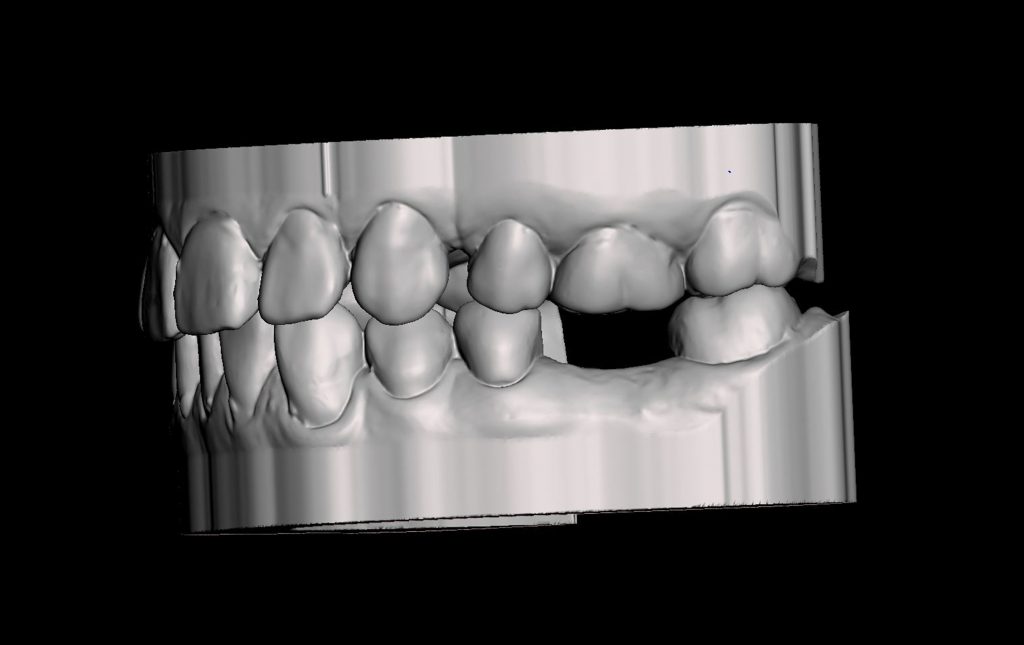
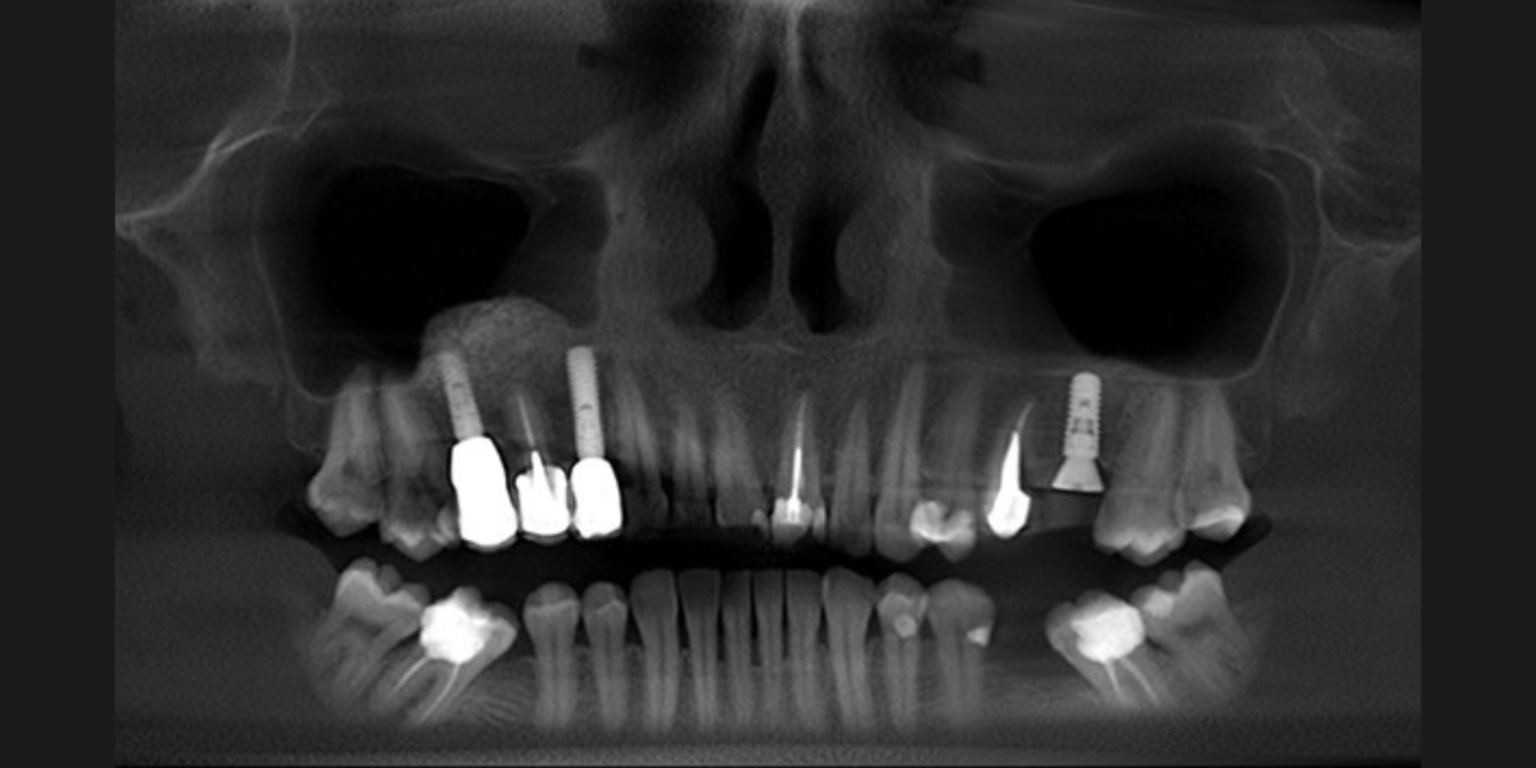
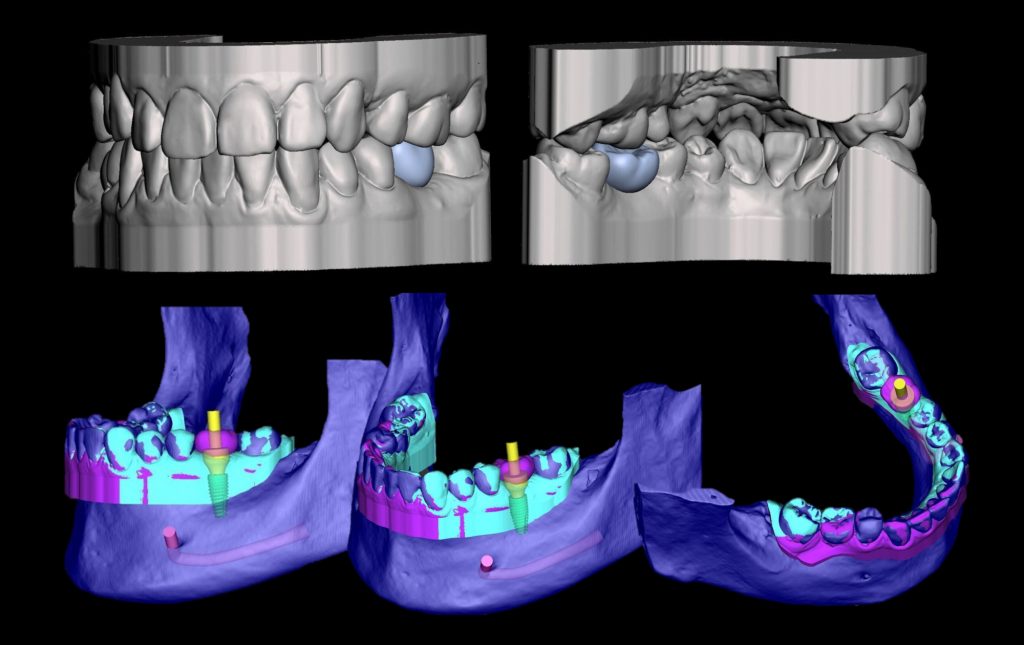
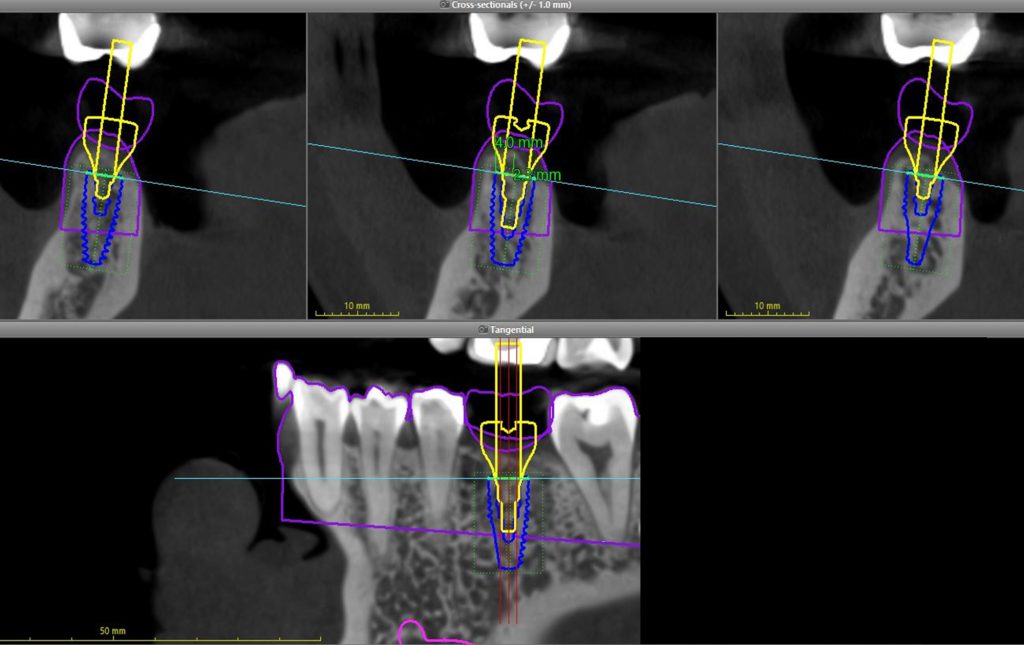
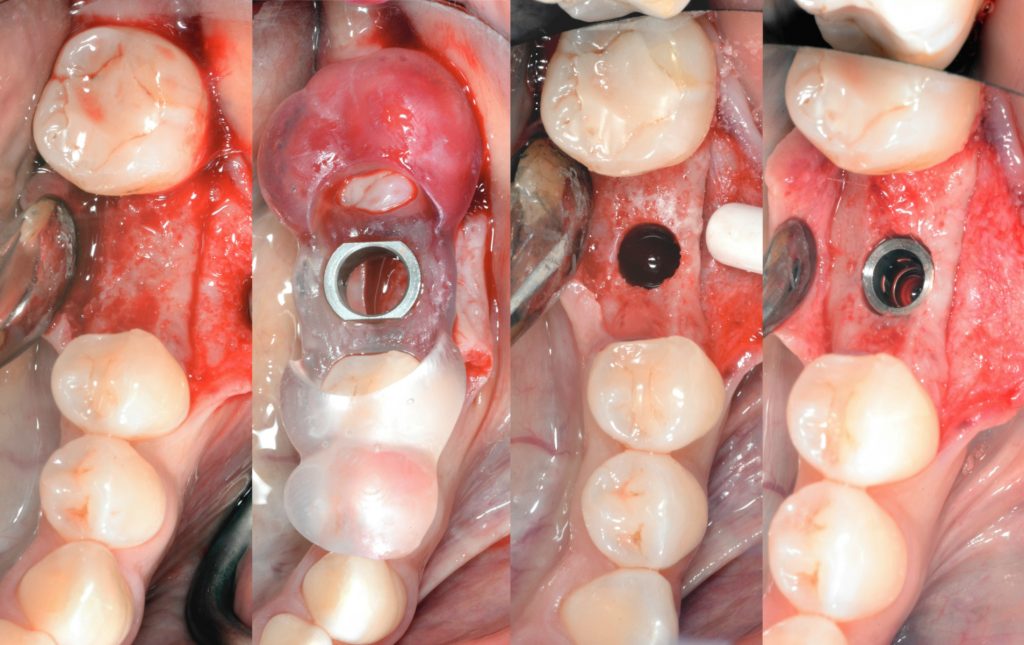
Subsequently, the maxillary and mandibular digital casts were imported into a free 3D modeling computer program (Meshmixer; AutoCAD), and a digital diagnostic wax-up for the edentulous site was completed. After designing the desired prosthetic contours digitally, the initial diagnostic scan and digital diagnostic wax-up casts were aligned with the patient’s CBCT data in a professional implant planning computer software (CoDiagnostiX; Straumann, Dental Wings). After evaluating the relationship of the underlying osseous structures with the overlying soft tissue and desired prosthetic contours, a Regular CrossFit (RC) ø 4.8 ×10-mm bone-level implant with SLActive surface was deemed a favorable implant design (Figures 3 and 4). A computer-generated surgical template was generated using the same implant planning software to facilitate implant placement in the prosthetically desired position. Subsequently, the template was manufactured in a professional DLP 3D printer (P30+; Straumann, RapidShape) using a biocompatible photopolymerizable resin (P Pro Surgical Guide Resin; Straumann Detax). After fabrication, the 3D-printed surgical template was cleaned and post-polymerized according to the manufacturer’s recommendations.
