Introduction
Tooth extraction is a common procedure in daily dental practice with an impact on the quality of life of our patients, indicated for strategic reasons or when the teeth cannot be maintained in a status compatible with health, function, or esthetics (Kao 2008). The local trauma of a tooth extraction causes a local physiologic disruption resulting in an initial inflammatory response, inevitably leading to a variable degree of alveolar ridge atrophy. Several preclinical and clinical studies have demonstrated that the peak of alveolar ridge remodeling after tooth extraction occurs during the first few weeks. However, a process of progressive disuse atrophy may continue over time (Araujo & Lindhe 2005; Chappuis et al. 2013; Chappuis et al. 2015; Couso-Queiruga et al. 2023)
A recent systematic review and meta-analysis evaluating the dimensional changes after tooth extraction in adult human subjects observed that ridge resorption is more pronounced in the horizontal dimension, followed by vertical mid-facial and mid-lingual changes. Facial bone thickness upon extraction was strongly related to the extent and magnitude of alveolar bone resorption, and non-molar sites were associated with an increased need for ancillary bone grafting procedures before or at the time of implant placement compared with molar sites (Couso-Queiruga et al. 2021). Also, as reported in a clinical study where minimally traumatic extraction measures were taken, 28% of the extraction sites presented some degree of buccal bone dehiscence, and 4% exhibited complete buccal bone loss (Leblebicioglu et al. 2015). Moreover, different patterns, severity, and extent of residual alveolar bone after tooth extraction can be encountered.
Several interceptive therapies have been proposed to attenuate these resorptive events. These include orthodontic forced eruption (Cordaro et al. 2021; González-Martín O et al 2020), alveolar ridge preservation procedures with or without immediate implant placement (Cordaro et al. 2021; Avila-Ortiz G et al. 2019; Avila-Ortiz et al.2020; Clementini et al. 2019; Saito et al. 2021; Spinato et al. 2014; Couso-Queiruga et al. 2023) and partial extraction protocols (Hürzeler et al. 2010; Gluckman et al. 2016; Salama et al. 2007). Other therapeutic options to treat alveolar ridge deficiencies may include bone and/or soft tissue augmentation procedures. However, these approaches have been associated with a variable degree of predictability and success (Abrams 1980; Aghaloo & Moy 2007; Antonious et al. 2021; Kuchler & von Arx 2014; Seibert et al. 1996), increase in treatment cost, intra- or postoperative complications, and time. Hence, whether the treatment plan for tooth replacement includes a removable, fixed, implant, or tooth-supported prosthesis, alveolar ridge reduction may result in a significant clinical challenge. Thus, it seems evident that an adequate assessment and effective management of the extraction site should be a core component of contemporary dental practice since it could contribute to preserving the architecture of the alveolar ridge and attenuating post-extraction dimensional changes (Couso-Queiruga et al. 2023). This is particularly critical in the anterior esthetic zone when tooth replacement via implant therapy is planned (Abrams 1980; Aghaloo & Moy 2007; Antonious et al. 2021; Kuchler & von Arx 2014; Seibert et al. 1996). Therefore, this ITI blog article aims to present a minimally invasive ridge reconstruction therapy for the management of post-extraction dehiscence defects, demonstrating the use of a particulate bone grafting material and a non-resorbable dense polytetrafluoroethylene (dPTFE) membrane immediately after tooth extraction.
Background
This technique has been evaluated by our group (Antonious et al. 2021). This study included a total of 17 patients with a hopeless single-rooted tooth. After minimally traumatic tooth extraction, all the sites presented with severe buccal bone dehiscence defects (5.76+4.23 mm). The defect sockets were reconstructed using a particulate bone allograft material and a non-resorbable dPTFE membrane. All sites were evaluated with a panel of clinical, dimensional, volumetric, implant-related, histomorphometric, and patient-reported outcome measures. Uneventful wound healing was observed in all patients. An increase of 5.66+5.1 mm in mid-buccal bone height was detected radiographically from baseline to 20 weeks. Similarly, a total gain of 9.12 % in alveolar bone volume and a reduction of 10.83 % in the soft tissue contour were observed. The histomorphometric analyses revealed a mean area of mineralized tissue of 31.04 %+15.22 %, residual biomaterial particles of 16.23 %+10.63 %, and non-mineralized tissue of 52.71 %+9.53 %. All the implants were placed in a prosthetically and anatomically favorable location, and 47% of sites required additional bone augmentation procedures at the time of implant placement. Finally, the average discomfort scores were low and decreased over time, and the patients were generally very satisfied with a patient-reported satisfaction level of 95.1/100 (Antonious et al. 2021).
Clinical presentation
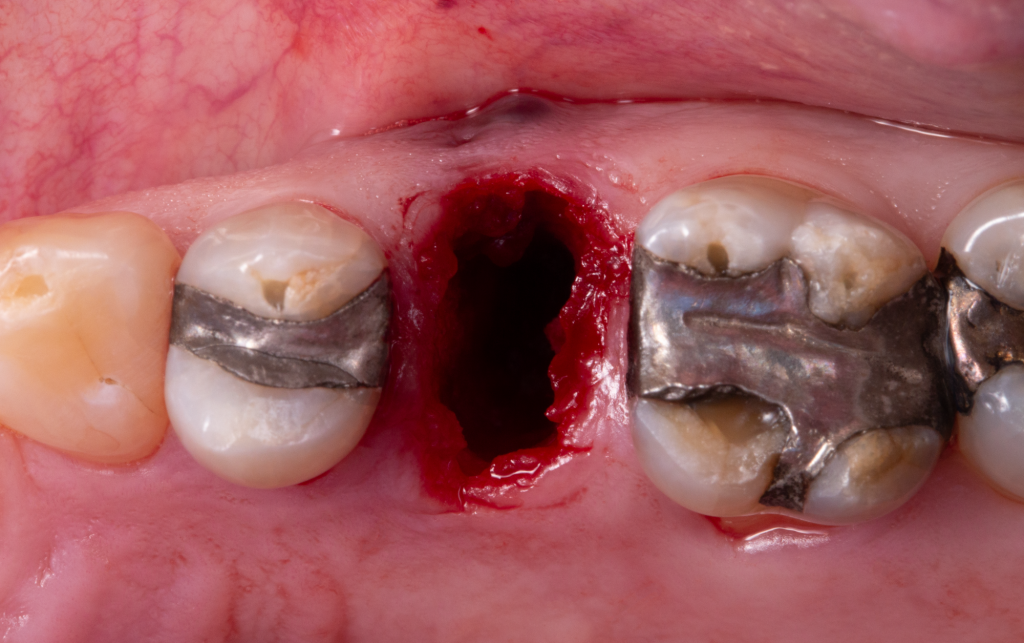
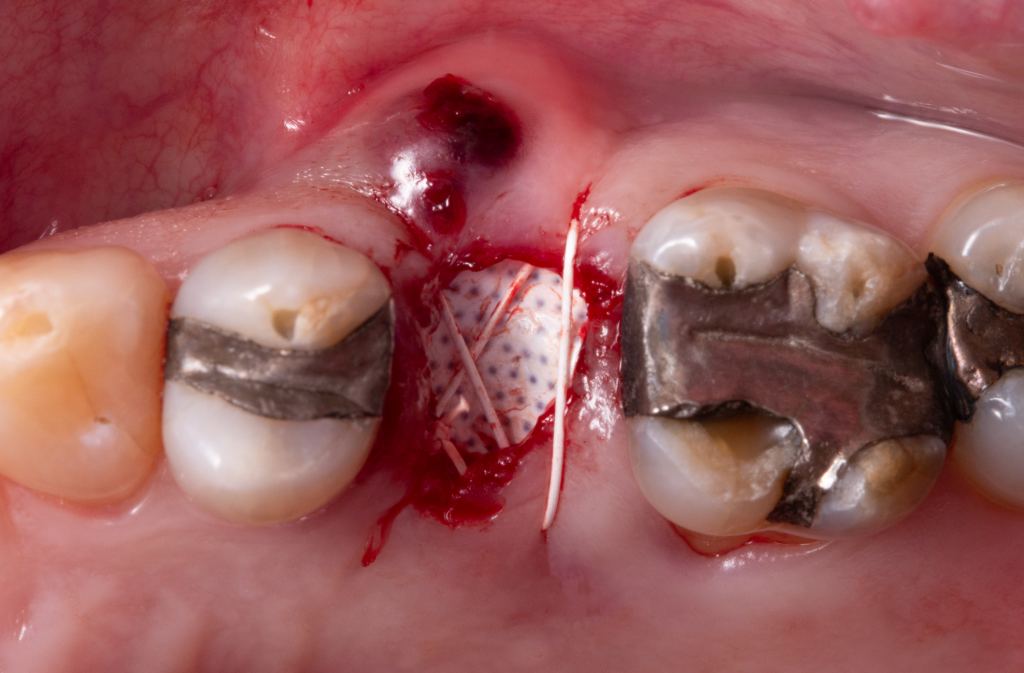
A systemically healthy 65-year-old man presented to the Department of Periodontology at the University of Iowa seeking treatment of a maxillary second premolar tooth (FDI system: #25), referred by the Department of Endodontics from the same university. The tooth had been endodontically treated more than 15 years ago, restored with a post and core and a full porcelain-fused-to-metal crown. During the clinical exam, a sinus tract at the facial aspect was detected as shown in Figure 1. Deep probing depth localized at the facial aspect (> 11mm) as exhibited in Figure 2A and bleeding and suppuration on probing, with mobility grade I were observed. Therefore, an endo-periodontal lesion in a non-periodontitis patient with root damage (possible root fracture or cracking) was diagnosed. Due to clinical and radiographic evidence of a possible vertical root fracture, the tooth was considered hopeless. Different alternative treatment options were discussed with the patient. Finally, the patient selected a treatment plan involving the replacement of the future missing tooth with a dental implant. Baseline clinical and radiographic views are depicted in Figure 1.