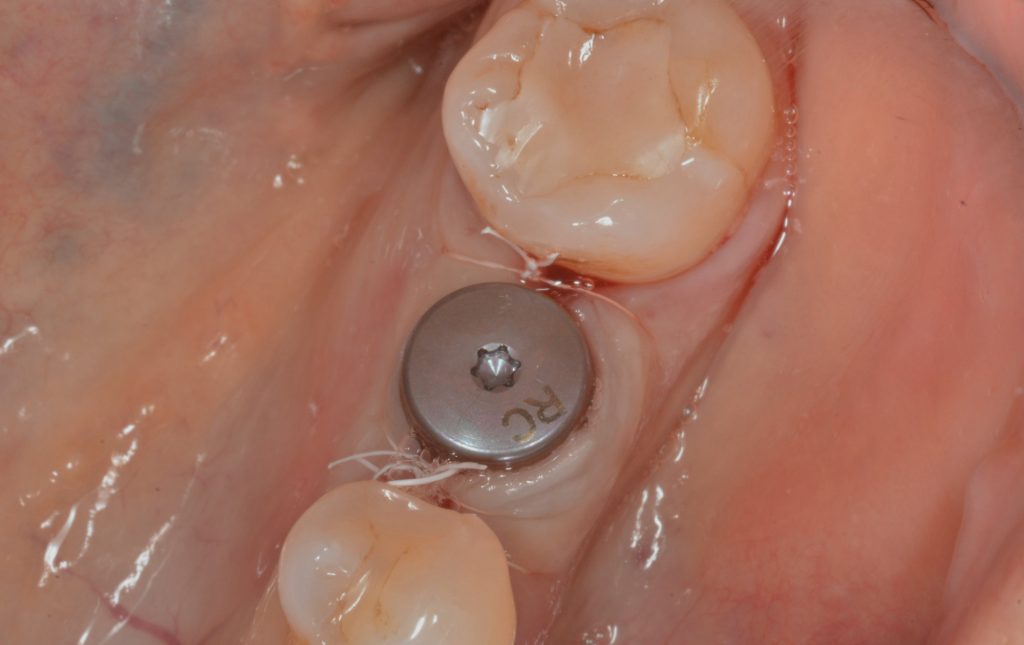
For implant placement, a crestal incision was made and a full thickness mucoperiosteal flap was elevated to expose the underlying alveolar bone. After the alveolar bone had been exposed, the implant bed was prepared using the guided surgery protocol generated by the implant planning software, and the dental implant was uneventfully inserted into the prepared osteotomy achieving an insertion torque of 40 Ncm (Figure 5). Additionally, the initial stability quotient of the dental implant was measured by means of resonance frequency analysis. The bucco-lingual and mesiodistal measurements recorded were >80 (Ostell Beacon; Ostell, W&H) (Figure 6). Finally, a ø 6.5×6-mm long RC healing abutment was inserted and hand-tightened, and polytetrafluoroethylene (PTFE) (Cytoplast PTFE Sutures; BioHorizons ltd) single interrupted sutures were placed on the mesial and distal interdental gingival papillae (Figure 7).