Case management
Alveolar ridge reconstruction procedure
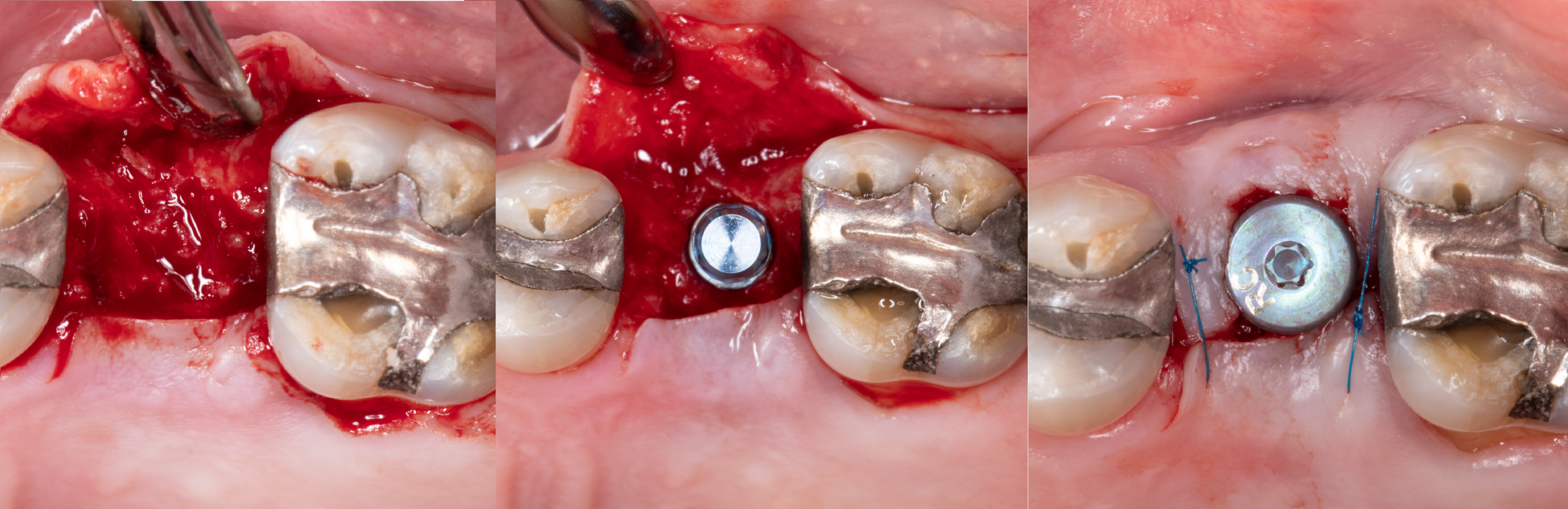
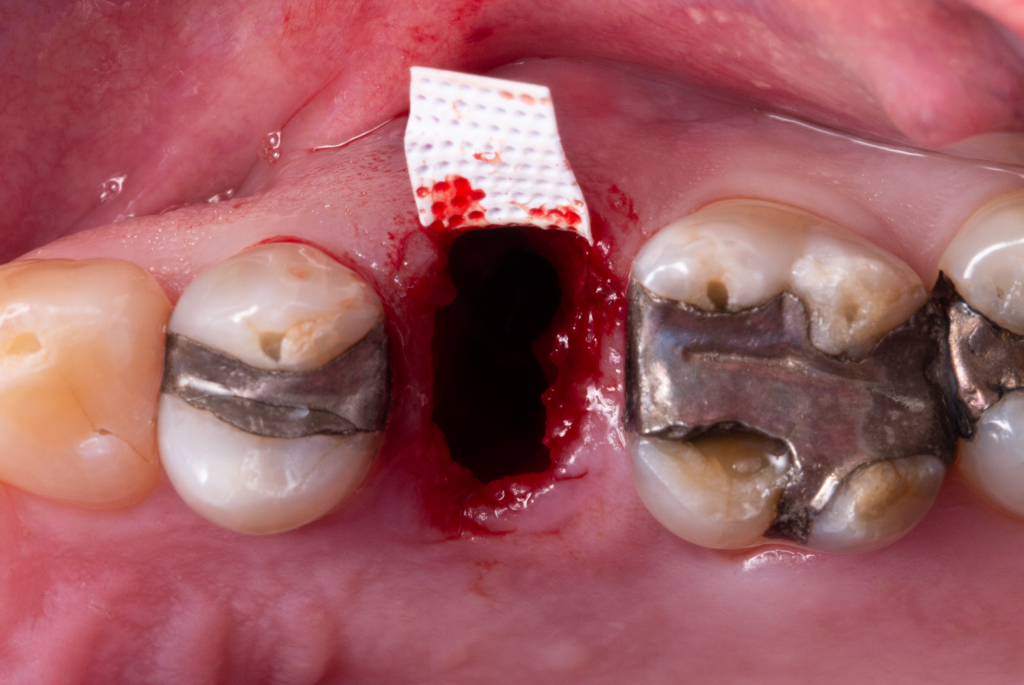
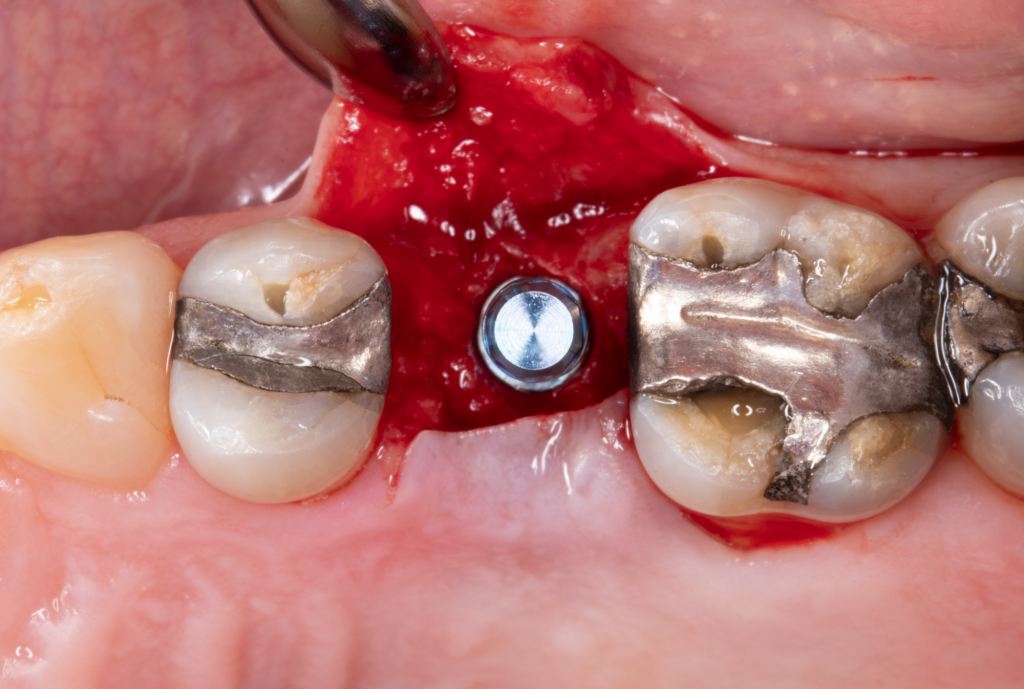
1. Once local anesthesia was achieved, tooth extraction was completed in a minimally traumatic, flapless fashion (Fig. 2C).
2. A dehiscence defect and the suspected vertical root fracture were confirmed clinically before and after extraction.
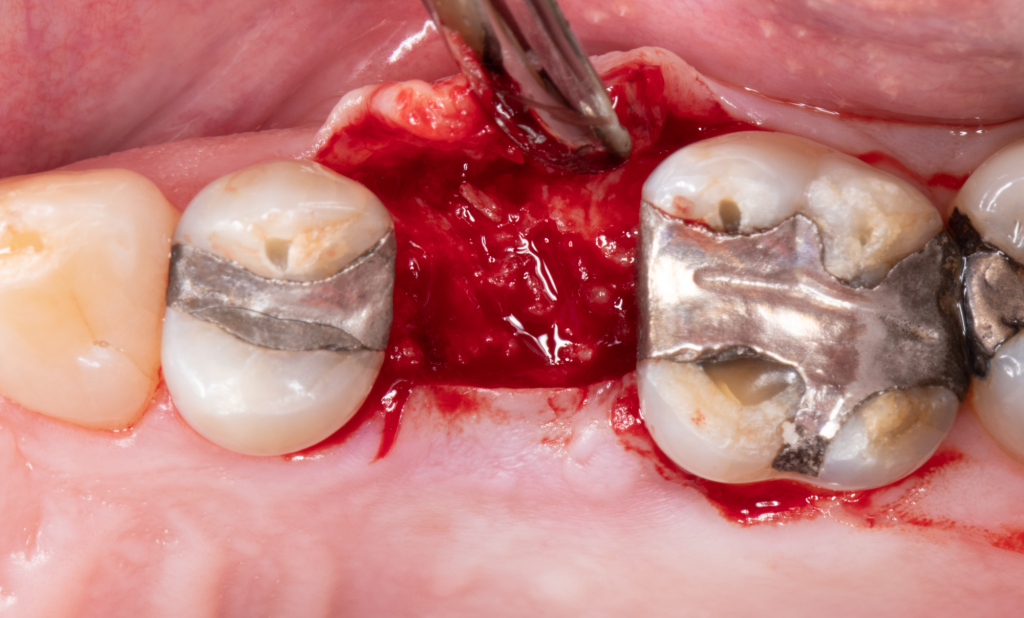
3. After gentle curetting to eliminate the granulomatous tissue, a full-thickness mucoperiosteal flap was created using tunneling instruments around the dehiscence bone defect and at the palatal site.
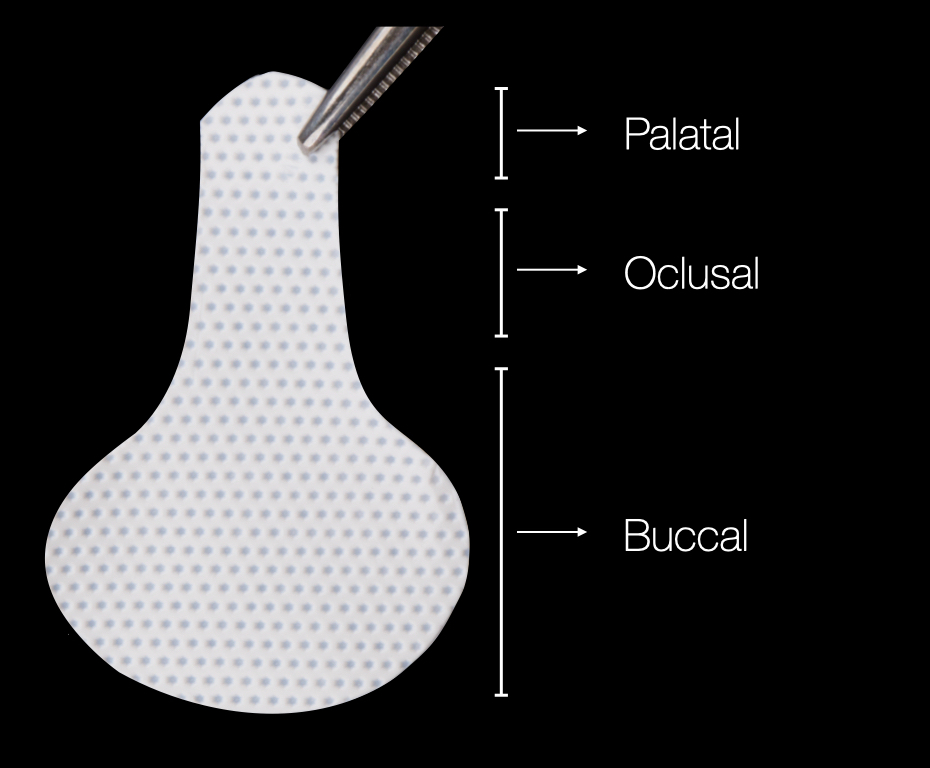
4. A non-resorbable dPTFE membrane (Cytoplast TXT-200, Osteogenic Biomedical) was trimmed to an appropriate size and shape allowing complete extension over the defect (Fig. 2D).