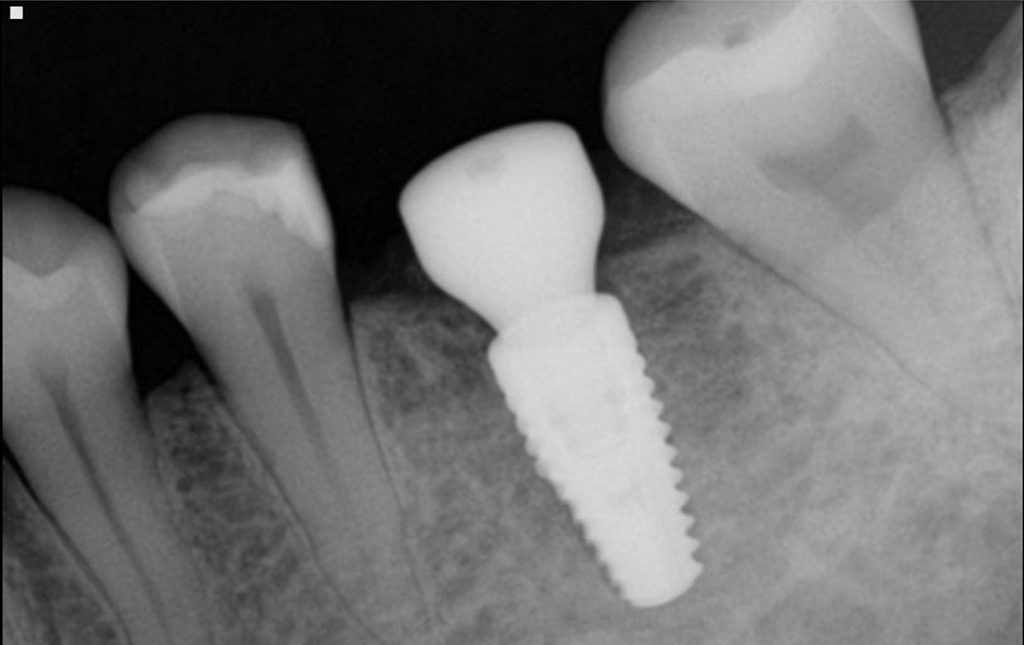
Two weeks post-insertion, the PTFE sutures were uneventfully removed, and the patient was instructed to return in 6 weeks to start the prosthetic phase of the treatment. At the 2-month appointment, the peri-implant tissues were evaluated and deemed clinically healthy; additionally, no mobility or signs of infection were noted, and the osseous structures around the dental implant appeared to be stable radiographically (Figures 8 and 9).
Discussion
The clinical and planning time for dental implants can be reduced significantly without compromising the accuracy of the surgical procedure using digital planning and computer-aided manufacturing technologies. The present clinical report demonstrates the implementation of contemporary imaging technologies and CAD-CAM techniques to simplify the placement of a dental implant for a female patient seeking a prosthetic replacement for her missing mandibular first molar.
Research advocates that patients treated with dental implants placed using computer-generated surgical templates experience a smoother surgical procedure with improved satisfaction; furthermore, clinicians have reported the application of these technologies to be an attractive tool capable of enhancing accuracy and safety compared to free-hand dental implant placement. (Vercruyssen et al., 2014; Youk et al., 2014). For those reasons, contemporary dental implant planning protocols were used on this patient. The clinical diagnostic data were merged with the CBCT data to evaluate the relationship of the digitally designed diagnostic wax-up with the underlying soft tissue, osseous structures, and adjacent teeth. Visualizing the volumetric and spatial relationships of the dental implant with these important anatomical structures ensured a true prosthetically-driven implant placement, a prerequisite for a long-lasting and biomechanically stable implant-supported prosthesis.
Despite the significant advantages regarding ease of visualization and simplified planning provided by digital implant planning and CAD-CAM technologies, research suggests the accuracy of guided implant surgery is influenced by several intrinsic and extrinsic factors related to the data acquisition and manufacture of the surgical template. Factors such as the data acquisition techniques, the manufacturing trinomial (Anadioti et al., 2022), the extent of human error during planning, and inadvertent movements of the template during surgery can affect the accuracy of the dental implant placement. (Chackartchi et al., 2022) In the present clinical report, a tooth-supported surgical template was fabricated using DLP 3D printing. Research suggests that tooth-supported surgical templates facilitate accurate implant placement, superior or equal to bone-supported or mucosa-supported surgical templates. (Tahmaseb et al., 2014). Furthermore, contemporary DLP technologies permit the creation of clinically satisfactory surgical templates, equal or superior to other 3D printing techniques. (Le et al., 2023) Therefore, whenever favorable intraoral situations are present, only minor discrepancies should be expected between the planned and the final implant position, specifically when preceded by thorough presurgical planning combined with CAD-CAM techniques.
It is important to note that the current clinical report presents only one clinical scenario of a single implant placement. Therefore, the good clinical results in this case cannot be generalized to all clinical scenarios, such as those involving multiple missing teeth or completely edentulous patients. The authors also acknowledge that the implant planning computer program and manufacturing technologies presented involve a significant financial investment, and therefore, not all dental offices may have the equipment needed to execute the digital workflow presented. However, some of the elements outlined in this report, including the careful assessment of the prosthetic space available, the depth of the implant placement, and the relationship of the projected implant placement with critical anatomical structures and the adjacent teeth, constitute traditional prosthetic and biological principles that still can be achieved by using traditional analog workflows or some parts of the digital workflow presented here.
Conclusion
Using digital imaging methods alongside CAD-CAM technologies significantly empowers clinicians engaged in dental implant placement and restoration. By combining crucial diagnostic information, these techniques enable the precise determination of optimal implant positions tailored to individual patients. This process potentially streamlines planning and surgical procedures while improving the patient’s response to dental implant therapy.