5. The trimmed dPTFE membrane was tucked between the facial mucoperiostal flap and the alveolar bone (Fig. 2E).
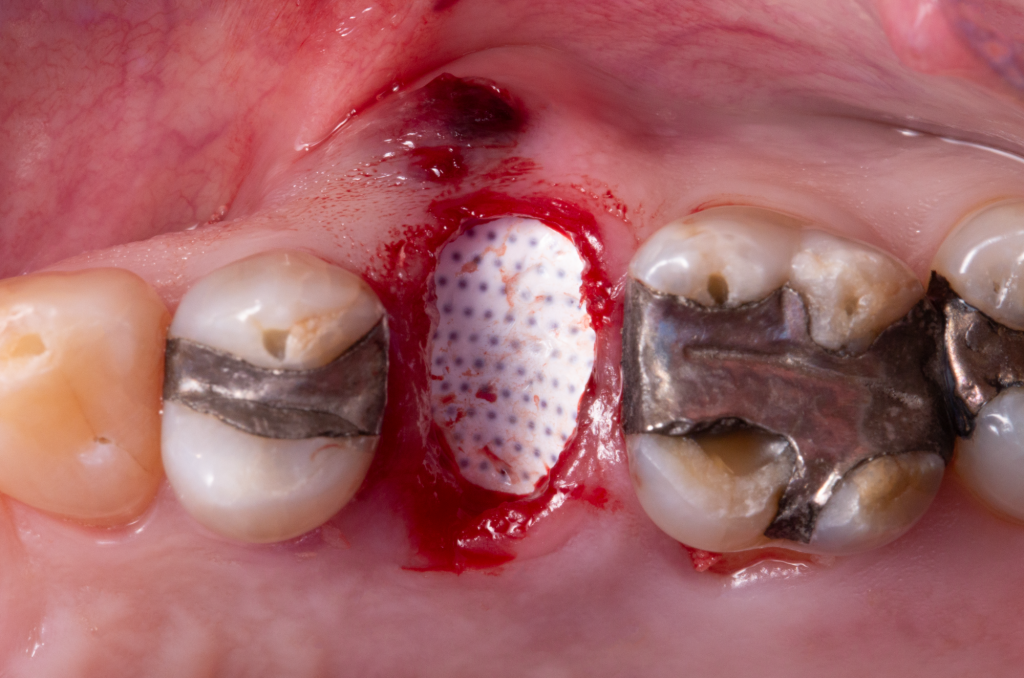
6. A cancellous particulate bone allograft (Puros, Zimmer Biomet) was utilized to fill the alveolar socket to the crestal level and over-contour the buccal bone housing (Figs 2F – 2G).
7. The socket was sealed with the dPTFE membrane and was tucked between the palatal mucosa and the alveolar bone. This ensures compartmentalization of the underlying bone grafting material and alveolar bone (Fig. 2H).
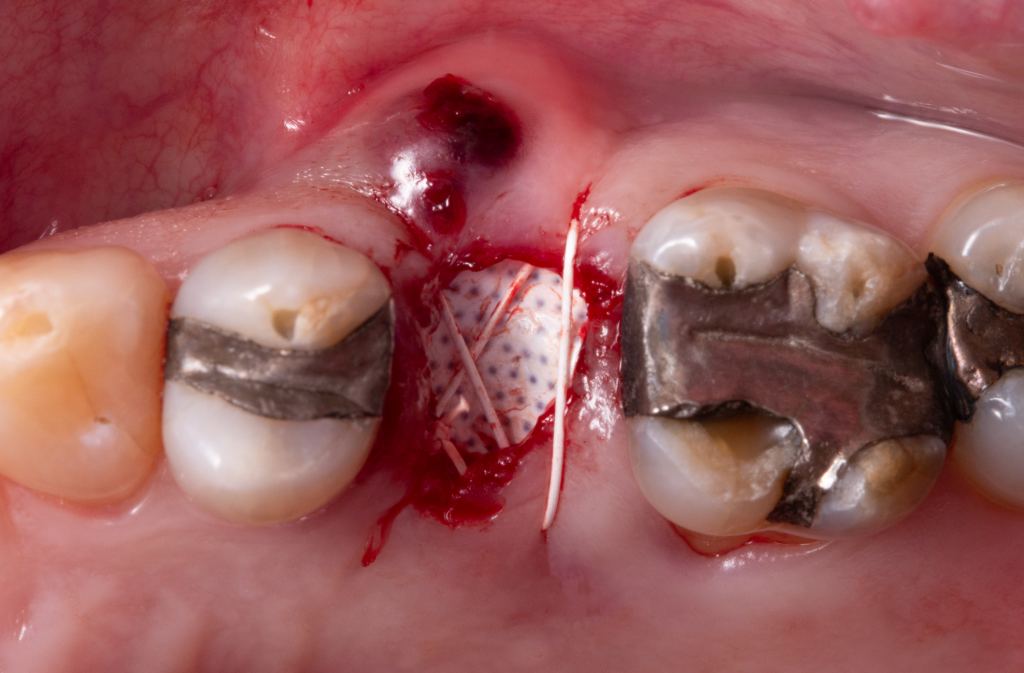
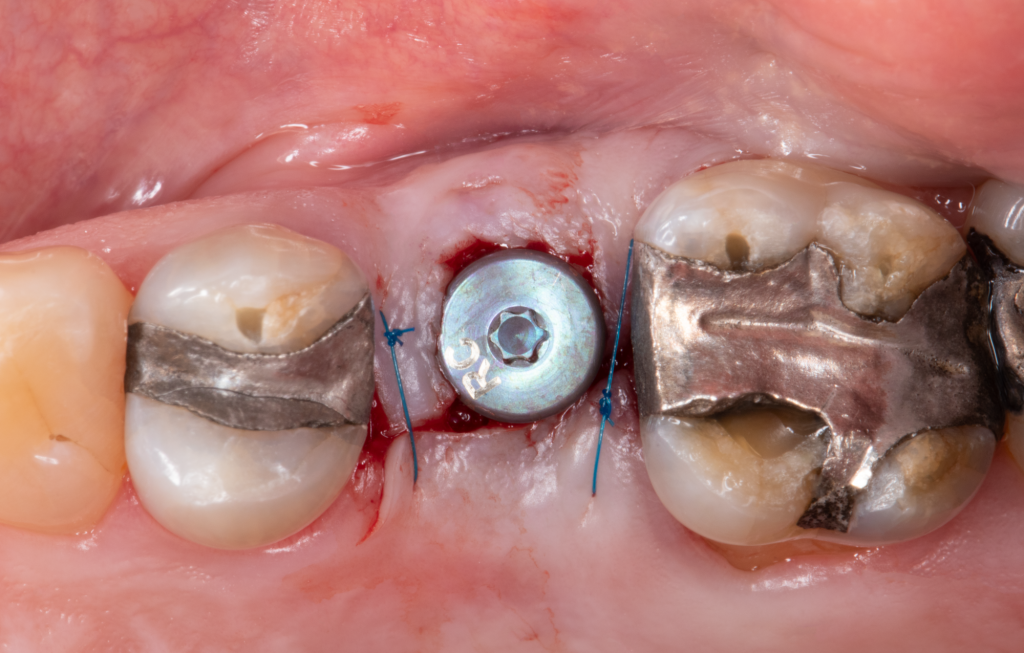
8. An external cross-mattress suture utilizing a non-absorbable suture was made (Cytoplast 5/0 suture, Osteogenic Biomedical), stabilizing the marginal mucosa (Fig. 2I).




The patient was instructed to avoid mechanical disturbance or excessive pressure on the surgical site and avoid brushing the area for the first 10 days. A chlorhexidine gluconate 0.12 % oral rinse was recommended to be used every 12 hours, and the patient was instructed to clean the membrane carefully with a cotton tip impregnated in the same antiseptic solution. Additionally, anti-inflammatory medication (600mg ibuprofen every 6 to 8 hours for the next 2 days, then as needed), and a systemic antibiotic (500mg amoxicillin every 8 hours for 7 days) were prescribed.
Post-operative visits
1. Ten days after the surgical intervention. Uneventful healing was observed, and the suture was removed (Fig. 3A). The patient was instructed to clean the area with a soft-bristle toothbrush and a cotton tip impregnated in chlorhexidine solution to avoid excessive pressure on the surgical site.


2. At around 5 weeks the non-resorbable membrane was retrieved without local anesthesia utilizing cotton forceps.
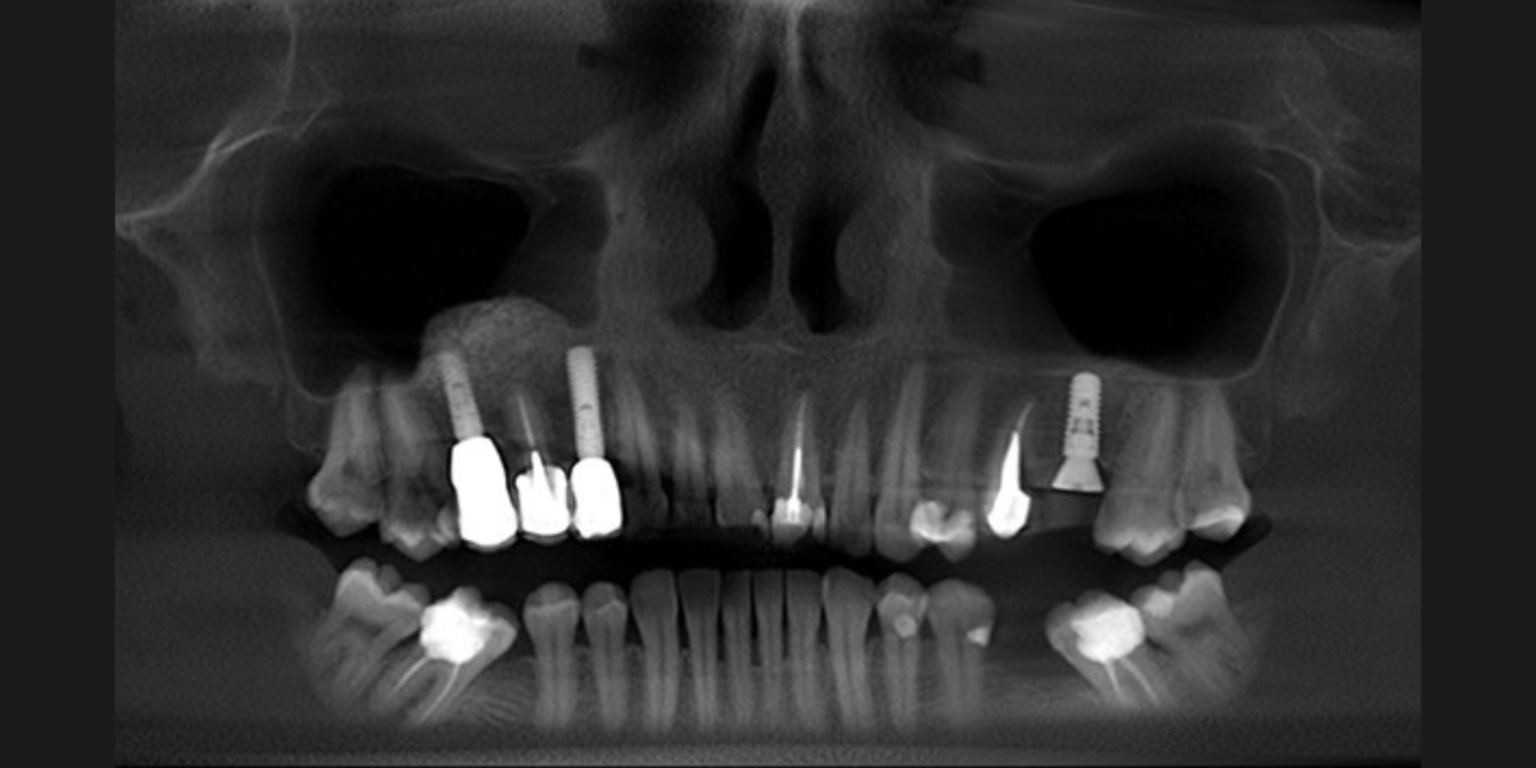
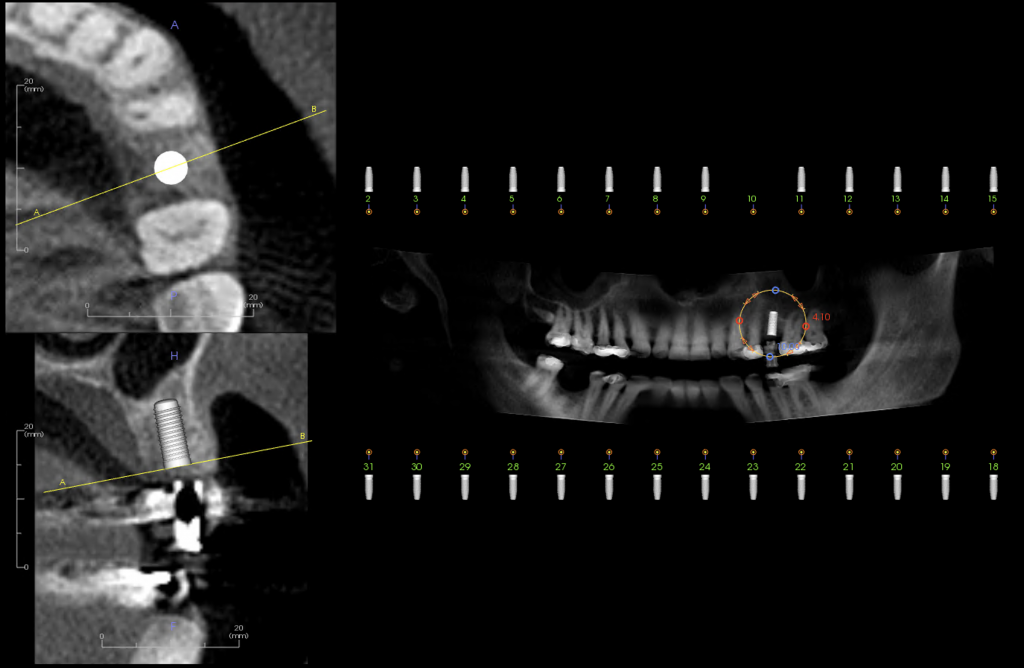
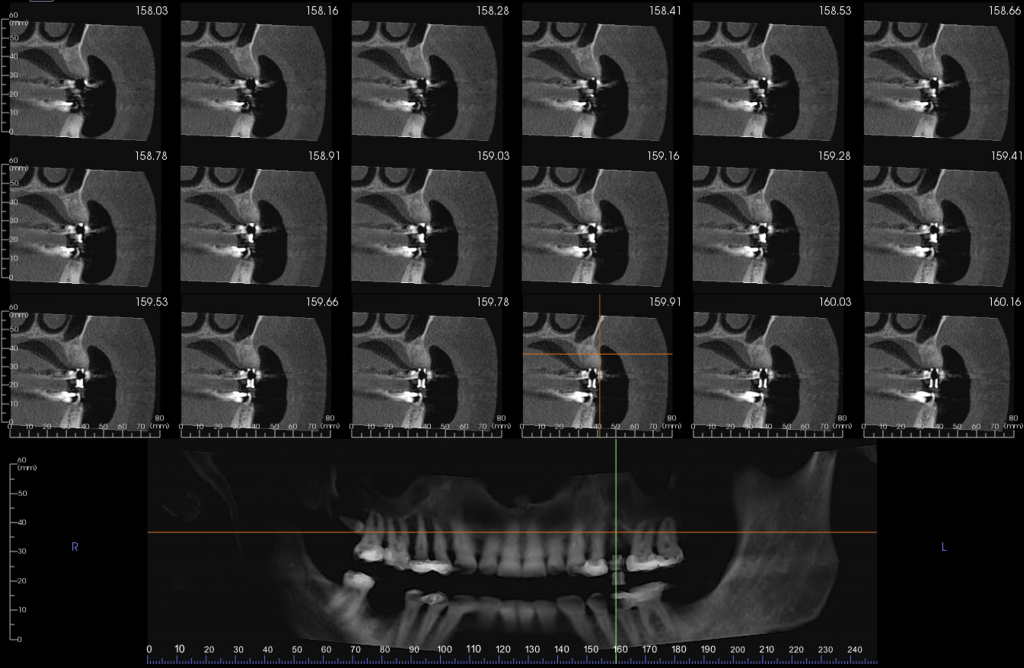
3. At 6 months a cone beam computed tomography (CBCT) scan was obtained to evaluate the alveolar ridge reconstruction procedure and plan the future implant placement. Adequate bone volume for placing the implant in a prosthetically and anatomically favorable location was observed (Fig. 4).
Implant placement
1. Eight months after the alveolar ridge reconstruction, a paracrestal incision within the keratinized mucosa was made towards the palatal site followed by an intrasulcular incision up to the mid-facial and mid-lingual sites of the adjacent teeth. A full-thickness flap elevation was subsequently performed (Figs 5A – 5B).
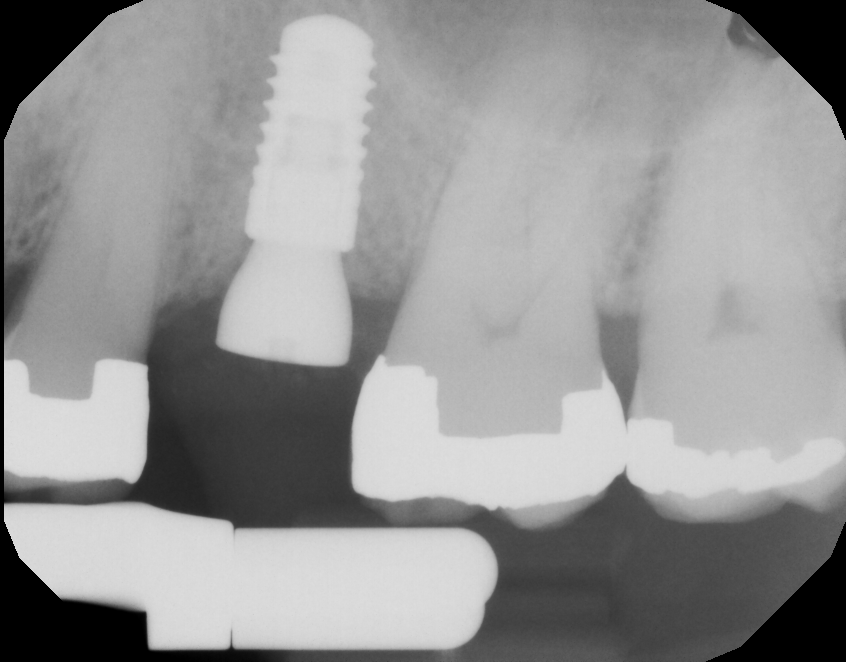
2. Implant site preparation and placement were completed following the manufacturer’s recommendation. A bone-level implant (4.1×10 mm with a parallel-walled endosteal design, SLActive Bone Level, Straumann) was placed (Fig. 5C).
3. Simultaneous bone/soft tissue augmentation was deemed not necessarily due to the local phenotypic characteristics of the site (Avila-Ortiz et al. 2020). Finally, after implant placement, the circumferential bone around the implant was >1.5 mm (Fig. 5C).
4. A healing abutment was placed, the facial mucosa was trimmed, and the flap was reapproximated with two single interrupted sutures utilizing a non-absorbable suture (Resolon 6/0 suture, Resorba) (Fig. 5D).
5. An intraoral periapical radiograph was taken to verify adequate implant position (Fig. 5E).

Postoperative instructions were given to the patient. Anti-inflammatory medication (600mg ibuprofen every 6 to 8 hours for the next two days), was recommended and no systemic antibiotic was prescribed.
Follow-up visits
1. Three months after implant placement, and when osseointegration had been achieved, the process of implant-supported crown planning and fabrication was initiated.
2. The final implant-supported restoration made of full zirconia was inserted 4.5 months after implant placement.
3. Periodontal and implant supportive therapy was provided to the patient every 6 months to monitor oral hygiene and peri-implant tissue health.
Final follow-up
Eighteen months after the delivery of the implant-supported restoration, clinical and radiographic exams were performed as shown in Figure 6. Peri-implant marginal bone level changes were negligible, indicating the stability of the bone substrate and successful implant integration. Clinically, probing depths were <4 mm, there was no clinically visible inflammation of the mucosa or suppuration, adequate keratinized mucosal width was present, and the patient did not report any pain or discomfort. The patient reported high esthetic and functional satisfaction. The comparison between the initial clinical situation before tooth extraction and the clinical aspect of the reconstruction and restorative outcomes 18 months after delivery of the final implant-supported restoration is shown in Figure 7.









Conclusion
This minimally invasive approach for managing a post-extraction dehiscence defect demonstrated an effective and predictable treatment option for reconstructing the alveolar ridge at the time of tooth extraction. This ultimately helped to provide an adequate ridge volume for implant placement, avoiding the need for further bone augmentation procedures.